Abstract
Background
Several studies have suggested that excellent therapeutic outcomes can be achieved with conservative treatment of proximal humeral epiphyseal fractures in patients younger than 11 years old; however, the outcomes of conservative treatment for children older than 11 years are controversial. To address this problem, this study compared outcomes of conservative treatment for proximal humeral epiphyseal fractures in pediatric patients of different ages.
Methods
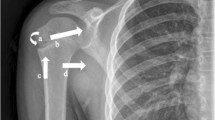
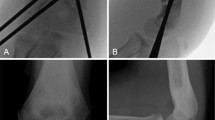
The patients were divided into two groups for comparative purposes based on age. Group I consisted of 34 patients who were less than 11 years old (average age: 5 years) and group II included 21 patients who were 11 years of age or older (average age: 14 years). Patients in both groups underwent conservative treatment and follow-up examination, where they first were examined with X‑radiography for assessment of deformity, fracture union and loss of reduction. At the final follow-up after 2 years, patients were assessed by an interview and a detailed physical examination including the assessment of shoulder function using the Constant-Murley score.
Results
There were no significant differences in the grading scale of varus deformity between the two groups (P > 0.05) after immediate postreduction X‑radiography; however, there were significant differences in the grading scale of varus deformity between group I and group II at the 2‑year follow-up (P < 0.05). There were no significant differences between the two groups with respect to the Constant-Murley score and arm length discrepancy (P > 0.05) at final follow-up examinations.
Conclusion
In general, the results suggested that the outcomes, as measured with radiographs, for both older and young children were comparable after immediate postreduction roentgenograms. For long-term follow-up there was a difference between the two groups and the degree of angulation and displacement might be associated with treatment outcomes for older children. Thus, these factors should be considered when treating and evaluating the outcomes for older children.
Zusammenfassung
Hintergrund
Mehrere Studien haben gezeigt, dass durch die konservative Behandlung proximaler humeraler epiphysärer Frakturen bei Patienten <11 Jahren exzellente therapeutische Ergebnisse erzielt werden können. Jedoch sind die Ergebnisse der konservativen Behandlung bei Kindern >11 Jahren kontrovers. Um dieses Problem zu adressieren, verglich man in dieser Studie die Ergebnisse der konservativen Behandlung proximaler humeraler epiphysärer Frakturen bei Kindern unterschiedlichen Alters.
Methoden
Gruppe I bestand aus 34 Patienten, die jünger als 11 Jahre waren (Durchschnittsalter 5 Jahre), und Gruppe II schloss 21 Patienten ein, die 11 Jahre oder älter waren (Durchschnittsalter: 14 Jahre). Die Patienten beider Gruppen erhielten eine konservative Behandlung sowie eine Follow-up-Untersuchung, bei der sie mittels Röntgenaufnahmen untersucht wurden, um Deformität, Frakturheilung und den Reduktionsverlust zu beurteilen. Beim letzten Follow-up nach 2 Jahren wurden die Patienten mittels eines Interviews und einer detaillierten körperlichen Untersuchung bewertet, einschließlich der Beurteilung der Schulterfunktion mittels Constant-Murley-Score.
Ergebnisse
Es gab keine signifikanten Unterschiede in der Klassifikationsskala für Varusdeformität zwischen den 2 Gruppen (p > 0,05) nach der sofortigen Röntgenaufnahme nach Reduktion. Jedoch gab es signifikante Unterschiede in der Klassifikationsskala für Varusdeformität zwischen Gruppe I und Gruppe II beim 2‑Jahres-Follow-up (p < 0,05). Hinsichtlich des Constant-Murley-Scores und der Armlängendiskrepanz (p > 0,05) wurden zwischen den beiden Gruppen bei der letzten Follow-up-Untersuchung keine signifikanten Unterschiede festgestellt.
Schlussfolgerung
Im Allgemeinen zeigten die Ergebnisse, dass die mittels Röntgenaufnahmen erfassten Outcomes sowohl bei älteren als auch bei jüngeren Kindern nach einer sofortigen Röntgenaufnahme nach Reduktion vergleichbar waren. Im Langzeit-Follow-up wurde ein Unterschied zwischen den beiden Gruppen festgestellt, und dass Angulationsgrad und Dislokation mit den Behandlungsergebnissen älterer Kinder assoziiert sein könnten. Daher sollten diese Faktoren bei der Behandlung und Evaluation der Ergebnisse älterer Kinder berücksichtigt werden.


Similar content being viewed by others
Abbreviations
- ADL:
-
Activities of daily living
- CRIF:
-
Closed reduction and internal fixation
- ED:
-
Emergency department
- ORIF:
-
Open reduction and internal fixation
- ROM:
-
Range of motion
References
Rose SH, Melton LJ 3rd et al (1982) Epidemiologic features of humeral fractures. Clin Orthop Relat Res 168:24–30
Baxter MP, Wiley JJ (1986) Fractures of the proximal humeral epiphysis. Their influence on humeral growth. J Bone Joint Surg Br 68(4):570–573
Larsen CF, Kiaer T, Lindequist S (1990) Fractures of the proximal humerus in children. Nine-year follow-up of 64 unoperated on cases. Acta Orthop Scand 61(3):255–257
Dameron TB, Reibel DB (1969) Fractures involving the proximal humeral epiphyseal plate. J Bone Joint Surg Am 51:289–297
Neer CS 2nd, Horwitz BS (1965) Fractures of the proximal humeral epiphysial plate. Clin Orthop Relat Res 41:24–31
Bahrs C, Zipplies S et al (2009) Proximal humeral fractures in children and adolescents. J Pediatr Orthop 29(3):238–242
Dobbs MB, Luhmann SL, Gordon JE et al (2003) Severely displaced proximal humeral epiphyseal fractures. J Pediatr Orthop 23:208–215
Chee Y, Agorastides I, Garg N et al (2006) Treatment of severely displaced proximal humeral fractures in children with elastic stable intramedullary nailing. J Pediatr Orthop B 15:45–50
Rajan RA, Hawkins KJ et al (2008) Elastic stable intramedullary nailing for displaced proximal humeral fractures in older children. J Child Orthop 2(1):15–19
Sherk HH, Probst C (1975) Fractures of the proximal humeral epiphysis. Orthop Clin North Am 6:401–413
Pritchett JW (1988) Growth and predictions of growth in the upper extremity. J Bone Joint Surg Am 70:520–525
Burgos-Flores J, Gonzalez-Herranz P, Lopez-Mondejar JA et al (1993) Fractures of the proximal humeral epiphysis. Int Orthop 17:16–19
Salter R, Harris W (1963) Injuries involving the epiphyseal plates. J Bone Joint Surg Am 45:587–622
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Den Hartog D, Van Lieshout EM, Tuinebreijer WE et al (2010) Primary hemiarthroplasty versus conservative treatment for comminuted fractures of the proximal humerus in the elderly (ProCon): a multicenter randomized controlled trial. BMC Musculoskelet Disord 11:97
Wang P, Koval KJ, Lehman W et al (1997) Salter-Harris type III fracture-dislocation of the proximal humerus. J Pediatr Orthop B 6(3):219–222
Beringer DC, Weiner DS, Noble JS et al (1998) Severely displaced proximal humeral epiphyseal fractures: a follow-up study. J Pediatr Orthop 18:31–37
Schwendenwein E, Hajdu S et al (2004) Displaced fractures of the proximal humerus in children require open/closed reduction and internal fixation. Eur J Pediatr Surg 14(1):51–55
Beaty JH (1992) Fractures of the proximal humerus and shaft in children. Instr Course Lect 41:369–372
Acknowledgements
The authors would like to thank the members of the hospital for helpful discussion of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S.-W. Wei, Z.-Y. Shi, Y.-M. Zhao, H. Wu, J.-Z. Hu, Z.-Z. Huang and J.-M. Zhao declare that they have no competing interests.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study or their legal guardians.
Additional information
Sheng-Wang Wie and Zhan-Ying Shi contributed equally to the manuscript
Rights and permissions
About this article
Cite this article
Wei, SW., Shi, ZY., Zhao, YM. et al. Comparison of conservative treatment outcomes for proximal humeral epiphyseal fractures in patients of different ages. Orthopäde 48, 119–124 (2019). https://doi.org/10.1007/s00132-018-03677-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00132-018-03677-3