Abstract
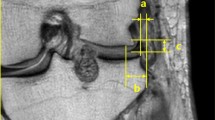
The aim of the study is to develop a clinically useful and reproducible method for evaluating lateral meniscal extrusion in normal and transplanted knees under different axial loading conditions. Magnetic resonance imaging (MRI) and ultrasound (US) were used to assess meniscal extrusion. Both types of imaging were performed at least 6 months postoperatively (mean 23.5 months). Coronal MR images (DESS-3D sequence) of the lateral compartments of 10 normal knees and 17 transplanted lateral knees were analyzed. Extrusion was defined as the distance measured from the femoral condyle or tibial plateau to the outer edge of the meniscus. Subjects were examined in the supine position. Ultrasound print-outs of the lateral compartment of both knees of ten patients (transplanted side and contralateral normal side) were analyzed. Extrusion cross-sectional area (CSA) and distance were measured just anterior to the lateral collateral ligament: the former was defined as the CSA of the meniscus outside the knee, the latter as the greatest distance from a line connecting the femur and tibia to the outer edge of the lateral meniscus. Patients were examined in the supine position, bipodal stance and unipodal stance. The viable meniscal allograft was securely sutured to a bleeding functional meniscal rim. No bone blocks were used to fix the allograft; instead, the anterior and posterior horn were firmly sutured to their enthesis. The MRI results (tibial) show the transplanted lateral meniscus to be significantly (p<0.005) more extruded in comparison to the normal lateral meniscus. The anterior horn (mean 5.8 mm, SD=2.8) of the transplanted lateral meniscus tends to be more extruded than the posterior horn (mean 2.7 mm, SD=1.48). The posterior horn of the normal lateral meniscus does not (mean 0 mm) extrude, while the mean extrusion of the anterior horn is 0.8 mm (SD=0.92). In the US results, the transplanted lateral meniscus is significantly (p<0.005) more extruded than the normal lateral meniscus in all patient positions. Both cross-sectional surface and distance are equally good parameters to determine meniscal extrusion. There is no statistical difference between patient positions. The transplanted lateral meniscus extrudes, in the supine position, bipodal and unipodal stance 6.43 (SD=1.84), 6.01 (SD=1.93) and 6.99 mm (SD=2.7) respectively. The extrusion surface of the lateral transplanted meniscus is 50.50 mm2 (SD=15.32), 47.24 mm2 (SD=14.35) and 58.61 mm2 (SD=29.65) in the supine position, bipodal stance and unipodal stance respectively. The normal lateral meniscus extrudes in the supine position, bipodal and unipodal stance 3.77 (SD=1.76), 3.94 (SD=1.66) and 3.79 mm (SD=1.79) respectively. The extrusion surface of the normal lateral meniscus is 22.42 mm2 (SD=12.54), 23.24 mm2 (SD=12.74) and 24.79 mm2 (SD=10.18) in the supine position, bipodal stance and unipodal stance respectively. The presented data shows that the transplanted lateral meniscus, without bone block fixation but with firm fixation of the horns to the original entheses, extrudes in the lateral direction significantly more than the normal meniscus. The transplanted lateral meniscus, however, does not extrude more in the lateral direction under axial load. The anterior horn of both normal and transplanted menisci is extruded more laterally than the posterior horn. Both methods are adequate to measure laterally-directed extrusion of the normal and transplanted lateral meniscus, but have distinctive advantages and disadvantages: MRI in this series visualizes the complete—from posterior to anterior—meniscal body, but only in the supine, non-weight-bearing position. Using ultrasound one can evaluate the meniscal extrusion in different conditions of axial loading, but only from a single examination point.








Similar content being viewed by others
References
Fairbank TJ (1948) Knee joint changes after meniscectomy. J Bone Joint Surg Br 30:664–670
Walker PS, Erkman MJ (1975) The role of the menisci in force transmission across the knee. Clin Orthop 109:184–192
Seedhom BB, Hargreaves DJ (1979) Transmission of the load in the knee joint with special reference to the role of the menisci. Part II: Experimental results, discussion and conclusions. Eng Med 4:220–228
Peters G, Wirth CJ (2003) The current state of meniscal allograft transplantation and replacement. Knee 10:19–31
van Arkel ER, de Boer HH (2002) Survival analysis of human meniscal transplantations. J Bone Joint Surg Br 84:227–231
Verdonk P, Almqvist KF, Demurie A, Witvrouw E, Verbruggen G, Verdonk R (2002) Viable meniscal allografts in humans: 101 cases with a 0.3–12.4 years follow-up. Osteoarthritis Cartilage 10 (Suppl A):S76 (PS168)
Verdonk R, Van Daele P, Claus B, Vandenabeele K, Desmet P, Verbruggen G, Veys EM, Claessens H (1994) Viable meniscus transplantation. Orthopade 23:153–159
Verdonk R (1997) Alternative treatments for meniscal injuries. J Bone Joint Surg Br 79:866–873
Wirth CJ, Peters G, Milachowski KA, Weismeier KG, Kohn D (2002) Long-term results of meniscal allograft transplantation. Am J Sports Med 30:174–181
Alhalki MM, Howell SM, Hull ML (1999) How three methods for fixing a medial meniscal autograft affect tibial contact mechanics? Am J Sports Med 27:320–328
Chen MI, Branch TP, Hutton WC (1996) Is it important to secure the horns during lateral meniscal transplantation? A cadaveric study. Arthroscopy 12:174–181
Paletta GA Jr, Manning T, Snell E, Parker R, Bergfeld J (1997) The effect of allograft meniscal replacement on intraarticular contact area and pressures in the human knee: a biomechanical study. Am J Sports Med 25:692–698
Verbruggen G, Verdonk R, Veys EM, Van Daele P, De Smet P, Van den Abbeele K, Claus B, Baeten D (1996) Human meniscal proteoglycan metabolism in long-term tissue culture. Knee Surg Sports Traumatol Arthrosc 4:57–63
Breitenseher MJ, Trattnig S, Dobrocky I, Kukla C, Nehrer S, Steiner E, Imhof H (1997) MR imaging of meniscal subluxation in the knee. Acta Radiol 38:876–879
Gale DR, Chaisson CE, Tottermann SMS, Schwarts RR, Gale ME, Felson D (1999) Meniscal subluxation: association with osteoarthritis and joint space narrowing. Osteoarthritis Cartilage 7:526–532
Verstraete KL, Verdonk R, Lootens T, Verstraete P, De Rooy J, Kunnen M (1997) Current status and imaging of allograft meniscal transplantation. Eur J Radiol 26:16–22
Huang A, Hull ML, Howell SM (2003)The level of compressive load affects conclusions from statistical analyses to determine whether a lateral meniscal autograft restores tibial contact pressure to normal: a study in human cadaveric knees. J Orthop Res 21:459–464
DeHaven KE (1999) Meniscus repair. Am J Sports Med 27:242–250
Acknowledgements
P.V. is a research assistant of the Fund for Scientific Research—Flanders (Belgium) (F.W.O.-Vlaanderen).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Verdonk, P., Depaepe, Y., Desmyter, S. et al. Normal and transplanted lateral knee menisci: evaluation of extrusion using magnetic resonance imaging and ultrasound. Knee Surg Sports Traumatol Arthrosc 12, 411–419 (2004). https://doi.org/10.1007/s00167-004-0500-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-004-0500-1