Abstract
Introduction and hypothesis
The standardized evaluation of posterior compartment prolapse using the Pelvic Organ Prolapse Quantification (POP-Q) system is limited. The primary objective of this study is to develop and validate the interexaminer reliability of a new system for assessing the posterior vaginal wall for the presence of a rectocele.
Methods
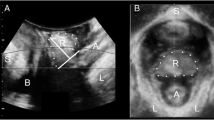
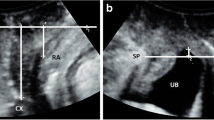
This was a cross-sectional study of women presenting to an academic urogynecology clinic. Subjects underwent a routine pelvic examination that included a standard POP-Q followed by two Standardized Digital Rectal Exams (SDRE) by two different providers, each blinded to the other’s results. The SDRE measures the distance from the leading edge of a posterior bulge to the hymen with a finger in the distal rectum - first visually and then an actual measured distance using a marked cotton swab (Q-tip measurement). Correlations between examiners for the SDRE and the POP-Q were analyzed using Pearson's correlation coefficient (ρ).
Results
Eight attending and fellow urogynecologists examined 50 subjects. Mean age was 57.3 years, mean BMI 30.9 kg/m2, with an overall median POP-Q stage 2 (range 0–3), and median posterior POP-Q stage 1 (range 0–3). Overall, 54 % of women had a noteworthy rectocele by typical digital rectal exam. Interexaminer correlations with SDRE for both the visual assessment (ρ = 0.697, p < 0.0001) and the Q-tip measurement (ρ = 0.767, p = p < 0.001) were strong. The intraexaminer visual assessment and the Q-tip measurement were highly correlated (ρ = 0.934, p = <0.001).
Conclusion
This standardized rectal examination provides a consistent method for the reporting of distal rectoceles that can lend additional information to the POP-Q exam.


Similar content being viewed by others
References
Bump RC, Mattiasson, Bo K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Hall AF, Theofrastous JP, Cundiff GW, Harris RL, Hamilton LF, Swift SE, Bump RC (1996) Interobserver and intraobserver reliability of the International Continence Society, Society of Gynecologic Surgeons, and American Urogynecologic Society pelvic organ prolapse classification system. Am J Obstet Gynecol 1467–71.
Kobak WH, Rosenberger K, Walters MD (1996) Interobserver variation in the assessment of pelvic organ prolapse. Int Urogynecol J 7:121–124
Zoorob D, Sanan CC, Evans JM, Maxwell R, South M (2012) A retrospective comparison of defecatory symptoms in subjects with a posterior vaginal wall defect identified by POP-Q scores versus digital rectal exam. Female Pelvic Med Reconstr Surg 18:S116
Weber AM, Walters MD, Ballard LA, Booher DL, Piedmonte MR (1998) Posterior vaginal prolapse and bowel function. Am J Obstet Gynecol 179:1446–1449
Ellerkmann RM, Cundiff GW, Melick CF, Nihira MA, Leffler K, Bent AE (2001) Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol 185:1332–1337
Bradley CS, Brown MB, Cundiff GW, Goode PS, Kenton KS, Nygaard IE, Whitehead WE, Wren PA, Weber AM (2006) Bowel symptoms in women planning surgery for pelvic organ prolapse. Am J Obstet Gynecol 195:1814–1819
Chmielewski L, Walters MD, Weber AM, Barber MD (2011) Reanalysis of a randomized trial of three techniques of anterior colporraphy using clinically relevant definitions of success. Am J Obstet Gynecol 205:69.e1–69.e8
Barber MD, Walters MD, Bump RC (2005) Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol 193:103–113
Lewis SJ, Heaton KW (1997) Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol 32:920–924
Spence-Jones C, Kamm MA, Henry MM, Hudson CN (1994) Bowel dysfunction: a pathogenic factor in uterovaginal prolapse and urinary stress incontinence. Br J Obstet Gynaecol 101:147–152
Cundiff GW, Fenner D (2004) Evaluation and treatment of women with rectocele: focus on associated defecatory and sexual dysfunction. Obstet Gynecol 104:1403–1421
Kahn MA, Breitkopf CR, Valley MT, Woodman PJ, O'Boyle AL, Bland DI, Schaffer JI, Grady JJ, Swift SE (2005) Pelvic organ support study (POSST) and bowel symptoms: staining at stool is associated with perineal and anterior vaginal descent in a general gynecologic population. Am J Obstet Gynecol 192:1516–1522
Mouritsen L, Larsen JP (2003) Symptoms, bother, and POP-Q in women referred with pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct 14:122–127
Acknowledgements
We would like to thank Mr. Yilan Xu and Dr. J.S. Marron of the Department of Statistics and Operations Research at the University of North Carolina at Chapel Hill for their statistical support.
Conflicts of interest
Matthews CA and Geller EJ: Robotics fellowship grant from Intuitive Surgical.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Crane, A.K., Geller, E.J., Myers, E.M. et al. Implementation of a standardized digital rectal exam to improve the accuracy of rectocele diagnosis. Int Urogynecol J 26, 107–111 (2015). https://doi.org/10.1007/s00192-014-2479-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2479-6