Abstract
Objective
The diaphragmatic pressure-time product (PTPdi) has been used to quantify the loading and unloading of the diaphragm. The validity of the relationship between PTPdi and diaphragm electrical activity (EMGdi) during pressure-support ventilation (PSV) is unclear. We examined this relationship.
Design and setting
Physiological study in a physiology laboratory.
Subjects
Six healthy adults.
Interventions
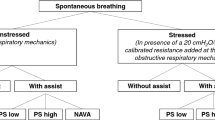
Spontaneous breathing (SB) and two levels of PSV (6 and 12 cmH2O), breathing room air and incremental concentrations of carbon dioxide, sufficient to achieve an EMGdi signal of approximately 200% of baseline value.
Measurements and results
We measured the electrical (EMGdi) and mechanical (PTPdi) activity of the diaphragm using oesophageal electrode and oesophageal and gastric balloon catheters. The relationship between EMGdi and PTPdi during SB was linear in five subjects and curvilinear in one. However, with PSV 12 cmH2O we observed that the relationship between EMGdi and PTPdi was ‘left shifted’; specifically, for any given level of EMGdi the PTPdi was smaller with PSV 12 cmH2O than during SB. However, when PTPdi was converted to power (the product of pressure and flow) the tendency to left shift was largely reversed.
Conclusions
We conclude that when assessing of diaphragm unloading during PSV flow measurements are required. Where flow is constant, PTPdi is a valid measure of diaphragm unloading, but if not these data may be used to make an appropriate correction.
Similar content being viewed by others
Introduction
The function of ventilatory assistance is to unload the respiratory muscles. Inspiratory pressure-support ventilation (PSV) is a form of partial ventilatory support which can be used effectively in a non-invasive manner in spontaneously breathing patients in a variety of clinical situations [1]. Quantification of the magnitude of diaphragm unloading can be achieved in two ways. The first is by measuring the mechanical force developed by the diaphragm during inspiration, which in vivo is represented by transdiaphragmatic pressure (Pdi). The diaphragmatic pressure-time product (PTPdi), an estimate of oxygen consumption of the respiratory muscles [1, 2, 3], has been used for this purpose. A second approach is to evaluate neuromuscular excitation by measuring the electrical activity of the diaphragm (EMGdi) [4]. Although EMGdi is one step closer to the central motor output than PTPdi (and would therefore possibly be a more accurate measure of diaphragmatic activity), in practice PTPdi is more often used because of the technical problems associated with accurately measuring EMGdi.
Theoretically several factors could modify the relationship between EMGdi and PTPdi [5, 6, 7, 8] so that despite unloading the respiratory muscles PSV could lead to a relatively small or even non-existent reduction in tension generation. In fact, clinical data suggest that PTPdi has a close relationship with EMGdi [9, 10]. However, in these studies only small variation in mean inspiratory flow occurred, and therefore the effects of flow rate are presently uncertain. In particular, this relationship has not been analysed during PSV which is a mode characterized by a high inspiratory flow. To test the hypothesis that flow influences the in vivo measurements of PTPdi and EMGdi we studied normal subjects during both spontaneous breathing (SB) and PSV at rest and in response to carbon dioxide (CO2) stimulation to generate increased inspiratory flow.
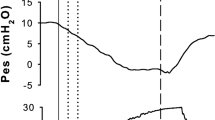
Methods
We studied six subjects, seated upright and breathing through a mouthpiece with a nose clip in place. Flow was measured using a pneumotachograph head (Hans Rudolph 3700 series, Hans Rudolph, Kansas City, Mo., USA) connected to a CS5T electrospirometer (GM Instruments, UK). The signal was processed to provide breath-to-breath computation of minute ventilation (Ve) and tidal volume (Vt). Airway pressure (Paw) was measured with a differential pressure transducer (MP 45 model, Validyne, Northridge, Calif., USA) connected to the mouthpiece. Expired CO2 (PetCO2) was measured at the mouth by a capnograph (PK Morgan, Gillingham, UK). The inspired CO2 (FICO2) was measured by a second capnograph (Hewlett Packard, Waltham, Mass., USA) and sampled in another computer (Macintosh Centris computer) running Labview 2 software (National Instruments, Austin, Tex., USA). Oesophageal pressure (Pes) and gastric pressure (Pgas) was measured in a standard fashion (see [11, 12, 13]). The EMG signal was recorded using a conventionally placed oesophageal electrode catheter [14]. This consisted of three coils each 1 cm wide and separated by a distance of 3 cm from one another. The top coil was connected to ground, and the lower two coils formed the electrode pair. The oesophageal and gastric balloon-catheters and the EMG electrode were then marked and firmly fixed on the subject’s nose. The EMG signal was amplified, band pass filtered in the range 50 and 2000 Hz, rectified and integrated with a time constant of 100 ms. These signals passed to a 12-bit analog-to-digital converter (NB-MIO-16; National Instruments) and displayed in real time and stored on a MacIntosh Power PC computer (Apple Computers, Cupertino, Calif., USA) running Labview 4.1 software (National Instruments).
Experimental protocol
Three epochs were studied. Period 1 was a period of SB. During this period the subject breathed through the pneumotachograph head with the ventilatory circuitry disconnected. Periods 2 and 3 were two periods of PSV with a constant inspiratory pressure of 6 or 12 cmH2O applied in random order and separated by 15 min of SB on air. PSV was supplied using a commercially available ventilator (Onyx, Mallinckrodt, UK). The trigger sensitivity was set at its minimal level, i.e. setting the maximal sensitivity without auto-triggering (−0.4 to −0.7 cmH2O). The initial flow rate was set at the maximal value to reach the preset pressure plateau. Expiration was free and initiated when the expiratory flow reached 30% of the peak inspiratory flow. The back up respiratory rate was set at its lowest value, i.e. four per minute, to ensure that the subject triggered all breaths. No positive end-expiratory pressure (PEEP) was added.
Each of these three periods started with a baseline period, which was composed of 5 min of quiet breathing room air. We then induced hyperventilation by adding CO2 after the baseline period. CO2 was added to oxygen (at a flow rate of 5 l/min) distal to the pneumotachograph head at the mouthpiece during SB or into the inspiratory circuit during the two PSV periods and the CO2 flow rate was adjusted to obtain an initial FICO2 of 2%. The FICO2 was increased by approximately 2% every 2 min until the EMGdi signal increased to a level of around 200% (as observed during the run) of the baseline value while breathing room air. The duration of the CO2 loading lasted between 3.6 and 9.3 min.
Data analysis
The last 2 min of the room air periods were used only to ensure that there was adequate stabilization of the breathing pattern. The changes that occurred during the CO2 inhalation periods were analysed continuously and are reported here. Breaths in which contamination occurred (e.g. from oesophageal peristalsis) were discarded; these accounted for 2.2% of the total.
Pressure generation and integrated EMGdi signal were analysed breath by breath. For both signals the start and the end of inspiration was determined using the flow signal to determine the start and the end of inspiration. Similarly the baseline for PTPdi was considered to be the resting end expiratory Pdi whilst for EMGdi the baseline was considered to be zero. To calculate PTPdi and EMGdi the areas subtended by the pressure-time curve and integrated rectified EMGdi curves, respectively, and the baseline was determined for each breath and had units of cmH2O/s and au/s, respectively. In line with convention, the values so obtained are expressed per minute by multiplication by (Ti/Ttot)×60. Further details with regard to practical calculation of PTPdi are presented elsewhere [13].
We also measured Vt, Ve, total breath cycle duration (Ttot), inspiratory time (Ti) and inspiratory time/total breath cycle duration ratio (Ti/Ttot), peak inspiratory flow (Vi-peak) and mean inspiratory flow (Vt/Ti) throughout the run. The data were subjected to graphic analysis.
Results
Effect of PSV on the breathing pattern
Representative traces from one individual are shown in Fig. 1. For the period of CO2 loading we observed that median Vt, Ve, Vt/Ti, and Vi-max for most individuals were higher during the two levels of PSV than during SB (Table 1). The impact of PSV on breathing was assessed visually using graphs for each subject of breathing outcomes across breaths for each treatment type. In the case of PTPdi levels were higher during SB than during PSV 12 in four of six subjects with overlap in the remaining two. Differences between the two levels of ventilation were generally smaller than differences with SB. Similarly, in the case of EMGdi peak values obtained were higher in three of the six patients during SB than during PSV and similar in two of the remaining subjects. Basal levels of EMGdi were lower during PSV than SB in three of six subjects. For all subjects PTPdi was virtually always lower during PSV than SB at any given level of EMGdi, demonstrating that PSV disproportionately suppresses PTPdi rather than EMGdi
Ttot did not vary greatly between treatments for most subjects; however, there was one individual in whom Ttot was visibly longer during 12 cmH2O PSV throughout the CO2 inhalation and another in whom this was the case during the first part of PSV 12 cmH2O. There were also two subjects for whom Ttot was shorter during SB than during PSV. There was no clear trend across subjects for the proportion of time for each breath spent inspiring (Ti/Tot) to be higher or lower during any particular run. Tidal volume (Vt) tended to be greater during PSV, and in two subjects there was a clear dose-response relationship such that peak inspiratory flow was highest during 12 cmH2O PSV and lowest during SB.
Relationship between the EMG activity and the breathing pattern
For each subject the change between first and last breaths during CO2 loading was measured to assess how breathing outcomes varied during this period. During SB the median change in Vt was 30.7% and during PSV 6 and PSV 12 it was 13.9% and −9.3%, respectively. In the case of Ve, the median change during SB was 28.4%, 23.7% during PSV 6, and 19.7% during PSV 12.
The relationship between PTPdi and EMGdi during CO2 loading
The primary goal of our study was to assess whether the relationship between PTPdi and EMGdi during SB differs from that during PSV, especially when flow is increased. We initially attempted to subject the data to statistical analysis. In brief, we first proposed that a linear regression model of EMGdi against PTPdi be constructed for each treatment type (i.e. SB and the two PSV levels) and the estimated intercepts and slopes for the three models compared to assess differences. An appropriate model was the generalized estimating equation (GEE) with Gaussian error and identity link that would control for the correlation structure within individuals and also include a ‘subject’ parameter to control for between-subject variability. Inspection of EMG data for each treatment type by q-q plot revealed that they were not normally distributed, and several transformations were explored. The log-transformation provided the most visibly normal results, but tests for kurtosis and skewness indicated non-normality, and the resulting association with PTP was not linear. A final transformation of EMG involved averaging across the first ten breaths for each individual, re-coding this mean as 100%, and expressing each subsequent breath as a percentage of this mean. The resulting data were not normally distributed, and there were no transformation of EMG that rendered data from each treatment normal and linearly associated with PTP.
Based on these findings it was decided that it was not appropriate to use a linear regression model to assess the relationship between PTPdi and EMGdi, and therefore graphic techniques were employed instead. These analyses involved producing two-way scatter-plot diagrams for each individual that distinguished between SB and the highest level of ventilation (12 cmH2O PSV). It was decided to ignore the 6 cmH2O PSV data in this graphic analysis since it was difficult to interpret the graphs with so many data series (average number of data points per person 287). The resulting graphs (Fig. 2) show that with PSV 12 cmH2O the relationship between EMGdi and PTPdi was ‘left shifted’; specifically, at any given value of EMGdi the PTPdi values were less for PSV 12 cmH2O than SB. This pattern was seen in all subjects but was most extreme in subjects 2, 3 and 4.
Individual data of the relationship between diaphragmatic pressure-time product (PTPdi) and electromyography (EMGdi) per breath in each subject during spontaneous breathing (SB; closed circles) and inspiratory pressure support ventilation at 12 cmH2O (open circles). Vertical axis EMGdi expressed in arbitrary units; horizontal axis pressure-time product. The axes are adjusted for each individual to use the full width and height of the graph. In all subjects for a given level of EMGdi there is a reduction in PTPdi per breath during PSV at 12 cmH2O
To evaluate the effect of velocity of contraction we introduced peak inspiratory flow to the relationship between PTPdi and EMGdi. Figure 3 shows the relationships between EMGdi and the pressure flow product (PTPdi×Vi-max). It is apparent that the plots of PSV 12 cmH2O and SB are brought much closer together and with the exception of subject 3 (who had the greatest visible separation between PSV 12 cmH2O and SB before flow correction) are overlapping and in some cases (subjects 5 and 6) effectively superimposed. Similar results were obtained by correction with the related variables tidal volume and minute ventilation.
Individual data of the relationship between diaphragmatic pressure-time product (PTPdi) multiplied by peak inspiratory flow (in litres) and electromyography (EMGdi) per breath in each subject, during spontaneous breathing (SB; closed circles) and inspiratory pressure support ventilation at 12 cmH2O (open circles). Vertical axis EMGdi expressed in arbitrary units; horizontal axis pressure-time flow product. In all but one subject (no. 3) PSV 12 cmH20 and SB are now overlapping and in some cases are effectively superimposed
Discussion
The main finding of this study is that the association between EMGdi and PTPdi is altered by the application of PSV such that at any given level of EMGdi PTPdi is reduced. Accordingly, the decrease in EMGdi would be underestimated if the association between EMGdi and PTPdi during SB were extended to estimate EMGdi by measuring PTPdi during PSV; specifically, a fall in PTPdi during PSV is not an accurate reflection of the fall in EMGdi. However, this underestimation of the fall in EMGdi is corrected if the product of pressure and inspiratory flow is used to estimate the mechanical output of the diaphragm, indicating that in situations of high inspiratory flow, pressure and timing of diaphragm contraction are less predictive of the diaphragm load.
Critique of the method
Criticism and limits of the EMG
EMGdi represents the “gold standard” for evaluating the neuromuscular activity of the diaphragm, but several technical difficulties can limit its value. The first is the position of the oesophageal electrode catheter. It is essential to locate the oesophageal electrode optimally to record a maximal signal. During spontaneous quiet breathing in healthy humans the signal can be small. For this purpose the position of the electrode was checked regularly between each period, asking the subject to breathe deeply, which produced a substantially larger signal.
The decrease in EMGdi during PSV could theoretically be partially due to the displacement of the electrode by a modification of the curvature and the position of the diaphragm as a result of the lung volume change induced by the applied positive pressure. However, we have demonstrated that the size of the signal obtained from our electrode is not significantly affected by the magnitude of lung volume change that can be expected from PSV [15]. Moreover, since data show that PTPdi is reduced more than EMGdi during PSV, such a mechanism would only serve to emphasize the validity of our conclusions.
Criticisms and limits of the PTP
The pressure-time product could be subject to error as a result of the force-length relationship of skeletal muscle since increased lung volume results in a reduction in the tension generating capacity of the diaphragm [7, 12, 16]. However, we doubt whether this mechanism can explain our findings because in the absence of externally applied PEEP or airflow limitation there is no physiological reason to suspect a significant change in end-expiratory lung volume. This assumption is supported by direct observation that end-expiratory oesophageal pressure was constant in all subjects throughout the study.
Significance of the findings
Our study confirms that EMGdi has a close linear relationship with PTPdi during SB. In addition, these findings build on published data which were obtained at relatively low inspiratory flow rates [9, 10] by demonstrating a change in the relationship between EMGdi and PTPdi when inspiratory flows are increased. We acknowledge that a weakness of the present study is that it was performed in the laboratory rather than in critically ill patients; nevertheless this allowed us to assess PTPdi and EMGdi over a greater range of drive than might be easily feasible in ventilated patients.
In fact, the relationship between EMGdi and PTPdi remains linear, but there is a greater reduction in PTPdi relative to the reduction in EMGdi during PSV presumably as a consequence of the force-velocity relationship increasing the velocity of contraction with increasing flow rates results in a reduction in force. The present findings are consistent with animal data which show that the pressure developed by the diaphragm decreases with increasing inspiratory flows [17] as a result of the force-velocity relationship of the diaphragm [7]. At least three human studies support the data from the present study [18, 19, 20], but none of these studies evaluated PSV which had not then entered clinical practice. Nava et al. [21] recorded EMGdi and PTPdi in seven patients with chronic obstructive pulmonary disease who were recovering from acute exacerbations requiring PSV. Their data did not directly address our hypothesis, but it is evident from the figure that whereas the addition of PEEP results in a reasonably consistent reduction in PTPdi, there is a smaller and more variable reduction in EMGdi.
One of the main characteristics of PSV is a high inspiratory flow at the beginning of inspiration, which has been demonstrated to affect the respiratory output [22]. Data from Bonmarchand et al. [23] who studied intubated patients with chronic obstructive pulmonary disease are consistent with ours in that the inspiratory work of breathing and the EMGdi were well correlated despite alterations in inspiratory flow. The question arises whether alternative surrogates for the velocity of shortening could be employed; for example, in a previous study in children with cystic fibrosis [22] the level of Vt/Ti did not differ significantly during PSV and assist control/volume cycled ventilation (AC/VC) compared to SB. In contrast, Vi-max differed significantly between SB and the two modes of ventilation, being significantly higher during PSV. Thus the product of PTPdi and Vi-max was considered to be the most appropriate calculation.
Many investigators, including ourselves [11, 24], have used PTPdi to evaluate loading and unloading of the diaphragm since non-invasive PSV has become more widely available. However, PTPdi may not accurately reflect the unloading of the diaphragm as compared to EMGdi during PSV unless flow is constant. Nevertheless the data from the present study were also analysed graphically using Vt and Ve, and the results were satisfactory, suggesting that these could also be used as correction factors. We caution that the present conclusions should be tested during other modes of ventilatory assistance, such as AC/VC, as well as in a variety of disease states.
In conclusion, we believe that our study has a number of potentially important clinical implications, although we appreciate these were not directly tested. Firstly, this study supports the strong relationship between EMGdi and PTPdi during SB in normal healthy subjects (linear in five of six subjects and curvilinear in the sixth). However, during PSV there is a ‘left-shift’ of this relationship, such that at any given level of EMGdi PTPdi is reduced. Nevertheless, this inaccuracy can be largely corrected in practice by the addition of inspiratory flow into the pressure analysis. These observations highlight the importance of integrating flow and possibly analysing work of breathing, rather than PTPdi, when assessing the loading or unloading of the respiratory muscles during PSV.
References
Brochard L, Pluskwa F, Lemaire F (1987) Improved efficacy of spontaneous breathing with inspiratory pressure support. Am Rev Respir Dis 136:411–415
Rochester DF, Bettini G (1976) Diaphragmatic blood flow and energy expenditure in the dog. J Clin Invest 57:661–672
Soust M, Walker AM, Berger PJ (1989) Diaphragm VO2, diaphragm EMG, pressure-time product and calculated ventilation in newborn lambs during hypercapnic hyperpnoea. Respir Physiol 76:107–118
Sinderby C, Navalesi P, Beck J, Skrobik Y, Comtois N, Friberg S, Gottfried SB, Lindstrom L (1999) Neural control of mechanical ventilation in respiratory failure. Nat Med 5:1433–1436
Bigland B, Lippold OCJ (1954) The relation between force, velocity and integrated electrical activity in human muscles. J Physiol (Lond) 123:214–224
Agostoni E, Sant’Ambrogio G, del Portillo Carrasco H (1960) Electromyography of the diaphragm in man and transdiaphragmatic pressure. J Appl Physiol 15:1093–1097
Pengelly LD, Alderson AM, Milic-Emili J (1971) Mechanics of the diaphragm. J Appl Physiol 30:797–805
Stainsby WN, Barclay JK (1972) Oxygen uptake for brief tetanic contractions of dog skeletal muscle in situ. Am J Physiol 223:371–375
Sassoon CSH, Light RW, Lodia R, Sieck GC, Mahutte CK (1991) Pressure-time product during continuous positive airway pressure, pressure support ventilation, and T-piece during weaning from mechanical ventilation. Am Rev Respir Dis 143:469–475
Beck J, Gottfried SB, Navalesi P, Skrobik Y, Comtois N, Rossini M, Sinderby C (2001) Electrical activity of the diaphragm during pressure support ventilation in acute respiratory failure. Am J Respir Crit Care Med 164:419–424
Kyroussis D, Polkey MI, Hamnegard CH, Mills GH, Green M, Moxham J (2000) Respiratory muscle activity in patients with COPD walking to exhaustion with and without pressure support. Eur Respir J 15:649–655
Polkey MI, Hamnegard C-H, Hughes PD, Rafferty GF, Green M, Moxham J (1998) Influence of acute lung volume change on contractile properties of the human diaphragm. J Appl Physiol 85:1322–1328
Hart N, Polkey M (2001) Investigation of respiratory muscle function. Clin Pulm Med 8:180–187
Luo YM, Polkey MI, Johnson LC, Lyall RA, Harris ML, Green M, Moxham J (1998) Diaphragm EMG measured by cervical magnetic and electrical phrenic nerve stimulation. J Appl Physiol 85:2089–2099
Luo YM, Lyall RA, Harris ML, Hawkins P, Hart N, Polkey MI, Moxham J (2000) Effect of lung volume on the oesophageal diaphragm EMG assessed by magnetic phrenic nerve stimulation. Eur Respir J 15:1033–1038
Grassino A, Goldman MD, Mead J, Sears TA (1978) Mechanics of the human diaphragm during voluntary contraction: statics. J Appl Physiol 44:829–839
Mognoni P, Saibene F, Sant’Ambrogio G, Agostino E (1968) Dynamics of the maximal contraction of the respiratory muscles. Respir Physiol 4:193–202
Goldman MD, Grassino A, Mead J, Sears TA (1978) Mechanics of the diaphragm during voluntary contraction: dynamics. J Appl Physiol 44:840–848
Collet PW, Perry C, Engel IA (1984) Pressure-time product, flow and oxygen cost of resistive breathing in humans. J Appl Physiol 58:1263–1272
Dodd DS, Kelly S, Collet PW, Engel IA (1988) Pressure-time product, work, rate, and endurance during resistive breathing in humans. J Appl Physiol 64:1397–1404
Nava S, Bruschi C, Rubini F, Palo A, Iotti G, Braschi A (1995) Respiratory response and inspiratory effort during pressure support ventilation in COPD patients. Intensive Care Med 21:871–879
Fauroux B, Pigeot J, Polkey MI, Isabey D, Clement A, Lofaso F (2001) In vivo physiologic comparison of two ventilators used for domiciliary ventilation in children with cystic fibrosis. Crit Care Med 29:2097–105
Bonmarchand G, Chevron V, Chopin C, Jusserand D, Girault C, Moritz F, Leroy J, Pasquis P (1996) Increased initial flow rate reduces inspiratory work of breathing in patients with exacerbation of chronic obstructive pulmonary disease. Intensive Care Med 22:1147–1154
Maltais F, Reissmann H, Gottfried SB (1995) Pressure support reduces inspiratory effort and dyspnea during exercise in chronic airflow obstruction. Am J Respir Crit Care Med 151:1027–1033
Author information
Authors and Affiliations
Corresponding author
Additional information
Brigitte Fauroux was supported by a grant from the Société de Pneumologie de Langue Française.
Rights and permissions
About this article
Cite this article
Fauroux, B., Hart, N., Luo, Y.M. et al. Measurement of diaphragm loading during pressure support ventilation. Intensive Care Med 29, 1960–1966 (2003). https://doi.org/10.1007/s00134-003-1941-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-1941-6