Abstract
Introduction and hypothesis
Limited existing evidence suggests that there is a high prevalence of female pelvic organ prolapse (POP) amongst Nepali women. However, to date, no comprehensive assessment of pelvic floor functional anatomy has been undertaken in this population. Our study aimed to determine functional pelvic floor anatomy in Nepali women attending a general gynaecology clinic.
Methods
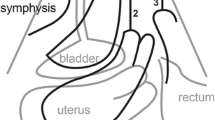
One hundred and twenty-nine consecutive women attending the clinic were offered an interview, clinical examination [International Continence Society Pelvic Organ Prolapse Quantification system (ICS/POP-Q)] and 4D translabial ultrasound (TLUS). Most presented with general gynaecological complaints. Five were excluded due to previous pelvic surgery, leaving 124.
Results
A POP-Q exam was possible in 123 women, of whom 29 (24%) were diagnosed with a significant cystocele, 50 (41%) significant uterine prolapse and seven (6%) significant posterior compartment prolapse. Evaluation of 4D TLUS data sets was possible in 120 women, of whom 25 (21%) had a significant cystocele, 45 (38%) significant uterine prolapse and ten (8%) significant descent of the rectal ampulla. In 13 cases, there was a rectocele with a mean depth of 14 (10–28) mm. Of 114 women in whom uterine position could be determined, 68 (60%) had a retroverted uterus associated with significant uterine prolapse (P 0.038).
Conclusions
POP is common in Nepali women attending a general gynaecology clinic, with a high prevalence of uterine prolapse (40%). Uterine retroversion was seen in 60% and was associated with uterine prolapse. Patterns of POP in Nepal seem to be different from patterns observed in Western populations.


Similar content being viewed by others
Abbreviations
- ICS/POP-Q:
-
International Continence Society, Pelvic Organ Prolapse Quantification system
- TLUS:
-
4D Translabial ultrasound
- POP:
-
Pelvic organ prolapse
- VAS:
-
Visual analogue scale
- PFM:
-
Pelvic floor muscle
- PFMC:
-
Pelvic floor muscle contraction
- LAM:
-
Levator ani muscle
- EAS:
-
External anal sphincter
- SP:
-
Symphysis pubis
- COPD:
-
Chronic obstructive pulmonary disease
References
Dietz HP, Franco AV, Shek KL, Kirby A. Avulsion injury and levator hiatal ballooning: two independent risk factors for prolapse? An observational study. Acta Obstet Gynecol Scand. 2012;91(2):211–4.
Bump RC, Norton PA. Epidemiology and natural history of pelvic floor dysfunction. Obstet Gynecol Clin N Am. 1998;25(4):723–46.
Smith FJ, Holman CA, Moorin RE, Tsokos N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010;116(5):1096–100.
Whitcomb EL, Rortveit G, Brown JS, Creasman JM, Thom DH, Van Den Eeden SK, et al. Racial differences in pelvic organ prolapse. Obstet Gynecol. 2009;114(6):1271.
Abdool Z, Dietz HP, Lindeque BG. Ethnic differences in the levator hiatus and pelvic organ descent: a prospective observational study. Ultrasound Obstet Gynecol. 2017;50(2):242–6.
Cheung RY, Shek KL, Chan SS, Chung TK, Dietz HP. Pelvic floor muscle biometry and pelvic organ mobility in east Asian and Caucasian nulliparae. Ultrasound Obstet Gynecol. 2015;45(5):599–604.
Shek KL, Krause HG, Wong V, Goh J, Dietz HPI. Pelvic organ support different between young nulliparous African and Caucasian women? Ultrasound Obstet Gynecol. 2016;47(6):774–8.
Center for Agro-Ecology and Development (CAED) (2006) Uterine prolapse widespread. Post Report. Nepal. Available from: http://www.advocacynet.org/partners_archive/womens-reproductive-rights-program/
Bonetti TR, Erpelding A, Pathak LR. Listening to “felt needs”: investigating genital prolapse in western Nepal. Reprod health matters. 2004;12(23):166–75.
Subba B, Adhikari D, Bhattarai T. The neglected case of the fallen womb. Nepal: Himal South Asian; 2003.
Gurung G, Rana A, Amatya A, Bista KD, Joshi AB, Sayami J. Pelvic organ prolapse in rural Nepalese women of reproductive age groups: what makes it so common? Nepal J Obstet Gynaecol. 2007;2(2):35–41.
Haylen BT, McNALLY G, Ramsay P, Birrell W, Logan VA. Standardised ultrasonic diagnosis and an accurate prevalence for the retroverted uterus in general gynaecology patients. Aust NZ J Obstet Gynaecol. 2007;47(4):326–8.
Haylen BT. The retroverted uterus: ignored to date but core to prolapse. Int Urogynecol J. 2006;17(6):555.
Ulrich D, Guzman Rojas R, Dietz HP, Mann K, Trutnovsky G. Use of a visual analog scale for evaluation of bother from pelvic organ prolapse. Ultrasound Obstet Gynecol. 2014;43(6):693–7.
Dietz HP, Shek C. Validity and reproducibility of the digital detection of levator trauma. Int Urogynecol J. 2008;19(8):1097–101.
Dietz HP, Mann KP. What is clinically relevant prolapse? An attempt at defining cutoffs for the clinical assessment of pelvic organ descent. Int Urogynecol J. 2014;25(4):451–5.
Dietz HP, Lekskulchai O. Ultrasound assessment of pelvic organ prolapse: the relationship between prolapse severity and symptoms. Ultrasound Obstet Gynecol. 2007;29(6):688–91.
Shek KL, Dietz HP. What is abnormal uterine descent on translabial ultrasound? Int Urogynecol J. 2015;26(12):1783–7.
Chan SS, Cheung RY, Yiu KW, Lee LL, Leung TY, Chung TK. Pelvic floor biometry during a first singleton pregnancy and the relationship with symptoms of pelvic floor disorders: a prospective observational study. BJOG. 2014;121(1):121–9.
Dietz HP, Moegni F, Shek KL. Diagnosis of levator avulsion injury: a comparison of three methods. Ultrasound Obstet Gynecol. 2012;40(6):693–8.
Lien YS, Chen GD, Ng SC. Prevalence of and risk factors for pelvic organ prolapse and lower urinary tract symptoms among women in rural Nepal. Int J Gynecol Obstet. 2012;119(2):185–8.
Bodner-Adler B, Shrivastava C, Bodner K. Risk factors for uterine prolapse in Nepal. Int Urogynecol J. 2007;18(11):1343–6.
Thapa S, Angdembe M, Chauhan D, Joshi R. Determinants of pelvic organ prolapse among the women of the western part of Nepal: a case–control study. J Obstet Gynecol Research. 2014;40(2):515–20.
Swift S, Woodman P, O’boyle A, Kahn M, Valley M, Bland D, et al. Pelvic organ support study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol. 2005;192(3):795–806.
Dietz HP, Simpson JM. Levator trauma is associated with pelvic organ prolapse. BJOG. 2008;115(8):979–84.
Dhital R, Otsuka K, Poudel KC, Yasuoka J, Dangal G, Jimba M. Improved quality of life after surgery for pelvic organ prolapse in Nepalese women. BMC Womens Health. 2013;13(1):22.
Sah DK, Doshi NR, Das CR. Vaginal hysterectomy for pelvic organ prolapse in Nepal. Kathmandu University Medical J. 2010;8(2):281–4.
Pixton S, Caudwell Hall J, Turel F, Dietz HP. Predictors of ring pessary success in women with pelvic organ prolapse. Int Urogynecol J. 2017; in print.
Fernando RJ, Thakar R, Sultan AH, Shah SM, Jones PW. Effect of vaginal pessaries on symptoms associated with pelvic organ prolapse. Obstet Gynecol. 2006;108(1):93–9.
Acknowledgements
The authors thank the women who participated in this study. We also thank staff at Kathmandu Model Hospital for their assistance and generosity with their limited space. We are especially grateful to Dr. Vishal Kumar Trivedi for excellent assistance during data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
H.P. Dietz has received unrestricted educational grants from GE Medical. F. Turel and D. Caagbay have no conflict of interest to declare.
Rights and permissions
About this article
Cite this article
Turel, F., Caagbay, D. & Dietz, H.P. Functional pelvic floor anatomy in Nepali women attending a general gynaecology clinic. Int Urogynecol J 29, 1435–1440 (2018). https://doi.org/10.1007/s00192-017-3534-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-017-3534-x