Abstract
Objective
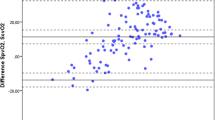
Comparison of the bias and the limits of agreement (LOA; 2 SD) of the central venous saturation (ScvO2) before, during and after coronary artery bypass graft surgery with a simultaneous measurement of the mixed venous saturation (SvO2).
Design and setting
Prospective controlled study in a university hospital department of anaesthesiology.
Patients
60 patients with coronary artery bypass surgery, 300 paired measurements of SvO2 and ScvO2.
Measurements and results
ScvO2 and SvO2 were analysed after induction of anaesthesia 15 min after cardiopulmonary bypass and 1, 6 and 18 h after admission to the intensive care unit. Regression analysis for the pooled measurements of ScvO2 and SvO2 showed a correlation R 2 = 0.52. After induction of anaesthesia 15 min after weaning from cardiopulmonary bypass and 6 h after admission to the intensive care unit the correlation coefficient was R 2 = 0.46, on admission to the intensive care unit it was R 2 = 0.42, and at 18 h it was R 2 = 0.38. Bland–Altman analysis for the measurements of ScvO2 and SvO2 showed a mean bias and LOA of 0.3% and −11.9 to +12.4%. In patients with a low ScvO2 there was a trend to overestimate the SvO2 by using the ScvO2. The only factor that influenced the ΔSvO2 − ScvO2 was the oxygen extraction rate (R 2 = 0.16). In patients with ScvO2 below 70% this association was more pronounced (R 2 = 0.60).
Conclusions
Our findings demonstrate that oxygen extraction rate is the major factor in the difference between SvO2 and ScvO2. Under certain circumstances ScvO2 differed substantially from SvO2. Therefore in selected patients both parameters should be monitored to exclude general or focal hypoperfusion.



Similar content being viewed by others
References
Andrews P, Azoulay E, Antonelli M, Brochard L, Brun-Buisson C, De Backer D, Dobb G, Fagon JY, Gerlach H, Groeneveld J, Mancebo J, Metnitz P, Nava S, Pugin J, Pinsky M, Radermacher P, Richard C, Tasker R (2006) Year in review in intensive care medicine, 2005. I. Acute respiratory failure and acute lung injury, ventilation, hemodynamics, education, renal failure. Intensive Care Med 32:207–216
Connors AF Jr, Speroff T, Dawson NV, Thomas C, Harrell FE Jr, Wagner D, Desbiens N, Goldman L, Wu AW, Califf RM, Fulkerson WJ Jr, Vidaillet H, Broste S, Bellamy P, Lynn J, Knaus WA (1996) The effectiveness of right heart catheterization in the initial care of critically ill patients. SUPPORT investigators. JAMA 276:889–897
Richard C, Warszawski J, Anguel N, Deye N, Combes A, Barnoud D, Boulain T, Lefort Y, Fartoukh M, Baud F, Boyer A, Brochard L, Teboul JL (2003) Early use of the pulmonary artery catheter and outcomes in patients with shock and acute respiratory distress syndrome: a randomized controlled trial. JAMA 290:2713–2720
Harvey S, Harrison DA, Singer M, Ashcroft J, Jones CM, Elbourne D, Brampton W, Williams D, Young D, Rowan K (2005) Assessment of the clinical effectiveness of pulmonary artery catheters in management of patients in intensive care (PAC-Man): a randomised controlled trial. Lancet 366:472–477
Sander M, von Heymann C, Foer A, von Dossow V, Grosse J, Dushe S, Konertz WF, Spies CD (2005) Pulse contour analysis after normothermic cardiopulmonary bypass in cardiac surgery patients. Crit Care 9:R729–R734
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345:1368–1377
Polonen P, Ruokonen E, Hippelainen M, Poyhonen M, Takala J (2000) A prospective, randomized study of goal-oriented hemodynamic therapy in cardiac surgical patients. Anesth Analg 90:1052–1059
Reinhart K, Rudolph T, Bredle DL, Hannemann L, Cain SM (1989) Comparison of central-venous to mixed-venous oxygen saturation during changes in oxygen supply/demand. Chest 95:1216–1221
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet I:307–310
Critchley LA, Critchley JA (1999) A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput 15:85–91
Berridge JC (1992) Influence of cardiac output on the correlation between mixed venous and central venous oxygen saturation. Br J Anaesth 69:409–410
Schou H, Perez DSV, Larsson A (1998) Central and mixed venous blood oxygen correlate well during acute normovolemic hemodilution in anesthetized pigs. Acta Anaesthesiol Scand 42:172–177
Reinhart K, Bloos F (2005) The value of venous oximetry. Curr Opin Crit Care 11:259–263
Lee J, Wright F, Barber R, Stanley L (1972) Central venous oxygen saturation in shock: a study in man. Anesthesiology 36:472–478
Reinhart K, Kersting T, Fohring U, Schafer M (1986) Can central-venous replace mixed-venous oxygen saturation measurements during anesthesia? Adv Exp Med Biol 200:67–72
Meier-Hellmann A, Reinhart K, Bredle DL, Specht M, Spies CD, Hannemann L (1997) Epinephrine impairs splanchnic perfusion in septic shock. Crit Care Med 25:399–404
Reinhart K, Kuhn HJ, Hartog C, Bredle DL (2004) Continuous central venous and pulmonary artery oxygen saturation monitoring in the critically ill. Intensive Care Med 30:1572–1578
De Backer D, Creteur J, Noordally O, Smail N, Gulbis B, Vincent JL (1998) Does hepato-splanchnic VO2/DO2 dependency exist in critically ill septic patients? Am J Respir Crit Care Med 157:1219–1225
Braun JP, Schroeder T, Buehner S, Jain U, Dopfmer U, Schuster J, Bas S, Schimke I, Dohmen PM, Lochs H, Konertz W, Spies C (2006) Small-dose epoprostenol decreases systemic oxygen consumption and splanchnic oxygen extraction during normothermic cardiopulmonary bypass. Anesth Analg 102:17–24
Braun JP, Schroeder T, Buehner S, Dohmen P, Moshirzadeh M, Grosse J, Streit F, Schlaefke A, Armstrong VW, Oellerich M, Lochs H, Konertz W, Kox WJ, Spies C (2004) Splanchnic oxygen transport, hepatic function and gastrointestinal barrier after normothermic cardiopulmonary bypass. Acta Anaesthesiol Scand 48:697–703
Berendes E, Mollhoff T, Van-Aken H, Schmidt C, Erren M, Deng MC, Weyand M, Loick HM (1997) Effects of dopexamine on creatinine clearance, systemic inflammation, and splanchnic oxygenation in patients undergoing coronary artery bypass grafting. Anesth Analg 84:950–957
Chawla LS, Zia H, Gutierrez G, Katz NM, Seneff MG, Shah M (2004) Lack of equivalence between central and mixed venous oxygen saturation. Chest 126:1891–1896
Dongre SS, McAslan TC, Shin B (1977) Selection of the source of mixed venous blood samples in severely traumatized patients. Anesth Analg 56:527–532
Faber T (1995) Central venous versus mixed venous oxygen content. Acta Anaesthesiol Scand Suppl 107:33–36
Martin C, Auffray JP, Badetti C, Perrin G, Papazian L, Gouin F (1992) Monitoring of central venous oxygen saturation versus mixed venous oxygen saturation in critically ill patients. Intensive Care Med 18:101–104
Dueck MH, Klimek M, Appenrodt S, Weigand C, Boerner U (2005) Trends but not individual values of central venous oxygen saturation agree with mixed venous oxygen saturation during varying hemodynamic conditions. Anesthesiology 103:249–257
Ander DS, Jaggi M, Rivers E, Rady MY, Levine TB, Levine AB, Masura J, Gryzbowski M (1998) Undetected cardiogenic shock in patients with congestive heart failure presenting to the emergency department. Am J Cardiol 82:888–891
Acknowledgements
The authors appreciate the diligent linguistic revision of this manuscript by Mrs. Sirka Sander (certified English translator) and thank their colleagues Mrs. Anja Heinemann (all from the Department of Anaesthesiology and Intensive Care Medicine, Charité University Medicine Berlin, Charité Campus Mitte/Campus Virchow Klinikum, Germany) for helping with the acquisition of the data, as well as Mrs. Gerda Siebert, Dipl.-Math., Department of Medical Biometry, Charité University Medicine Berlin, Germany) for the detailed statistical advice in analysing the data.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was financially supported by a research grant from the German Research Society (DFG-SA 1346/4–1) and institutional research grants of the Charité Medical School.
Rights and permissions
About this article
Cite this article
Sander, M., Spies, C.D., Foer, A. et al. Agreement of central venous saturation and mixed venous saturation in cardiac surgery patients. Intensive Care Med 33, 1719–1725 (2007). https://doi.org/10.1007/s00134-007-0684-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0684-1