Abstract
Purpose
To investigate the effect of a wide range of assistance levels during neurally adjusted ventilatory assist (NAVA) and pressure support ventilation (PSV) on respiratory pattern, breathing variability, and incidence of tidal volumes (V T) above 8 and 10 ml/kg in acute respiratory failure patients.
Methods
Eight increasing NAVA levels (0.5, 1, 1.5, 2, 2.5, 3, 4, and 5 cmH2O/μV) and four increasing pressure support (PSV) levels (4, 8, 12, and 16 cmH2O) were applied to obtain 10 min of stable recordings in 15 patients.
Results
One out of 15 patients did not sustain the NAVA levels of 3, 4, and 5 cmH2O/μV and was excluded. The 5 cmH2O/μV NAVA level was not tolerated by three patients and it was excluded. Increasing NAVA levels were associated with decreased diaphragm electrical activity (EAdi), and, at variance with PSV, with small changes in V T, no changes in respiratory rate (RR), and increases in V T and EAdi variability. At high NAVA levels, an increase in V T variability was associated with increased incidence of V T above 8 and 10 ml/kg and an uncomfortable respiratory pattern in some patients.
Conclusions
Increasing NAVA levels were associated with no effect on RR, small increase in V T, and increase in V T and EAdi variability. Effective decrease in EAdi occurred at NAVA levels below 2–2.5 cmH2O/μV, while preserving respiratory variability and low risks of V T above 8 or 10 ml/kg.
Similar content being viewed by others
Introduction
Neurally adjusted ventilatory assist (NAVA) is a novel mode of mechanical ventilation during which the pressure applied by the ventilator to the airways during inspiration is proportional to the diaphragm electrical activity (EAdi) according to a multiplicative factor called “NAVA level” [1]. Studies on healthy volunteers [2], acute respiratory failure (ARF) patients [3–7], newborns [8, 9], and animal models [10–13] have shown that NAVA can efficiently unload the respiratory muscles. Clinical studies on NAVA suggest that there is a different physiologic response in respiratory pattern to changing levels of assistance than that commonly observed during pressure support ventilation (PSV) [3–8, 14]. However, most of the available data come from studies where either each NAVA level was applied for only 3 min [5] or only a narrow range of NAVA levels was applied [3, 4]. Moreover, some potentially relevant aspects of NAVA have not been investigated in the clinical setting.
First, given the strict interdependency between EAdi and ventilatory output variables, during NAVA the effects of NAVA level on respiratory pattern should be related to the amplitude of EAdi signal. We hypothesize that, in patients with low EAdi at low assistance, V T and peak airway pressure (Pawpeak) are less affected by changes of the NAVA level.
Second, it is believed that during NAVA the physiologic neural variability is preserved and unaffected by the level of assistance [6]. However, a recent study by Schmidt et al. [6] seems to suggest that the use of relatively high NAVA levels may have an amplification feedback effect on physiological neural variability. On the basis of these observations, we hypothesize that high NAVA levels may increase neural variability to an extent that may compromise patient comfort during NAVA.
Third, the idea that NAVA is relatively protected against the risk of overassistance and high lung-distending volumes and/or pressure is based mainly on the effect of NAVA on the mean airway pressure and V T, but does not take into consideration the high breath-by-breath variability characteristic of NAVA.
In this study, we investigated the effect of a wide range of assistance levels on respiratory pattern and breathing variability during NAVA and PSV in patients with acute respiratory failure (ARF). We also explored whether the effects of NAVA on V T and Pawpeak were dependent on the EAdi signal amplitude under low assistance. Finally, we explored the effect of respiratory variability on the incidence of delivering V T above 8 and 10 ml/kg.
Materials and methods
Study population
The study included 15 patients admitted to the intensive care unit (ICU) of San Gerardo Hospital from September 2007 to July 2009 (Table 1). The study was approved by the institutional ethics committee: written informed consent was provided by the patients or next of kin. All patients with ARF receiving partial ventilatory support were considered eligible. Exclusion criteria were age less than 18 years, contraindication to nasogastric tube positioning or substitution (gastroesophageal surgery in the previous 12 months, gastroesophageal bleeding in the previous 30 days, history of esophageal varices, facial trauma, and/or surgery), hemodynamic instability, and unavailability of the Servo-I ventilator integrating the NAVA module (Maquet Critical Care, Solna, Sweden) [3, 13].
Study protocol
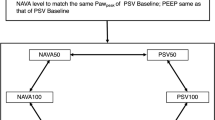
Once enrolled, patients were connected to the Servo-I ventilator. The EAdi was registered with a nasogastric tube carrying a multiple array of esophageal electrodes (EAdi catheter, Maquet Critical Care, Solna, Sweden) [13]. After placement, correct position of the EAdi catheter was assessed according to the manufacturer’s instructions [15]. The protocol consisted of two phases applied in random order: a NAVA phase consisting of eight increasing NAVA levels (0.5, 1, 1.5, 2, 2.5, 3, 4, and 5 cmH2O/μV) and a PSV phase consisting of four increasing pressure support levels (PS) (4, 8, 12, and 16 cmH2O). A stable ventilator pattern was recorded for at least 10 min during both phases.
The alarm limit of peak airway pressure on the ventilator was set to limit peak airway pressure at 35 cmH2O throughout the protocol. More details on PSV setting are reported in the online supplementary material.
The trial was discontinued whenever one of the following criteria was reached: arterial oxygen saturation less than 90%, heart rate above 140 bpm or less than 30% variation from the initial value, systolic arterial pressure greater than 180 mmHg or less than 90 mmHg, extreme agitation or sweating, or if signs of ventilatory discomfort occurred (coughing, agitation, dyspnea, irregular respiratory pattern, frequent alarming of peak airway pressure). For sedation, propofol or midazolam in conjunction with opiates (remifentanyl or fentanyl) were titrated to a target Ramsey sedation score of 2 or 3 [16] and maintained constant throughout the study.
Data analysis
Airway pressure, flow, volume, and EAdi waveforms were acquired from the ventilator (Labview, Texas Instrument, Houston, TX, USA). All parameters are reported as the average from the last 5 min of stable recording for each step. From acquired waveforms we obtained Pawpeak, mean inspiratory (Pawimean) airway pressure, ventilator respiratory rate (RRflow), inspiratory (Tiflow) and expiratory (Teflow) time, total breath duration (Ttotflow), inspiratory duty cycle (Tiflow/Ttotflow), V T peak inspiratory EAdi (EAdipeak), patient’s neural respiratory rate (RRneural), inspiratory (Tineural) (time from the onset of the EAdi swing and EAdipeak) and expiratory (Teneural) (time between EAdipeak and the onset of the next EAdi swing) time, total neural breath duration (Ttotneural), and the neural inspiratory duty cycle (Tineural/Ttotneual) (Fig. 1). To obtain an electrical surrogate of pressure–time product, the integral of the EAdi signal over time from its onset to its peak value (electrical time product for each breath, ETPbreath) was multiplied by the RR (ETP per minute, ETPmin), and divided by the minute ventilation (ETP indexed for liter of ventilation, ETPLiter).
Representative examples of measurements of the main parameters studied during NAVA (left panel) and PSV (right panel). All data were obtained by averaging all values of each parameter computed from all breaths taken over 5 min of stable respiratory pattern. Vertical dotted lines represent ventilator respiratory cycles according to airway flow; vertical dashed lines represent patient (neural) respiratory cycles according to EAdi signal. Paw peak peak airway pressure, Pawi mean average airway pressure during inspiration (horizontal dashed lines), V T tidal volume, EAdi peak peak of EAdi during inspiration, ETP breath electrical time product of EAdi computed as the integral of the EAdi signal over time from the onset of the inspiratory rise to its peak value (gray area on EAdi signal, Ti flow time from start to end of inspiratory flow, Te flow time from start of expiratory flow to start of inspiratory flow of next breath, Ttot flow sum of Tiflow and Teflow, Ti neural time from onset of EAdi rise to the EAdipeak, Te neural time between EAdipeak and onset of the next EAdi rise, Ttot neural sum of Tineural and Teneural
Respiratory pattern variability was assessed by computing the coefficient of variation (CV) for V T, RRflow, EAdipeak, and Pawpeak. The extent of patient–ventilator dyssynchrony was assessed by computing the asynchrony index (AI). Details on methods and results about dyssynchrony are available in the online supplement. For each patient we selected the maximal and minimal average V T, and the maximal and minimal average inspiratory airway pressure swing computed as Pawpeak − PEEP (Pawpeak−PEEP) among all NAVA levels. To explore the influence of EAdi signal amplitude on the effect of different NAVA levels maximal and minimal V T and Pawpeak−PEEP were correlated with the EAdipeak at 0.5 cmH2O/μV NAVA level (EAdi0.5).
Statistical analysis
The effect of NAVA or PSV level was assessed separately by one-way analysis of variance for repeated measurements. The normality assumption was tested by the Shapiro–Wilk W test, whereas the sphericity assumption was tested by the Mauchly’s test. Bonferroni correction was applied to compare each level of assistance with both the highest and lowest level of assistance within the same ventilatory mode. Correlation between two data series was tested by linear regression analysis. Results in text, tables, and figures are expressed as mean ± standard deviation unless otherwise indicated. All statistical analyses were performed with the SPSS 18 (SPSS Inc, Chigago, IL, USA).
Results
One patient unable to sustain NAVA levels 3 and 4 cmH2O/μV and PS level 16 cmH2O was excluded from the analysis. Three other patients were unable to sustain NAVA level 5 cmH2O/μV; thus, this level was excluded from the analysis and NAVA level 4 cmH2O/μV was considered the highest assist level during NAVA. In all these cases we observed dyspnea, agitation, and an unstable respiratory pattern with high breath-by-breath variability in EAdi, V T, and Pawpeak which frequently reached 35 cmH2O. All patients showed phases of 5–10 breaths during which the EAdi signal did not return to its basal expiratory value (Fig. 2). No modifications in oxygen saturation and hemodynamics were observed.
Respiratory pattern
During NAVA, there was a small but significant increase in V T at NAVA levels 1.5 and 2 cmH2O/μV compared to V T at 0.5 cmH2O/μV (Fig. 3, see online supplement for more details). There were no statistically significant differences between other NAVA levels. The effect of NAVA level on V T was highly variable among patients. None of the other respiratory variables showed significant changes at different levels of assistance (Table 2). On the contrary, during PSV, increasing PS levels were associated with significant increases in V T, Tiflow, Teflow, Teneural, and decreases in RRflow, Tineural, Ti/TOTflow, and Ti/TOTneural (Table 2). Minute ventilation did not change significantly during either NAVA or PSV.
Effect of the level of assistance during NAVA and PSV on the peak of diaphragm electrical activity (EAdipeak), respiratory rate (RR), peak of airway pressure (Pawpeak), and tidal volume (V T). *p < 0.05 versus lowest level of assistance of the same ventilatory mode; #p < 0.05 versus highest level of assistance of the same ventilatory mode
Pawpeak and Pawimean increased with increasing levels of assistance both during NAVA and PSV. Incidence of Pawpeak higher than 35 cmH2O was extremely rare, 1 ± 1.2% at NAVA level 4 cmH2O/μV (maximal incidence 4.5% at NAVA level 5 cmH2O/μV) (online supplementary Fig. E10).
Indices of muscle unloading
During NAVA and PSV, EAdipeak, ETPbreath, ETPmin, and ETPLiter decreased with increasing assistance levels. During NAVA, most of the EAdi reduction occurred between the NAVA levels of 0.5 and 2 cmH2O/μV.
Effect of EAdi0.5 on Pawpeak−PEEP and V T/kg
The effects of NAVA level on V T and Pawpeak−PEEP depended on the EAdi0.5. The higher the Eadi0.5, the wider the range of V T (computed as difference between the maximal and minimal V T) (r = 0.566, p < 0.05) and Pawpeak−PEEP (Fig. 4) over different NAVA levels. In some patients, it was not possible to find a NAVA level yielding a Pawpeak−PEEP equivalent to those recorded during PSV (Fig. 4). In particular, patients with low EAdi0.5 could not match high PS levels, whereas patients with high EAdi0.5 could not match low PS levels.
Correlation between the maximal (Pawpeak−PEEP maximal, open circles), and minimal (Pawpeak−PEEP minimal, closed circles) peak airway pressure above PEEP (computed as Pawpeak − PEEP) values from different NAVA levels for each patient and the diaphragm electrical activity at the 0.5 cmH2O/μV NAVA level (EAdi0.5). For a given EAdi the two regression lines represent the lower and higher limit of airway pressure swing obtainable during inspiration with the NAVA levels applied in the study. The area enclosed between the two lines represents the level of PSs that can be matched during NAVA. The range of Pawpeak−PEEP (computed as the difference between maximal and minimal Pawpeak−PEEP, i.e., the distance between open and closed circles in the graph) also positively correlated with EAdi0.5 (r = 0.592, p < 0.05)
Variability
The CVs of V T, Pawpeak, RR, and EAdipeak are reported in Fig. 5 (details in the online supplement). During NAVA, the CVs of V T, Pawpeak, and EAdipeak increased with increasing NAVA levels, whereas that of RR did not change significantly. During PSV, the CVs of RR and EAdipeak increased with increasing PS levels, whereas that of V T showed a decreasing trend. The CVs of V T and Pawpeak were significantly higher during NAVA at both the lowest and highest levels of assistance.
Effect of the level of assistance during NAVA and PSV on the coefficient of variation of tidal volume (CV V T), respiratory rate (CV RR), peak of airway pressure (CV Pawpeak), and peak of diaphragm electrical activity (CV EAdipeak). *p < 0.05 versus lowest level of assistance of the same ventilatory mode; #p < 0.05 versus highest level of assistance of the same ventilatory mode
V T/kg
In some patients the proportion of V T above 8 and 10 ml/kg increased at increasing NAVA levels (online supplementary Fig. E9). The three patients showing the highest proportion of V T above 10 ml/kg at NAVA level 4 cmH2O/μV were the same patients who could not tolerate NAVA level 5 cmH2O/μV.
Discussion
In the present study we explored a wide range of assist levels during both NAVA and PSV in patients with ARF. Responses to NAVA were different than to PSV. Increasing the level of assistance during NAVA was associated with a decrease in EAdi, a small increase in the average V T, and an increase in V T and EAdi variability. We indicated the EAdi at NAVA level 0.5 cmH2O/μV (EAdi0.5) as the highest diaphragmatic activation under low ventilator support. The range of changes in V T and Paw swing over different NAVA levels was greater in patients with higher EAdi0.5. In some patients, it was not possible to find NAVA levels producing Paw swings equivalent to those produced by any of the tested PS level. The increase in V T variability was associated with an increased proportion of V T above 8 and 10 ml/kg and, in some patients, with signs of ventilatory discomfort.
Effect of NAVA on V T and RR
In this study increasing NAVA levels led to a decrease in EAdi, had only marginal effects on V T and no effect on RR. Most of the effects on EAdi and V T were observed between the NAVA levels 0.5 and 2 cmH2O/μV. These results are consistent with those of previous studies [3–7]. Brander et al. [5] observed, in all patients, a two-phase response to increasing NAVA levels, characterized by an initial steep increase in both Pawpeak and V T followed by a second phase in which the increase in Pawpeak slowed down and V T reached a plateau. In contrast, we observed wide between-patient variability in response to increasing NAVA levels, and some of our patients did not show any change in EAdi or V T. However, in Brander’s study NAVA was delivered with a prototype system in which NAVA levels were expressed in different units.
Colombo et al. [3] applied NAVA levels between approximately 0.5 and 2 cmH2O/μV in ARF patients and found an average increase in V T/kg of 0.7 ml/kg. In a study by Schmidt et al. [6] in patients recovering from ARF, the application of NAVA levels from 1 to 4 cmH2O/μV produced a mean change in V T of approximately 80 ml; in contrast to our study, a significant increase in V T was observed up to NAVA level 4 cmH2O/μV. Some of the differences may be explained by the patients’ population characteristics. In particular, in the aforementioned studies, patients showed higher EAdi values at low NAVA levels and smaller decreases in EAdi with changing NAVA levels than in our study. According to the positive correlation found between EAdi0.5 and the range of changes in V T, smaller changes in V T are expected in our population. However, all these studies consistently show that increasing the level of assistance during NAVA produces an increase in Pawpeak and a reduction in EAdi that, in contrast to PSV, are accompanied by small effects on V T and RR.
These results have important clinical implications. The main ventilator setting during partial ventilatory modes is the level of assistance. With classical modes of partial ventilatory support, such as PSV, increased assistance levels are associated with decrease in RR and, often, with increase in V T [17, 18]. The effect on RR is particularly important because, as long as the patient is not overassisted (in this case a decrease in RR may be associated with overinflation and increased muscular effort), its decrease is interpreted as a sign of relief from respiratory distress [19, 20]. Given the scarce effect on respiratory pattern, the setting of the NAVA level cannot be easily driven by changes in V T and, most of all, RR. Whether the higher RR commonly observed during NAVA should be accepted as an expression of the patient’s best mechanical compromise or whether it is a sign of the inability of NAVA to effectively relieve respiratory distress remains to be investigated.
Effect of EAdi0.5 on Pawpeak and V T/kg
We found that EAdi0.5 is an important determinant of the range of V T and Pawpeak changes in response to varying NAVA levels. This finding may have important consequences for the use of NAVA in patients with intrinsically low or high EAdi values. In particular, patients showing low EAdi because of muscular weakness, or patients in whom the EAdi is not a reliable measure of diaphragmatic muscular effort (i.e., patients breathing predominantly with intercostal muscle) may not benefit from the use of NAVA. Further investigation of these potential limitations of NAVA for these categories of patients is necessary. An interesting use of an equivalent of the EAdi0.5 was recently proposed by Rozé et al. [21] as a parameter to titrate NAVA level.
In all studies comparing NAVA and PSV, it has been assumed that equal Pawpeak values correspond to equivalent assistance levels [3, 4]. We showed in this study that the range of Pawpeak obtainable during NAVA strongly depends on the EAdi at low levels of assistance. Patients with low EAdi0.5 cannot obtain Pawpeak values obtained at high PS levels even at high NAVA levels, whereas patients with high EAdi0.5 cannot obtain Pawpeak values obtained at low levels of PSV. However, the impossibility to reach an equivalent Pawpeak when switching from PSV to NAVA does not imply inadequate ventilator assistance during NAVA. Considering the different response in respiratory pattern between NAVA and PSV, we suggest that PSV and NAVA may not always be matched in terms of equivalent Pawpeak.
Effect of NAVA on breathing variability
Normal human subjects exhibit considerable variability in V T and RR [22] which, during lung injury, may improve oxygenation and respiratory mechanics [23–27]. Thus, preservation of physiological variability during NAVA is considered an important favorable effect.
In agreement with our results, Schmidt et al. [6] found similar variability in EAdi between NAVA and PSV, higher variability of V T and Pawpeak during NAVA, and increased variability of V T and Pawpeak with increasing NAVA levels. However, in contrast to our study, they observed only a negligible, though statistically significant, effect on EAdi variability. They concluded that neural variability is unaffected by NAVA level, supporting the common idea that NAVA seems to preserve the physiologic neural variability. Our results partially challenge this idea. In fact, in our study the increase in NAVA level produces an increase in EAdi variability more marked than in Schmidt’s study. We found a high heterogeneity between patients with increases in CV of EAdi ranging between 0 and 57%. In four patients at NAVA level 5 cmH2O/μV and in one patient at NAVA levels 3 and 4 cmH2O/μV, we observed a highly unstable pattern that was associated with periodical delivery of high V T and high Pawpeak followed by periods of apnea, and signs of patient discomfort that required discontinuation of the study. A similar behavior was described by Allo et al. [28] in rabbits with lung injury. They observed that increasing the NAVA level beyond a level able to reverse inspiratory esophageal pressure from negative to positive frequently resulted in a periodic breathing pattern [28].
We hypothesize that in some patients high NAVA levels may amplify the physiologic neural variability to an extent that overcomes the expected output variability, triggering a sort of oscillatory feedback behavior that bypasses the patient’s control. This behavior is likely mediated by pulmonary inhibitory vagal reflexes [29] and it is probably triggered when NAVA levels are further increased after the patient’s respiratory demand is already satisfied and the downregulation of inspiratory effort is maximal. This behavior could be considered a form of overassistance specific to NAVA.
Incidence of high tidal volumes
The common idea that NAVA is relatively protected against the risk of overassistance and high lung-distending volumes and/or pressures is based mainly on the effect of NAVA on mean Paw and V T [2, 3, 5, 10]; it does not take into account the large breath-by-breath variability that we and others have observed. An important consequence of this increased variability is the increased proportion of high V T. When high variability is present, an average value within the protective ranges does not exclude the possibility of delivering intermittently a potentially harmful V T. We found that as the NAVA level increased, a higher proportion of high V T was delivered with some patients receiving up to 60% of the V T above 10 ml/kg at higher NAVA levels. Though we lack data clearly indicating which V T ranges may be accepted during assisted mechanical ventilation to prevent ventilator-induced lung injury, a V T target below 8 ml/kg appears reasonable and feasible also during assisted mechanical ventilation, including NAVA.
Limitations of the study
We studied a selected population of mechanically ventilated patients with ARF, heterogeneous in terms of etiology of respiratory failure, length of mechanical ventilation, and respiratory muscle efficiency. However, we excluded patients in the early acute phase of respiratory failure and those with COPD. For this reason, and considering the relatively small sample of patients, our results may not apply to all ICU patients receiving partial support ventilation. In this study we tested the same predefined and wide range of ventilator assistance levels in all patients irrespective of their EAdi amplitude and conditions; this approach served the purpose of the study, which was not to describe a titrating procedure for NAVA, but to study the physiological effects of different NAVA levels in a heterogeneous population.
Conclusions
Increased levels of assistance during NAVA are associated with small changes in V T and RR and increased variability in V T and EAdi. The effect of NAVA level on V T and Pawpeak is smaller in patients with lower EAdi amplitude at low level of assistance. In some patients it is not possible to find NAVA levels yielding Pawpeak values equivalent to those produced during PSV. Excessive increases in V T and EAdi variability at the higher NAVA levels investigated were associated, in some patients, with increased incidence of V T above 10 ml/kg and with uncomfortable respiratory patterns. In most patients, NAVA levels below 2–2.5 cmH2O/μV yield an effective decrease of EAdi, while preserving the patient’s respiratory variability and low risks of excessive V T and patient discomfort.
References
Sinderby C, Navalesi P, Beck J, Skrobik Y, Comtois N, Friberg S, Gottfried SB, Lindström L (1999) Neural control of mechanical ventilation in respiratory failure. Nat Med 5:1433–1436
Sinderby C, Beck J, Spahija J, de Marchie M, Lacroix J, Navalesi P, Slutsky AS (2007) Inspiratory muscle unloading by neurally adjusted ventilatory assist during maximal inspiratory efforts in healty subjects. Chest 131:711–717
Colombo D, Cammarota G, Bergamaschi V, De Lucia M, Corte FD, Navalesi P (2008) Physiologic response to varying levels of pressure support and neurally adjusted ventilatory assist in patients with acute respiratory failure. Intensive Care Med 34:2010–2018
Wu XY, Huang YZ, Yang Y, Liu SQ, Liu HG, Qiu HB (2009) Effects of neurally adjusted ventilatory assist on patient-ventilator synchrony in patients with acute respiratory distress syndrome. Zhonghua Jie He He Hu Xi Za Zhi 32:508–512
Brander L, Leong-Poi H, Beck J, Brunet F, Hutchison SJ, Slutsky AS, Sinderby C (2009) Titration and implementation of neurally adjusted ventilatory assist in critically ill patients. Chest 135:695–703
Schmidt M, Demoule A, Cracco C, Gharbi A, Fiamma MN, Straus C, Duguet A, Gottfried SB, Similowski T (2010) Neurally adjusted ventilatory assist increases respiratory variability and complexity in acute respiratory failure. Anesthesiology 112:670–681
Spahija J, de Marchie M, Albert M, Bellemare P, Delisle S, Beck J, Sinderby C (2010) Patient-ventilator interaction during pressure support ventilation and neutrally adjusted ventilatory assist. Crit Care Med 38:518–526
Breatnach C, Conlon NP, Stack M, Healy M, O’Hare BP (2010) A prospective crossover comparison of neurally adjusted ventilatory assist and pressure-support ventilation in a pediatric and neonatal intensive care unit population. Pediatr Crit Care Med 11:7–11
Beck J, Reilly M, Grasselli G, Mirabella L, Slutsky AS, Dunn MS, Sinderby C (2009) Patient-ventilator interaction during neurally adjusted ventilatory assist in low birth weight infants. Pediatr Res 65:663–668
Brander L, Sinderby C, Lecomte F, Leong-Poi H, Bell D, Beck J, Tsoporis JN, Vaschetto R, Schultz MJ, Parker TG, Villar J, Zhang H, Slutsky AS (2009) Neurally adjusted ventilatory assist decreases ventilator-induced lung injury and non-pulmonary organ dysfunction in rabbits with acute lung injury. Intensive Care Med 35:1979–1989
Beck J, Campoccia F, Allo JC, Brander L, Brunet F, Slutsky AS, Sinderby C (2007) Improved synchrony and respiratory unloading by neurally adjusted ventilatory assist (NAVA) in lung-injured rabbits. Pediatr Res 61:289–294
Allo JC, Beck J, Brander BrunetF, Slutsky AS, Sinderby CA (2006) Influence of neurally adjusted ventilatory assist (NAVA) and PEEP on breathing pattern in rabbits with acute lung injury. Crit Care Med 34:2997–3004
Lecomte F, Brander L, Jalde F, Beck J, Qui H, Elie C, Slutsky AS, Brunet F, Sinderby C (2009) Physiological response to increasing levels of neurally adjusted ventilator assist (NAVA). Respir Physiol Neurobiol 30:117–124
Navalesi P, Costa R (2003) New modes of mechanical ventilation: proportional assist ventilation, neurally adjusted ventilatory assist and fractal ventilation. Curr Opin Crit Care 9:51–58
Barwing J, Ambold M, Linden N, Quintel M, Moerer O (2009) Evaluation of the catheter positioning for neurally adjusted ventilatory assist. Intensive Care Med 35:1809–1814
Ramsay MAE, Savege TM, Simpson BR, Goodwin R (1974) Controlled sedation with alpaxalone-alphadolone. Br Med J 2:656–659
Brochard L, Harf A, Lorino H, Lemaire F (1989) Inspiratory pressure support prevents diaphragmatic fatigue during weaning from mechanical ventilation. Am Rev Respir Dis 139:513–521
Tokioka H, Saito S, Kosaka F (1989) Effects of pressure support ventilation on breathing pattern and respiratory work. Intensive Care Med 15:491–494
Jubran A, Van de Graaff WB, Tobin MJ (1995) Variability of patient-ventilator interaction with pressure support ventilation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 152:129–136
Thille AW, Cabello B, Galia F, Lyazidi A, Brochard L (2008) Reduction of patient-ventilator asynchrony by reducing tidal volume during pressure-support ventilation. Intensive Care Med 8:1477–1486
Rozé H, Lafrikh A, Perrier V, Germain A, Dewitte A, Gomez F, Janvier G, Ouattara A (2011) Daily titration of neurally adjusted ventilatory assist using the diaphragm electrical activity. Intensive Care Med 37:1087–1094
Tobin MJ, Mador MJ, Guenther SM, Lodato RF, Sackner MA (1988) Variability of resting respiratory center drive and timing in healthy subjects. J Appl Physiol 65:309–317
Arold SP, Mora R, Lutchen KR, Ingenito EP, Suki B (2002) Variable tidal volume ventilation improves lung mechanics and gas exchange in a rodent model of acute lung injury. Am J Respir Crit Care Med 165:366–371
Boker A, Haberman CJ, Girling L, Guzman RP, Louridas G, Tanner JR, Cheang M, Maycher BW, Bell DD, Doak GJ (2004) Variable ventilation improves perioperative lung function in patients undergoing abdominal aortic aneurysmectomy. Anesthesiology 100:608–616
Mutch WA, Harms S, Ruth GM, Kowalski SE, Girling LG, Lefevre GR (2000) Biologically variable or naturally noisy mechanical ventilation recruits atelectatic lung. Am J Respir Crit Care Med 162:319–323
Patroniti N, Foti G, Cortinovis B, Maggioni E, Bigatello LM, Cereda M, Pesenti A (2002) Sigh improves gas exchange and lung volume in patients with acute respiratory distress syndrome undergoing pressure support ventilation. Anesthesiology 96:788–794
Spieth PM, Carvalho AR, Pelosi P, Hoehn C, Meissner C, Kasper M, Hübler M, von Neindorff M, Dassow C, Barrenschee M, Uhlig S, Koch T, de Abreu MG (2009) Variable tidal volumes improve lung protective ventilation strategies in experimental lung injury. Am J Respir Crit Care Med 179:684–693
Allo JC, Beck JC, Brander L, Brunet F, Slutsky AS, Sinderby CA (2006) Influence of neurally adjusted ventilatory assist and positive end-expiratory pressure on breathing pattern in rabbits with acute lung injury. Crit Care Med 34:2997–3004
Sammon MP, Bruce EN (1991) Vagal afferent activity increases dynamical dimension of respiration in rats. J Appl Physiol 70:1748–1762
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Patroniti, N., Bellani, G., Saccavino, E. et al. Respiratory pattern during neurally adjusted ventilatory assist in acute respiratory failure patients. Intensive Care Med 38, 230–239 (2012). https://doi.org/10.1007/s00134-011-2433-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-011-2433-8