Abstract
Purpose
To systematically review the results of focal metallic inlay resurfacing prosthesis for the treatment of isolated cartilage defects of the femoral condyles.
Methods
A systematic electronic search of the PubMed database and the Cochrane Library was performed in April 2017 to identify studies that reported clinical or radiographic outcome of focal metallic inlay resurfacing prosthesis for the treatment of isolated cartilage defects of the femoral condyles. Included studies were abstracted regarding study characteristics, patient demographics, prosthetic device and location, indications and contraindications, and outcome measures. Outcome of interest included functional outcome scores, radiographic measures, complications, re-operations, and conversion to arthroplasty. The methodologic quality of the included studies was assessed with the Coleman Methodology Score.
Results
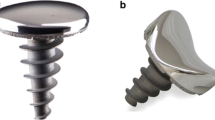
Six studies with a total of 186 patients met the inclusion criteria. Five studies were level IV evidence, and one was level III. The methodologic quality of the included studies was good, with a mean Coleman Methodology Score of 78. Two different implants were used: the HemiCAP® (five studies; 66% of study group) and UniCAP® (one study; 34%) implant. The mean age was 46–54 years, and the mean follow-up was 24 months to 7 years. Pre- and post-operative outcome scores were compared in all six studies, and five studies reported significant improvements at the final follow-up for all scores (objective und functional KSS, KOOS, WOMAC, Tegner, HSS Knee and Function score, SF-36 and SF-12 physical component score) except for the SF-36 and SF-12 mental component score. Progression of osteoarthritis was analysed using the Kellgren–Lawrence grading in three studies (30% of study group), with two studies reporting significant progression. The OARSI grading system was analysed in one study with no significant progression. The overall conversion rate to arthroplasty was 22% with considerable differences between the two implants: 9% for HemiCAP® and 47% for UniCAP®.
Conclusions
Focal metallic inlay resurfacing prosthesis seems to be a viable option for a carefully selected group of patients. Significant improvement in knee function and pain was observed in most patients. Uncertainty remains with regard to progression of osteoarthritis because of conflicting results and inconsistent reporting. One out of five patients has to be converted to arthroplasty after an average of 4 years. However, compared to the UniCAP® implant, considerable lower conversion rates were reported for the smaller HemiCAP® implant.
Level of evidence
Systematic review of level III and IV studies, Level IV.


Reprinted with permission from Arthrosurface, Inc., Franklin, MA
Similar content being viewed by others
References
Angele P, Madry H, Kon E (2016) Early OA: point of no return or a chance for regenerative approaches. Knee Surg Sports Traumatol Arthrosc 24(6):1741–1742
Angele P, Niemeyer P, Steinwachs M, Filardo G, Gomoll AH, Kon E, Zellner J, Madry H (2016) Chondral and osteochondral operative treatment in early osteoarthritis. Knee Surg Sports Traumatol Arthrosc 24(6):1743–1752
Becher C, Cantiller EB (2017) Focal articular prosthetic resurfacing for the treatment of full-thickness articular cartilage defects in the knee: 12-year follow-up of two cases and review of the literature. Arch Orthop Trauma Surg. doi:10.1007/s00402-017-2717-8
Becher C, Kalbe C, Thermann H, Paessler HH, Laprell H, Kaiser T, Fechner A, Bartsch S, Windhagen H, Ostermeier S (2011) Minimum 5-year results of focal articular prosthetic resurfacing for the treatment of full-thickness articular cartilage defects in the knee. Arch Orthop Trauma Surg 131(8):1135–1143
Bollars P, Bosquet M, Vandekerckhove B, Hardeman F, Bellemans J (2012) Prosthetic inlay resurfacing for the treatment of focal, full thickness cartilage defects of the femoral condyle: a bridge between biologics and conventional arthroplasty. Knee Surg Sports Traumatol Arthrosc 20(9):1753–1759
Brennan SA, Devitt BM, O’Neill CJ, Nicholson P (2013) Focal femoral condyle resurfacing. Bone Joint J 95-B(3):301–304
Buckwalter JA, Martin JA, Brown TD (2006) Perspectives on chondrocyte mechanobiology and osteoarthritis. Biorheology 43(3–4):603–609
Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD (2000) Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports 10(1):2–11
Curl WW, Krome J, Gordon ES, Rushing J, Smith BP, Poehling GG (1997) Cartilage injuries: a review of 31,516 knee arthroscopies. Arthroscopy 13(4):456–460
Davies-Tuck ML, Wluka AE, Wang Y, Teichtahl AJ, Jones G, Ding C, Cicuttini FM (2008) The natural history of cartilage defects in people with knee osteoarthritis. Osteoarthritis Cartilage 16(3):337–342
Dhollander AA, Almqvist KF, Moens K, Vandekerckhove PJ, Verdonk R, Verdonk P, Victor J (2015) The use of a prosthetic inlay resurfacing as a salvage procedure for a failed cartilage repair. Knee Surg Sports Traumatol Arthrosc 23(8):2208–2212
Feucht MJ, Cotic M, Beitzel K, Baldini JF, Meidinger G, Schottle PB, Imhoff AB (2017) A matched-pair comparison of inlay and onlay trochlear designs for patellofemoral arthroplasty: no differences in clinical outcome but less progression of osteoarthritis with inlay designs. Knee Surg Sports Traumatol Arthrosc 25(9):2784–2791
Goebel L, Kohn D, Madry H (2016) Biological reconstruction of the osteochondral unit after failed focal resurfacing of a chondral defect in the knee. Am J Sports Med 44(11):2911–2916
Heir S, Nerhus TK, Rotterud JH, Loken S, Ekeland A, Engebretsen L, Aroen A (2010) Focal cartilage defects in the knee impair quality of life as much as severe osteoarthritis: a comparison of knee injury and osteoarthritis outcome score in 4 patient categories scheduled for knee surgery. Am J Sports Med 38(2):231–237
Hjelle K, Solheim E, Strand T, Muri R, Brittberg M (2002) Articular cartilage defects in 1,000 knee arthroscopies. Arthroscopy 18(7):730–734
Imhoff AB, Feucht MJ, Meidinger G, Schottle PB, Cotic M (2015) Prospective evaluation of anatomic patellofemoral inlay resurfacing: clinical, radiographic, and sports-related results after 24 months. Knee Surg Sports Traumatol Arthrosc 23(5):1299–1307
Jasper LL, Jones CA, Mollins J, Pohar SL, Beaupre LA (2016) Risk factors for revision of total knee arthroplasty: a scoping review. BMC Musculoskelet Disord 17:182
Kirker-Head CA, Van Sickle DC, Ek SW, McCool JC (2006) Safety of, and biological and functional response to, a novel metallic implant for the management of focal full-thickness cartilage defects: preliminary assessment in an animal model out to 1 year. J Orthop Res 24(5):1095–1108
Knutsen G, Drogset JO, Engebretsen L, Grontvedt T, Isaksen V, Ludvigsen TC, Roberts S, Solheim E, Strand T, Johansen O (2007) A randomized trial comparing autologous chondrocyte implantation with microfracture. Findings at five years. J Bone Joint Surg Am 89(10):2105–2112
Kuipers BM, Kollen BJ, Bots PC, Burger BJ, van Raay JJ, Tulp NJ, Verheyen CC (2010) Factors associated with reduced early survival in the Oxford phase III medial unicompartment knee replacement. Knee 17(1):48–52
Laursen JO (2016) Treatment of full-thickness cartilage lesions and early OA using large condyle resurfacing prosthesis: UniCAP®. Knee Surg Sports Traumatol Arthrosc 24(5):1695–1701
Laursen JO, Lind M (2017) Treatment of full-thickness femoral cartilage lesions using condyle resurfacing prosthesis. Knee Surg Sports Traumatol Arthrosc 25(3):746–751
Li CS, Karlsson J, Winemaker M, Sancheti P, Bhandari M (2014) Orthopedic surgeons feel that there is a treatment gap in management of early OA: international survey. Knee Surg Sports Traumatol Arthrosc 22(2):363–378
Manda K, Ryd L, Eriksson A (2011) Finite element simulations of a focal knee resurfacing implant applied to localized cartilage defects in a sheep model. J Biomech 44(5):794–801
Martinez-Carranza N, Ryd L, Hultenby K, Hedlund H, Nurmi-Sandh H, Lagerstedt AS, Schupbach P, Berg HE (2016) Treatment of full thickness focal cartilage lesions with a metallic resurfacing implant in a sheep animal model, 1 year evaluation. Osteoarthritis Cartilage 24(3):484–493
Miniaci A (2014) UniCAP as an alternative for unicompartmental arthritis. Clin Sports Med 33(1):57–65
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62(10):1006–1012
Pareek A, Carey JL, Reardon PJ, Peterson L, Stuart MJ, Krych AJ (2016) Long-term outcomes after autologous chondrocyte implantation: a systematic review at mean follow-up of 11.4 years. Cartilage 7(4):298–308
Pascual-Garrido C, Daley E, Verma NN, Cole BJ (2017) A comparison of the outcomes for cartilage defects of the knee treated with biologic resurfacing versus focal metallic implants. Arthroscopy 33(2):364–373
Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG (2003) Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Arthroscopy 19(5):477–484
van der List JP, Chawla H, Zuiderbaan HA, Pearle AD (2016) The role of preoperative patient characteristics on outcomes of unicompartmental knee arthroplasty: a meta-analysis critique. J Arthroplasty 31(11):2617–2627
Wright JG, Swiontkowski MF, Heckman JD (2003) Introducing levels of evidence to the journal. J Bone Joint Surg Am 85-A(1):1–3
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest with regard to the present study.
Funding
There is no funding source.
Ethical approval
This was a systematic review of published literature, and IRB approval was not required.
Informed consent
Informed consent was not applicable to this study.
Rights and permissions
About this article
Cite this article
Fuchs, A., Eberbach, H., Izadpanah, K. et al. Focal metallic inlay resurfacing prosthesis for the treatment of localized cartilage defects of the femoral condyles: a systematic review of clinical studies. Knee Surg Sports Traumatol Arthrosc 26, 2722–2732 (2018). https://doi.org/10.1007/s00167-017-4714-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4714-4