Abstract
Purpose
To evaluate the relationship between posterior tibial slope (PTS), posterior condylar offset (PCO), femoral sagittal angle (FSA) on clinical outcomes, and propose optimal sagittal plane alignments for unicompartmental knee arthroplasty (UKA).
Methods
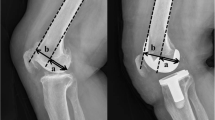
Prospectively collected data of 265 medial UKA was analysed. PTS, PCO, FSA were measured on preoperative and postoperative lateral radiographs. Clinical assessment was done at 6-month, 2-year and 10-year using Oxford Knee Score, Knee Society Knee and Function scores, Short Form-36, range of motion (ROM), fulfilment of satisfaction and expectations. Implant survivorship was noted at mean 15-year. Kendall rank correlation test evaluated correlations of sagittal parameters against clinical outcomes. Multivariable linear regression evaluated predictors of postoperative ROM. Effect plots and interaction plots were used to identify angles with the best outcomes. (p < 0.05) was the threshold for statistical significance.
Results
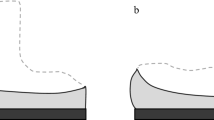
There were significant correlations between PTS, PCO and FSA. Younger age, lower BMI, implant type, greater preoperative flexion, steeper PTS and preservation of PCO were significant predictors of greater postoperative flexion. There were significant interaction effects between PTS and PCO. Effect plots demonstrate a PTS between 2° to 8° and restoration of PCO within 1.5 mm of native values are optimal for better postoperative flexion. Interaction plot reveals that it is preferable to reduce PCO by 1.0 mm when PTS is 2° and restore PCO at 0 mm when PTS is 8°.
Conclusion
UKA surgeons and future studies should be mindful of the relationship between PTS, PCO and FSA, and avoid considering them in isolation. When deciding on the method of balancing component gaps in UKA, surgeons should rely on the PTS. Decrease the posterior condylar cut when PTS is steep, and increase the posterior condylar cut when PTS is shallow. The acceptable range for PTS is between 2° to 8° and PCO should be restored to 1.5 mm of native values.
Level of evidence
II.






Similar content being viewed by others
References
Adulkasem N, Rojanasthien S, Siripocaratana N, Limmahakhun S (2019) Posterior tibial slope modification in osteoarthritis knees with different ACL conditions: cadaveric study of fixed-bearing UKA. J Orthop Surg (Hong Kong) 27:2309499019836286
Aleto TJ, Berend ME, Ritter MA, Faris PM, Meneghini RM (2008) Early failure of unicompartmental knee arthroplasty leading to revision. J Arthroplasty 23:159–163
Andriacchi TP, Galante JO, Fermier RW (1982) The influence of total knee-replacement design on walking and stair-climbing. J Bone Joint Surg Am 64:1328–1335
Bell SW, Anthony I, Jones B, MacLean A, Rowe P, Blyth M (2016) Improved accuracy of component positioning with robotic-assisted unicompartmental knee arthroplasty: data from a prospective, randomized controlled study. J Bone Joint Surg Am 98:627–635
Berend KR, Lombardi AV Jr, Mallory TH, Adams JB, Groseth KL (2005) Early failure of minimally invasive unicompartmental knee arthroplasty is associated with obesity. Clin Orthop Relat Res 440:60–66
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63
Bruni D, Gagliardi M, Akkawi I, Raspugli GF, Bignozzi S, Marko T et al (2016) Good survivorship of all-polyethylene tibial component UKA at long-term follow-up. Knee Surg Sports Traumatol Arthrosc 24:182–187
Cho KY, Kim KI, Song SJ, Kim KJ (2018) Intentionally increased flexion angle of the femoral component in mobile bearing unicompartmental knee arthroplasty. Knee Surg Relat Res 30:23–27
Cinotti G, Sessa P, Ripani FR, Postacchini R, Masciangelo R, Giannicola G (2012) Correlation between posterior offset of femoral condyles and sagittal slope of the tibial plateau. J Anat 221:452–458
Flury A, Hasler J, Dimitriou D, Antoniadis A, Finsterwald M, Helmy N (2019) Midterm clinical and radiographic outcomes of 115 consecutive patient-specific unicompartmental knee arthroplasties. Knee 26:889–896
Gaudiani MA, Nwachukwu BU, Baviskar JV, Sharma M, Ranawat AS (2017) Optimization of sagittal and coronal planes with robotic-assisted unicompartmental knee arthroplasty. Knee 24:837–843
Han HS, Kang SB (2018) Interactive effect of femoral posterior condylar offset and tibial posterior slope on knee flexion in posterior cruciate ligament-substituting total knee arthroplasty. Knee 25:335–340
Harbourne AD, Sanchez-Santos MT, Arden NK, Filbay SR (2019) Predictors of return to desired activity 12 months following unicompartmental and total knee arthroplasty. Acta Orthop 90:74–80
Horsager K, Kaptein BL, Rømer L, Jørgensen PB, Stilling M (2017) Dynamic RSA for the evaluation of inducible micromotion of Oxford UKA during step-up and step-down motion. Acta Orthop 88:275–281
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Inui H, Taketomi S, Yamagami R, Kawaguchi K, Nakazato K, Tanaka S (2020) Necessary factors to achieve deep flexion for Asian populations after Oxford unicompartmental knee arthroplasty. J Knee Surg 33:294–300
Jiang L, Chen JY, Chong HC, Chia SL, Lo NN, Yeo SJ (2016) Early outcomes of unicompartmental knee arthroplasty in patients with preoperative genu recurvatum of non-neurological origin. J Arthroplasty 31:1204–1207
Kaya Bicer E, Servien E, Lustig S, Demey G, Ait Si Selmi T, Neyret P (2010) Sagittal flexion angle of the femoral component in unicompartmental knee arthroplasty: is it same for both medial and lateral UKAs? Knee Surg Sports Traumatol Arthrosc 18:928–933
Kazarian GS, Barrack TN, Okafor L, Barrack RL, Nunley RM, Lawrie CM (2020) High prevalence of radiographic outliers and revisions with unicompartmental knee arthroplasty. J Bone Joint Surg Am 102:1151–1159
Kozinn SC, Scott R (1989) Unicondylar knee arthroplasty. J Bone Joint Surg Am 71:145–150
Kuipers BM, Kollen BJ, Bots PC, Burger BJ, van Raay JJ, Tulp NJ et al (2010) Factors associated with reduced early survival in the Oxford phase III medial unicompartment knee replacement. Knee 17:48–52
Kurosaka M, Yoshiya S, Mizuno K, Yamamoto T (2002) Maximizing flexion after total knee arthroplasty: the need and the pitfalls. J Arthroplasty 17:59–62
Lee M, Huang Y, Chong HC, Ning Y, Lo NN, Yeo SJ (2016) Predicting satisfaction for unicompartmental knee arthroplasty patients in an Asian population. J Arthroplasty 31:1706–1710
Lee SY, Bae JH, Kim JG, Jang KM, Shon WY, Kim KW et al (2014) The influence of surgical factors on dislocation of the meniscal bearing after Oxford medial unicompartmental knee replacement: a case-control study. Bone Joint J 96 b:914–922
Liow MH, Goh GS, Tay DK, Chia SL, Lo NN, Yeo SJ (2016) Obesity and the absence of trochlear dysplasia increase the risk of revision in patellofemoral arthroplasty. Knee 23:331–337
Lo Presti M, Raspugli GF, Reale D, Iacono F, Zaffagnini S, Filardo G et al (2019) Early failure in medial unicondylar arthroplasty: radiographic analysis on the importance of joint line restoration. J Knee Surg 32:860–865
Malviya A, Lingard EA, Weir DJ, Deehan DJ (2009) Predicting range of movement after knee replacement: the importance of posterior condylar offset and tibial slope. Knee Surg Sports Traumatol Arthrosc 17:491–498
Miner AL, Lingard EA, Wright EA, Sledge CB, Katz JN (2003) Knee range of motion after total knee arthroplasty: how important is this as an outcome measure? J Arthroplasty 18:286–294
Mulholland SJ, Wyss UP (2001) Activities of daily living in non-Western cultures: range of motion requirements for hip and knee joint implants. Int J Rehabil Res 24:191–198
Murray DW, Fitzpatrick R, Rogers K, Pandit H, Beard DJ, Carr AJ et al (2007) The use of the Oxford hip and knee scores. J Bone Joint Surg Br 89:1010–1014
Park KK, Han CD, Yang IH, Lee WS, Han JH, Kwon HM (2019) Robot-assisted unicompartmental knee arthroplasty can reduce radiologic outliers compared to conventional techniques. PLoS ONE 14:e0225941
Park KK, Koh YG, Park KM, Park JH, Kang KT (2019) Biomechanical effect with respect to the sagittal positioning of the femoral component in unicompartmental knee arthroplasty. Biomed Mater Eng 30:171–182
Polat AE, Polat B, Gürpinar T, Peker B, Tüzüner T (2020) Factors affecting the functional outcome of oxford phase 3 unicompartmental knee arthroplasty. Acta Ortop Bras 28:78–83
Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P et al (2011) Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 173:676–682
Ritter MA, Harty LD, Davis KE, Meding JB, Berend ME (2003) Predicting range of motion after total knee arthroplasty. Clustering, log-linear regression, and regression tree analysis. J Bone Joint Surg Am 85:1278–1285
Robinson BJ, Rees JL, Price AJ, Beard DJ, Murray DW, McLardy Smith P et al (2002) Dislocation of the bearing of the Oxford lateral unicompartmental arthroplasty. A radiological assessment. J Bone Joint Surg Br 84:653–657
Sekiguchi K, Nakamura S, Kuriyama S, Nishitani K, Ito H, Tanaka Y et al (2019) Effect of tibial component alignment on knee kinematics and ligament tension in medial unicompartmental knee arthroplasty. Bone Joint Res 8:126–135
Small SR, Berend ME, Rogge RD, Archer DB, Kingman AL, Ritter MA (2013) Tibial loading after UKA: evaluation of tibial slope, resection depth, medial shift and component rotation. J Arthroplasty 28:179–183
Suzuki T, Ryu K, Kojima K, Oikawa H, Saito S, Nagaoka M (2019) The effect of posterior tibial slope on joint gap and range of knee motion in mobile-bearing unicompartmental knee arthroplasty. J Arthroplasty 34:2909–2913
Takayama K, Matsumoto T, Muratsu H, Ishida K, Araki D, Matsushita T et al (2016) The influence of posterior tibial slope changes on joint gap and range of motion in unicompartmental knee arthroplasty. Knee 23:517–522
Tammachote N, Kriengburapha N, Chaiwuttisak A, Kanitnate S, Boontanapibul K (2018) Is Regular knee radiograph reliable enough to assess the knee prosthesis position? J Arthroplasty 33:3038–3042
Ueo T, Kihara Y, Ikeda N, Kawai J, Nakamura K, Hirokawa S (2011) Deep flexion-oriented bisurface-type knee joint and its tibial rotation that attributes its high performance of flexion. J Arthroplasty 26:476–482
Ware JE Jr, Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A (1995) Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care 33:As264-279
Weale AE, Halabi OA, Jones PW, White SH (2001) Perceptions of outcomes after unicompartmental and total knee replacements. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-200101000-00021143-153
Weber P, Schröder C, Schwiesau J, Utzschneider S, Steinbrück A, Pietschmann MF et al (2015) Increase in the tibial slope reduces wear after medial unicompartmental fixed-bearing arthroplasty of the knee. Biomed Res Int 2015:736826
Weber P, Woiczinski M, Steinbrück A, Schmidutz F, Niethammer T, Schröder C et al (2018) Increase in the tibial slope in unicondylar knee replacement: analysis of the effect on the kinematics and ligaments in a weight-bearing finite element model. Biomed Res Int 2018:8743604
World Medical Association (2013) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310:2191–2194
Xu S, Lim WJ, Chen JY, Lo NN, Chia SL, Tay DKJ et al (2019) The influence of obesity on clinical outcomes of fixed-bearing unicompartmental knee arthroplasty: a ten-year follow-up study. Bone Joint J 101-b:213–220
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
YZK (Medical Student): Conceptualization, Methodology, Validation, Statistical Analysis, Data Collection, Writing—Original Draft, Writing—Review and Editing. MHLL (Orthopaedic Surgeon): Conceptualization, Methodology, Writing—Original Draft, Writing—Review and Editing, Supervision. ML (Orthopaedic Surgeon): Validation. JYC (Orthopaedic Surgeon): Supervision. NNL (Orthopaedic Surgeon): Surgeon, Supervision. SJY (Orthopaedic Surgeon): Surgeon, Supervision.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
Yes.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khow, Y.Z., Liow, M.H.L., Lee, M. et al. Posterior condylar offset and posterior tibial slope targets to optimize knee flexion after unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 30, 822–831 (2022). https://doi.org/10.1007/s00167-021-06453-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06453-7