Abstract
Objectives
To determine the effects of an intravenous bolus dose of a vasopressin analogue, terlipressin (1 mg), on systemic haemodynamic parameters and gastric mucosal perfusion (GMP) in patients with catecholamine-treated septic shock using a gastric tonometry and laser-Doppler flowmetry technique.
Design
Prospective open label study.
Settings
Two multidisciplinary intensive care units.
Patients
Fifteen patients with norepinephrine-treated septic shock.
Interventions
Every patient with mean arterial pressure between 50 and 55 mmHg treated with high dose norepinephrine received an intravenous bolus dose of terlipressin as last resort therapy. A laser-Doppler probe and tonometer were introduced into the gastric lumen.
Measurements and main results
Terlipressin produced a decrease in cardiac output (p<0.05), a progressive increase in mean arterial pressure (p<0.05) and in GMP, detected by laser-Doppler flowmetry (p<0.05) over 30 min and sustained for at least 24 h. The ratio of GMP to systemic oxygen delivery increased after terlipressin bolus dose (p<0.05). The gradient between gastric mucosal and arterial PCO2 tended to be lower after terlipressin, and the difference was statistically significant (p<0.05) after 8 h. Terlipressin administration significantly increased (p<0.05) urine output compared to baseline and higher values were found at each set of measurement. The terlipressin-induced increase in urine output was associated with a significantly increased creatinine clearance (p<0.05). Reduction of the high-dose norepinephrine was observed in all patients (p<0.05).
Conclusions
Our findings showed that, in patients with norepinephrine-treated septic shock, terlipressin increased GMP, urine output and creatinine clearance by an increase in mean arterial pressure.
Similar content being viewed by others
Introduction
Septic shock is characterised by decreased peripheral vascular resistance, impaired distribution of blood flow and oxygen extraction with normal or improved oxygen delivery. Altered peripheral resistance in septic shock could result in redistribution of cardiac output (CO) with the risk of hypoperfusion of the splanchnic organs. A combination of vasodilatation and pronounced vascular hyporeactivity to conventional vasopressor treatment with high dose norepinephrine often result in resistant hypotension. The discovery of vasopressin deficiency and hypersensitivity in septic shock in humans has suggested a new treatment in norepinephrine-resistant hypotension [1, 2]. The haemodynamic effects of vasopressin have not been studied extensively in endotoxic and septic shock [3, 4, 5, 6, 7, 8, 9]. Vasopressin induces an increase in mean arterial pressure (MAP) and a decrease in CO mainly linked to a negative chronotropic effect [10]. For this reason infusion of low-dose vasopressin might be useful in norepinephrine-resistant septic shock. However, rebound hypotension often occurs when the drug is discontinued and vasopressin has to be administered for several days [11].
Terlipressin, a synthetic analogue of vasopressin, has a half-life of 6 h and its effects occur via vascular V1a receptors and renal tubular V2 receptors [12]. In addition to its effects on microvascular blood flow, terlipressin also reduces CO via reflex mechanisms, mediated through central nervous V1a receptors. The fall in CO and the potent vasoconstrictor response on splanchnic macro- and micro-circulation may cause, or at least worsen, gut mucosal ischaemia.
The goal of this study was to evaluate the effects of an intravenous bolus dose of terlipressin on gastric mucosal perfusion (GMP), using laser-Doppler flowmetry and gastric tonometry, in patients with norepinephrine-treated septic shock.
Materials and methods
Patients
The study protocol was approved by the local institutional ethics committee. Informed written consent was obtained from the closest relative of each patient.
Fifteen critically ill patients were enrolled in the study (ages 63±12 years, male/female ratio 10:5). All patients had clinical and laboratory parameters that fulfilled the criteria of septic shock [13]. The Acute Physiology and Chronic Health Evaluation II score was 27 (range 25–30). We included only patients with septic shock whose hypotension (mean arterial pressure 51±1.5 mmHg) failed to respond to vasopressor support associated with volume resuscitation (pulmonary artery occlusion pressure [PAOP] 14 mmHg). Vasopressor support was defined as: 0.6 µg/kg per min or more of norepinephrine for at least 36 h. The clinical characteristics of the study group are summarised in Table 1. Each patient was mechanically ventilated and sedated with continuous intravenous sufentanil and midazolam. Exclusion criteria were: pregnancy, present or suspected acute coronary artery disease, present or suspected acute mesenteric ischaemia or vasospastic diathesis.
Parameters investigated
Systemic haemodynamic and oxygenation parameters
Clinical monitoring of the patients included a pulmonary artery catheter (7.5 Fr, Arrow International, Reading, PA, USA) and a radial artery catheter. MAP, right atrial pressure (RAP), mean pulmonary arterial pressure (MPAP) and PAOP (Solar M8000, Marquette Hellige Medical System, WI, USA) were measured at end expiration. Heart rate (HR) was analysed from a continuous recording of electrocardiogram with ST segments monitored. CO was measured by thermodilution (Solar M8000, Marquette Hellige Medical System, WI, USA). Arterial and mixed venous blood samples were withdrawn for the measurement of PaO2, PaCO2 and arterial lactate concentrations. Arterial oxygen delivery index and oxygen consumption index were calculated from standard formulas. Urine samples were collected to assess urine output volume and creatinine clearance.
Gastric mucosal parameters
Gastric mucosal perfusion was evaluated by a laser-Doppler technique flowmeter (Periflux System 5000, Perimed, Stockholm, Sweden), using a gastric probe for the measurement of GMP (P 424, Perimed, Stockholm, Sweden), and by tonometer (Tonocap, Datex-Ohmeda Division Instrumentarium, Helsinki, Finland) allowing measurement of gastric mucosal PCO2.
The gastric probe was inserted via the naso- or oro-gastric route. The correct position of the gastric probe in the lumen of the stomach was confirmed by X-rays. The laser-Doppler flowmetry signal was considered as reliable when pulse waves and respiratory synchronous fluctuation could be identified and were free of motion artefacts. The output signal from the flowmeter was continuously monitored on a computer using the Perisoft software (Perimed, Stockholm, Sweden). The software enabled the performance of continuous monitoring as well as the acquisition and processing of the laser-Doppler signal for the duration of the protocol, with a period of 240 s at each set of measurements to average the laser-Doppler flowmetry values over this period.
Because the data of GMP were measured in arbitrary units (perfusion units: PU), the results were expressed as a percentage of change between the reference value, defined as the value at the baseline, and each measurement. This was calculated according to the following formula: GMP % = (measured value – baseline value / baseline value). In addition, we calculated the ratio between the absolute value of GMP and DO2 (systemic oxygen delivery), which may be considered as reflecting the fraction of total red cell flux perfusing gastric mucosa [14].
We measured gastric mucosal PCO2 using a naso-gastric tonometer. The tonometer was inserted via the naso-gastric route and its position in the stomach was confirmed by X-rays. The gradient between gastric mucosal and arterial PCO2 (ΔPg-aCO2) was calculated as gastric mucosal PCO2 minus arterial PCO2. Enteral feeding was discontinued during the study and vacuity was ensured by gastric aspiration. Histamine receptor antagonists were discontinued during the study [15].
Experimental protocol
An initial set of measurements were taken. Afterwards, patients received an intravenous bolus dose of 1 mg of vasopressin analogue, terlipressin. After the intravenous bolus dose of terlipressin and during the protocol, the pre-study vasopressor agent (norepinephrine) was titrated down to maintain MAP constant at a level determined by the attending intensive care physician. A continuous intravenous fluid infusion (hydroxyethyl starch 6%), at a starting dose of 70 ml/h, was performed to maintain PAOP constant during the protocol. All other medications were held constant, dobutamine infusion (5 µg/kg per min) was not adjusted and mechanical ventilator settings were not changed.
Measurements were performed at baseline and after the intravenous bolus dose of terlipressin: at 30 min, at 1 h, at 2 h and then every 2 h for a total of 10 h. At 24 h, at the end of the study period, a final set of measurements were obtained to complete the study. ΔPg-aCO2 was calculated at baseline and after the intravenous bolus dose of terlipressin: at 2 h and then every 2 h for a total of 10 h and after 24 h. Urine samples were collected at baseline, at 6 h, at 10 h and after 24 h to measure creatinine clearance. Lactate concentrations were measured at baseline, at 6 h, at 10 h and after 24 h.
Statistical analysis
All results are reported as means ± SD. In order to evaluate the behaviour of the variation over time of systemic, regional haemodynamic and oxygenation parameters and gastric mucosal parameters in the group studied, a Repeated Measures Analysis of Variance was performed for all the quantitative variables, considering ‘time’ as the ‘within’ factor with nine levels (baseline, 30 min, 1 h, 2 h, 4 h, 6h, 8 h, 10 h and 24 h). All statistical analyses were conducted using the “R” statistical package (version 1.7.0).
Results
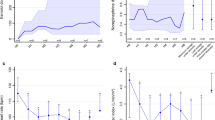
There were no complications associated with either the administration of terlipressin or the use of the laser-Doppler flowmeter and gastric tonometer. Data are summarised in Table 2 and Table 3 and shown in Figs. 1, 2and 3. For each patient no statistical differences were found at different data collection times for PAOP, pH, PaO2, PaCO2 and haemoglobin concentration during the protocol. This suggests that volume status and ventilatory support were maintained constant. In patients with peritonitis (n=5), intra-abdominal pressure was normal. As compared with baseline values, after the intravenous bolus dose of terlipressin the systemic vascular resistance and pulmonary vascular resistance increased significantly (p<0.05) over 30 min and for at least 24 h. By contrast, as compared with baseline, CO and HR were significantly lower (p<0.05) after 30 min from the intravenous bolus of terlipressin and lower values were found at each set of measurements. MAP, laser-Doppler GMP and the ratio of GMP to systemic oxygen delivery significantly increased (p<0.05) over 30 min and were sustained for at least 24 h.
Compared to baseline values, after the intravenous bolus dose of terlipressin, the ΔPg-aCO2 value was significantly lower (p<0.05) at 10 h and after 24 h, and arterial lactate concentrations were significantly lower (p<0.05) at 6 h, 10 h and after 24 h.
After 1 h, terlipressin administration significantly increased (p<0.05) urine output compared to baseline, and higher values were found at each set of measurements. The terlipressin-induced increase in urine output was associated with a significantly increased creatinine clearance (p<0.05). After the intravenous bolus dose of terlipressin, the norepinephrine infusion was progressively decreased from 0.7±0.05 µg/kg per min pre-study to 0.1±0.08 (p<0.05) at 24 h while maintaining the same MAP.
Discussion
In the present study, we demonstrated that the administration of an intravenous bolus dose of terlipressin in patients with norepinephrine-resistant septic shock increased the GMP, as assessed by laser-Doppler flowmetry, by increasing MAP.
Methodological consideration
The laser-Doppler flowmetry was closely correlated with other flow-measuring techniques [16, 17, 18]. However, with reference to data interpretation, it is important to take into account the limitations of laser-Doppler flowmetry. Firstly, the laser-Doppler measurements were recorded from a tissue area of only a few square millimetres (2–4 mm2) and at a 1 mm3 penetration depth, (tissue volume) using a 780 nm laser diode with 250 µm separation between optical fibres. A second limitation is the difficulty of maintaining optical coupling between the laser-Doppler probe and gastric mucosa. This is particularly important because, for each set of measurements, it is necessary to ensure the study of the same tissue volume.
However, considering its technical features and as observed by others authors [19], the P 424 probe detects perfusion of gastric mucosa. Furthermore, the weight and the dimension of the tip of the P 424 probe make it possible to maintain the probe in a stable position in the gastric lumen for the duration of the protocol. Continuous monitoring of the laser-Doppler signal on a personal computer using the Perisoft software in the 15 patients of the protocol showed no loss of contact between the tip of the probe and the gastric mucosa. Finally, ΔPgaCO2 was not calculated at 30 min and at 1 h, to avoid any measurement errors associated with the intragastric balloon equilibration times.
Systemic haemodynamic and gastric mucosal parameters
Vasopressor treatments play an important role in the therapeutic management of severe septic shock. Vasodilatation and vascular hyporeactivity to conventional treatment with high-dose norepinephrine often result in resistant hypotension. Vasopressin, an endogenous hormone produced in the hypothalamus, is released in response to hypovolaemia and hypotension. In fact, plasma concentrations of vasopressin were significantly higher during cardiogenic and hypovolaemic shock [20, 21, 22, 23, 24]. These high concentrations maintain arterial blood pressure through the activation of V1a receptors on vascular smooth muscle [21, 23] producing potent vasoconstriction. The discovery made by Landry and co-workers [1, 2] of the vasopressin deficiency and hypersensitivity in septic shock in humans provided the rationale for the use of vasopressin in severe septic shock [25]. However, discontinuation of vasopressin results in rapid hypotension, requiring immediate resumption of the treatment or increase in norepinephrine [11].
It is unclear whether terlipressin is harmful to the splanchnic circulation in septic shock. In our study, after a bolus dose of terlipressin, despite the restoration of MAP, we observed a significant fall in cardiac index due to a decrease in heart rate since the systolic ejection volume did not change; this result is not in accordance with previous findings [1, 2]. The fall in CO, associated with the potent vasoconstriction [26, 27, 28, 29] after vasopressin or terlipressin administration, could cause or at least worsen sepsis-related alterations in organ function. However, patients with severe septic shock generally have high CO and low systemic resistances. In all the patients enrolled in our study we observed a high CO at baseline: after 30 min from terlipressin administration we observed an increase in MAP and a decrease in CO. Since these findings were not associated with modifications in RAP and PAOP, the fall in CO may be related to a blood flow redistribution effect of terlipressin.
It is not known whether the terlipressin-induced shift in blood flow from muscle, skin and gut towards brain and myocardium has deleterious effects for the splanchnic region and whether this may lead to multiple organ failure once spontaneous circulation has been re-established. This terlipressin-induced redistributive effect could be beneficial only when the fall in CO is limited by the presence of the high-output state characterising severe septic shock. In this case, as shown in our study, terlipressin increased MAP without producing harmful effects on systemic haemodynamics. The key role of the high-output state is in accordance with the work of Asfar and colleagues; in their study, they observed improved splanchnic haemodynamics without any detrimental effects on ileal micro-circulation in a fluid-challenged endotoxic rat model [30] and this suggests that high CO was maintained despite the increase in MAP. The main finding of our study is the significant increase in GMP, despite the fall in CO, observed after the intravenous bolus dose of terlipressin. This hypothesis of an increase in the fraction of total red cell flux perfusing the gastric mucosa is also supported by the significantly high ratio between GMP and DO2 observed after terlipressin administration.
The preliminary study of Auzinger and co-workers showed a rise in ΔPg-aCO2 over 72 h [31]. In their preliminary study, Klinzing and colleagues showed a similar result in 12 septic patients [32]. In our protocol we observed a decrease in ΔPg-aCO2 at 8 h, at 10 h and at 24 h.
The lack of early significant changes in mucosal hypercarbia, despite the observed rapid changes in GMP, might be related to the severity of our patients’ illnesses or, as has been reported by previous studies, by a malperfusion in gastric and intestinal mucosa. An increase in mucosal oxygen availability should induce simultaneously a decrease in anaerobic CO2 production, an increase in mucosal venous CO2 washout and a restoration of aerobic metabolism. This could limit the magnitude of the decrease in mucosal hypercarbia due to the decrease in anaerobic CO2 production and to the increase in CO2 washout [33]. In addition, during gastric mucosal hypoxia states, modification of ΔPg-aCO2 and gastric mucosal blood flow could not be present at the same time. Hence, the initial ΔPg-aCO2 response to a rapid increase in mucosal blood perfusion could be limited if compared with GMP evaluated by laser-Doppler technique.
The additional finding of the study is that the administration of terlipressin increased urine output and creatinine clearance. Vasopressin and its analogue terlipressin, increase resistance in efferent glomerular arterioles but have no effect on afferent glomerular arterioles. Hence, for the same MAP, replacement of norepinephrine with terlipressin may result in increased perfusion pressure and in an elevated glomerular filtration rate because of the beneficial vasoconstriction of efferent arterioles and the relative vasodilatation of afferent arterioles [34].
Finally, high-dose norepinephrine has several potential side effects, including increased tissue oxygen demand [35] and decreased renal and mesenteric blood flow [36]. Thus, it is conceivable that the principle of removing or decreasing the high dose of vasopressor agents as promptly as possible in the presence of adequate blood pressure may limit the potential side effect without compromising organ perfusion. After a single bolus of terlipressin, all patients included in our study showed an increase in MAP, allowing reduction of high-dose norepinephrine, that was sustained at least 24 h, as was observed in previous studies [37]. Like O’Brien and co-workers [38], we are not able to explain the efficacy of a single bolus of terlipressin in our patients. This could be partially explained by the fact that a single dose might restore vascular reactivity and the sensitivity to endogenous and exogenous catecholamine. Another hypothesis could be the marked increase in serum arginine vasopressin (AVP) levels after bolus dosing in contrast to a continuous infusion. As reported in the recent paper by Sharshar and co-workers, plasma vasopressin levels almost always increase in the initial phase of septic shock and decrease afterwards. Relative vasopressin deficiency is seen in approximately one-third of late septic shock patients [39]. However, this aspect remains open to speculation, and the serum AVP levels before and after the treatment with terlipressin should be addressed in further studies.
This study has a number of limitations. Firstly, we did not investigate a control group because terlipressin administration was considered as a therapy of last resort and we chose to focus our attention on indices of haemodynamic stability and measures of organ perfusion. Since it is an open label design with no control group, we cannot be sure that the observed effects are only the consequence of the administration of terlipressin or, in part, a time-effect with favourable evolution of the patients. Thus, these data do not address the issue of whether terlipressin increases survival of in patients with septic shock compared with conventional catecholamine therapy. Secondly, our sample size was limited to 15 patients. We chose this sample size to address adequately the current physiological hypotheses. A much larger sample size will be required to demonstrate a survival benefit.
In conclusion, our study showed that administration of an intravenous bolus dose of terlipressin to patients with norepinephrine-treated septic shock increases GMP as assessed by laser-Doppler flowmetry. This result could be explained by a positive redistribution effect of CO on hepatosplanchnic macro- and micro-circulation, resulting in an increase of blood flow towards mucosa. An important effect of a bolus dose of terlipressin may be that it reduces the norepinephrine dose and thereby reduces the detrimental effects of high-dose norepinephrine. Terlipressin spares conventional vasopressor use in septic shock without compromising organ perfusion. Our findings provide evidence that the fall in CO in the high-output state after terlipressin is entirely in keeping with the increase in blood pressure achieved and is a positive response during severe septic shock. A properly powered, randomised, controlled trial with survival as primary end point, is required.
References
Landry DW, Levin HR, Gallant EM, Seo S, D’Alessandro D, Oz MC, Oliver JA (1997) Vasopressin pressor hypersensivity in vasodilatatory septic shock. Crit Care Med 25:1279–1282
Landry DW, Levin HR, Gallant EM, Asthon RC Jr, Seo S, D’Alessandro D, Oz MC, Oliver JA (1997) Vasopressin deficiency contributes to the vasodilatation of septic shock. Circulation 95:1122–1125
Chernow B, Roth B (1986) Pharmacologic manipulation of the peripheral vasculature in septic shock: clinical and experimental approaches. Circ Shock 18:141–155
Schaller MD, Waeber B, Nusseberger Brunner HR (1985) Angiotensin I, vasopressin and sympathetic activity in conscious rats with endotoxemia. Am J Physiol 18:H1086-H1092
Hollenberg SM, Tangora JJ, Piotrowsky MJ, Easington C, Parrillo JE (1997) Impaired micro-vascular vasoconstrictive responses to vasopressin in septic rats. Crit Care Med 25:869–873
Wilson MF, Brackett DJ, Hinshaw LB, Tompkins P, Archer LT, Benjamin BA (1981) Vasopressin releasing during sepsis and septic shock in baboons and dogs. Surg Gynecol Obstet 153:869–872
Brackett DJ, Schaefer CF, Tompkins P, Fragaeus L, Peters LG, Wilson MF (1985) Evaluation of cardiac output, total peripheral resistances and plasma concentrations of vasopressin in the conscious, unrestrained rat during endotoxemia. Circ Shock 17:273–284
Egan JW, Jugus M, Kinter LB, Lee K, Smith EF (1989) Effect of a selective vasopressin receptor antagonist on the sequelae of endotoxemia in the conscious rat. Circ Res 29:155–166
Malay MB, Asthon RCJ, Landry DW, Townsend RN (1999) Low-dose vasopressin in the treatment of vasodilatatory septic shock. J Trauma 47:699–705
Heyndrickx GR, Boettcher DH, Vatner SF (1976) Effects of angiotensin, vasopressin and methoxamine on cardiac function and blood flow distribution in conscious dogs. Am J Physiol 231:1579–1587
Tsuneyoshi I, Yamada H, Kakihana Y, Nakamura L, Nakano Y, Boyle WA (2001) Haemodynamic and metabolic effects of low dose vasopressin infusions in vasodilatatory septic shock. Crit Care Med 29:487–493
Bernadich C, Bandi JC, Bosch J (1988) Effects of F-180, a new selective vasoconstrictor peptide compared with terlipressin and vasopressin on systemic and splanchnic haemodynamics in rat model of portal hypertension. Hepatology 27:351–356
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101:1644–1655
Duranteau J, Sitbon P, Teboul JL, Vicaut E, Anguel N, Richard C, Samii K (1999) Effects of epinephrine, norepinephrine or combination of norepinephrine and dobutamine on gastric mucosa in septic shock. Crit Care Med 27:893–900
Parvianen I, Vaisanen O, Ruokonen E, Takala J (1996) Effect of nasogastric suction and ranitidine on the calculated gastric intramucosal pH. Intensive Care Med 22:319–323
Kvietys PR, Shepherd AP, Neil Granger D (1985) Laser-Döppler, H2 clearance and microsphere estimates of mucosal blood flow. Am J Physiol 249:G221-G227
Nicholson CD, Schmitt RA, Wilke R (1985) The effect of acute and chronic femoral artery ligation on the blood flow through the gastrocnemius muscle of the rat examined using laser-Doppler flowmetry and Xenon133 clearance. Int J Microcirc Clin Exp 4:151–171
Oberg A (1990) Laser-Doppler flowmetry. Biomedical Engineering 18:125–163
Krohg-Sorensen K, Line PD, Kvernebo K (1993) The significance of probe design in evaluation of colonic perfusion with laser-Doppler flowmetry. Scand J Gastroenterol 28:381–386
Abboud FM, Floras JS, Aylward PE, Guo GP, Gupta BN, Schmid PG (1990) Role of vasopressin in cardiovascular and blood pressure regulation. Blood Vessels 27:106–115
Schwartz J, Reid IA (1981) Effect of vasopressin blockade on blood pressure regulation during hemorrhage in conscious dogs. Endocrinology 109:1778–1780
Laslo FA, Laslo F Jr, De Wied D (1991) Pharmacology and clinical perspective of vasopressin antagonists. Pharmacol Rev 43:73–108
Minaker KL, Meneilly GS, Youn GJ, Landberg L, Stoff JS, Robertson GL, Rowe JW (1991) Blood pressure, pulse and neurohumoral responses to nitroprusside-induced hypotension in normotensive aging men. J Gerontol 46:M151–154
Schrier RW, Berl T, Anderson RJ (1979) Osmotic and non osmotic control of vasopressin release. Am J Physiol 236:F321-F332
Holmes CL, Patel BM, Russell JA, Walley KR (2001) Physiology of vasopressin relevant to management of septic shock. Chest 120:989–1002
Iwao T, Toyonaga A, Oho K, Shigemori H, Sakai T, Tayama C, Masumoto H, Sato M, Tanikawa K (1996) Vasopressin plus oxygen vs vasopressin alone in cirrhotic patients with portal-hypertensive gastropathy: effects on gastric mucosal haemodynamics and oxygenation. J Gastroenterol Hepatol 11:216–222
Laszlo F, Karacsony G, Pavo I, Varga C, Rojik I, Laszlo FA (1994) Aggressive role of vasopressin in development of different gastric lesions in rats. Eur J Pharmacol 258:15–22
Montani JP, Liard JF, Schoun J, Mohring J (1980) Haemodynamic effects of exogenous and endogenous vasopressin at low plasma concentrations in conscious dogs. Circ Res 47:346–355
Undesser KP, Hasser EM, Haywood JR, Johonson AK, Bishop VS (1985) Interactions of vasopressin with the area postrema in arterial baroreflex function in conscious rabbits. Circ Res 56:410–417
Asfar P, Pierrot M, Veal N, Moal F, Oberti F, Croquet V, Douay O, Gallois Y, Saumet JL, Alquier P, Cales P (2003) Low-dose terlipressin improves systemic and splanchnic haemodynamics in fluid-challenged endotoxic rats. Crit Care Med 31:215–220
Auzinger GM, O’Callaghan PG, Harry RA (2002) Terlipressin in the treatment of the catecholamine resistant septic shock (abstract). Crit Care 6:61
Klinzing S, Schiergens V, Reinhart K (2002) Could vasopressin be an alternative for vasopressor therapy in sepsis? (abstract) Eur J Anaesthesiol 19:169–170
Russel JA (1997) Gastric tonometry: does it work? Intensive Care Med 23:3-6
Edwards RM, Trizna W, Kinter LB (1989) Renal effects of vasopressin and vasopressin antagonists. Am J Physiol 256:F274–278
Schreuder WO, Schneider AJ, Groeneveld AB, Thijs LG (1989) Effect of dopamine vs norepinephrine on haemodynamics in septic shock: emphasis on right ventricular performance. Chest 95:1282–1288
Bomzon L, Rosendorff C, Scriven DR, Farr J (1975) The effect of noradrenaline, adrenergic blocking agents and tyramine on the intrarenal distribution of blood flow in the baboon. Cardiovasc Res 9:314–322
Patel BM, Chittok DR, Russel JA, Walley KR (2002) Beneficial effects of short-term vasopressin infusion during severe septic shock. Anaesthesiology 96:576–582
O’Brien A, Clapp L, Singer M (2002) Terlipressin for norepinephrine-resistant septic shock. Lancet 359:1209–1210
Sharshar T, Blanchard A, Paillard M, Raphael JC, Gajdos P, Annane D (2003) Circulating vasopressin levels in septic shock. Crit Care Med 31(6):1752–1758
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was funded by an independent research grant from the Department of Anaesthesiology and Intensive Care of the University of Rome “La Sapienza”.
Rights and permissions
About this article
Cite this article
Morelli, A., Rocco, M., Conti, G. et al. Effects of terlipressin on systemic and regional haemodynamics in catecholamine-treated hyperkinetic septic shock. Intensive Care Med 30, 597–604 (2004). https://doi.org/10.1007/s00134-003-2094-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-2094-3