Abstract
Purpose
Disorganised attachment is a key concept in understanding the development of psychosis. However, existing questionnaires of adult attachment do not adequately measure this construct hindering future research into the psychosocial causes of psychosis. The most widely measure of adult attachment in people experiencing psychosis is the Psychosis Attachment Measure (PAM). The measure has recently been revised to include disorganised attachment items. This study develops previous research by providing a rigorous examination the psychometric properties of the revised questionnaire (PAM-R).
Methods
A total of 407 participants with self-reported experiences of psychosis completed a battery of questionnaires which included the PAM-R and other measures which were conceptually related to the concept of disorganised attachment.
Results
Confirmatory factor analysis (CFA) indicated a three-factor solution with factors corresponding to anxious, avoidant, and disorganised attachment. The majority of the fit statistics were acceptable with the exception of the RMSEA statistic. Internal consistency and test–retest reliability were good for all subscales. The disorganised subscale correlated in expected directions with other measures of attachment, dissociation, trauma, and psychotic experiences.
Conclusion
The PAM-R is a valid and reliable measure of adult attachment. It is a practical assessment tool for clinicians and researchers to measure insecure and disorganised attachment patterns that is acceptable to people experiencing psychosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Psychosis is a serious mental health issue affecting 20 million people across the globe, and is associated with experiences such as hallucinations, delusions, and paranoia [1]. The proposed biological mechanisms underpinning psychosis have historically dominated research efforts. However, there has been a growing body of evidence demonstrating the link between childhood trauma and the nature and severity of psychotic symptoms [2,3,4], as well as the prevalence of interpersonal difficulties amongst this group [5]. This has highlighted that further exploration of psychosocial processes is a necessary, and promising, line of enquiry to better understand the onset and maintenance of psychosis [6].
Attachment theory has been identified as one psychological model which may help to delineate the relational component of this condition [7]. Attachment theory argues that our early relationships lead us to form “internal working models” from infancy, which include dynamic representations of the self, others, and the self within relationships [8]. This allows individuals to make sense of and interpret interpersonal interactions, informing their own behaviour within relationships and ultimately leading to the development of their attachment style [9]. Infants tend to form a “secure” attachment style when caregivers are emotionally attuned and available [10]. Caregivers provide a source of comfort and safety, which enables them to explore and appropriately manage distressing situations [11]. Where there are protracted difficulties in key relationships, particularly with respects to the caregiver’s sensitivity to infant distress [12], children a more likely to be insecurely attached, and develop an anxious, avoidant, or disorganised attachment pattern [13, 14].
Attachment styles appear to remain moderately stable from childhood to adulthood [15, 16], however can be subject to change, especially following significant adverse life events [17, 18], or exposure to positive alternative support figures [19]. In adulthood, whilst secure attachment has been associated with improved emotional regulation, social competence, and self-esteem [20, 21], insecure attachment styles have been linked with poorer mental health outcomes, relationship satisfaction, and resilience in coping with stressors [22,23,24].
Childhood trauma (including sexual, physical, and emotional abuse, parental death, neglect, and bullying) inherently threatens the formation of secure bonds. Given the link between trauma and psychosis, it is perhaps unsurprising that the prevalence of insecure attachment styles has been found to be significantly higher amongst this population compared to non-clinical samples [25, 26]. As such, it has been argued that attachment insecurity may act as a mediating factor in the relationship between childhood trauma and the onset of psychosis [7]. Indeed, there is a growing body of evidence in support of this hypothesis, illustrating the mediating role of attachment with respect to a wide range of psychotic phenomena, including paranoia [27] and voice-hearing [28]. There is a related body of research investigating factors which mediate the association between attachment and psychosis including negative beliefs, poor emotional regulation, poor cognitive diffusion [29], resilience [30], and experiential avoidance [31].
More recently, the concept of disorganised attachment has attracted substantial interest within psychosis research. This attachment pattern was first documented by Main and Solomon [14], who identified a subgroup of infants that appeared disoriented or demonstrated contradictory behaviour upon being reunited with their caregiver. It has been hypothesised that this develops when infants repeatedly experience the paradoxical situation whereby their caregiver is both the person that they turn to in times of distress, and the source of their fear [32]. The infant’s “fright without solution” then manifests in simultaneous or sequential attempts to approach and flee the caregiver, freezing, or dissociation [33]. In adulthood, the fear of both intimacy and abandonment underpins similar conflictual patterns of behaviour, accompanied by feelings of confusion and mistrust towards others [34]. This attachment pattern appears to predispose individuals to dissociative experiences [35], which is proposed to be a central process that contributes to development of voice-hearing [36]. Crucially, disorganised attachment has been associated with higher incidents of sexual and physical abuse in people living with psychosis, and more severe hallucinations and delusions, compared to other attachment styles [37]. These findings further highlight the potential for attachment theory to enrich current conceptualisations of psychosis and trauma, and identify areas for intervention. In turn, this requires valid and reliable measures of attachment that can be readily administered in both research and clinical settings.
Despite the abundance of self-report measures of attachment, a recent review conducted by Pollard et al. [38] suggests that many lack a robust evidence base or do not adequately capture the concept of disorganised attachment. For example, several self-report measures include a measure of fearful attachment, which is characterised by individuals vacillating between approach and avoidance behaviours in relationships and is thought to conceptually similar to but not equivalent to disorganised attachment as described in infancy. Similarly, many measures (i.e., Adult Disorganised Attachment Scale [ADA] [34]; The Psychological Treatment Inventory—Attachment Styles Scale [PTI-ASS] [39]) are designed with romantic relationships in mind. These items may not be as accessible for individuals with psychosis, who can often struggle to form and maintain close relationships [40]. The Psychosis Attachment Measure (PAM) is the most widely used adult attachment measure with people experiencing psychosis and assess avoidance and anxious attachment. Pollard et al. [41] recently adapted the measure to include items to capture disorganised attachment. The authors subjected 28 items which included 16 items in the original scale and 12 disorganised items to an EFA. They provided encouraging preliminary evidence regarding the psychometric properties of the PAM-R, although the authors’ results suggested removal of five items (including two of the original avoidance items) resulting in a 23-item measure. The present study aimed to build on the work of Pollard et al. to confirm the structural dimensionality, reliability, and validity of the PAM-R in an independent sample. Confirmatory factor analysis is an important step in measure development which aims to assess the stability of factor structures in new samples.
The following study hypotheses were developed in line with the Consensus-based Standards for the selection of health Measurement Instruments’ (COSMIN) criteria for good measurement properties [42].
-
1.
Confirmatory Factor Analysis will indicate a three-factor model of the PAM-R, according to multiple fit indices.
-
2.
Cronbach’s alphas used to determine internal consistency will be > 0.7 for all subscales.
-
3.
Test–retest reliability, as measured by Intraclass Correlation Coefficients (ICCs), will exceed 0.75 for all subscales.
-
4.
There will be a moderate positive association (correlation coefficients > 0.3) between the disorganised subscale and other measures which are conceptually related to this attachment style, including measures of trauma, dissociation, and psychotic experiences.
-
5.
A large positive relationship (> 0.5) will be observed between the disorganised factor of the PAM-R and the corresponding subscale of other measures of attachment.
Method
Participants
Participants were eligible to take part in the study providing that they (i) were aged 18 or over, (ii) had a self-reported diagnosis of a psychotic disorder or had received treatment for experiences related to psychosis, and (iii) were proficient in English. Participants were recruited online between January 2021 and December 2021, and completed all measures online. These data were combined with an existing data set collected as part of two previously published doctoral projects [43, 44]. The eligibility criteria, measures, and procedures, for this existing dataset, can be assumed to be the same unless otherwise stated in this paper.
Measures
Demographic questionnaire
This collected information about the participant’s gender, age, ethnicity, sexual orientation, relationship status, academic qualifications, and employment status. Questions around participants’ psychiatric diagnoses and experiences of mental health support relating to symptoms associated with psychosis were also included.
The Brief Betrayal Trauma Survey (BBTS)
The BBTS [45] is a 12-item self-report measure designed to assess exposure to trauma in childhood and adulthood. Participants were asked to rate their experience of adverse life events on a 3-point Likert scale (1—“never”; 2—“one or two times”; 3—“more than that”), before and after the age of 18. Freyd et al. [46] outline that items can also be grouped according to the level of betrayal: “high” (physical, emotional, or sexual abuse by someone close), “medium” (witnessing a traumatic event involving someone close or experiencing abuse perpetrated by someone more relationally distant), or “low” (witnessing a traumatic event involving someone less close, natural disasters, or accidents). Studies have indicated that the BBTS has good test–retest reliability [45] and construct validity [47]. Internal consistency within the present sample was α = 0.935 (before 18) and α = 0.835 (after age 18).
The Community Assessment Psychic Experiences—42 (CAPE)
The CAPE [48] is a 42-item self-report measure assessing positive and negative psychotic symptoms and depressive symptoms. Only the positive symptom subscale (20 items) was included within this study. Participants indicated what percentage of the time they experience the symptoms described in each question (0%—Never; 100%—Always). Good psychometric properties have been established for the CAPE, within both clinical and non-clinical samples [48, 49]. Internal consistency in this study was α = 0.795.
Dissociative Experiences Scale (DES-II)
DES-II [50] is a 28-item self-report measure assessing experiences of amnesia, depersonalisation, derealisation, and absorption. Participants were required to rate the extent to which they felt the item applied to their experiences, from 0 to 100% (0%—Never; 100%—Always). The DES-II is the most widely used measure of dissociative experiences, with numerous studies indicating good reliability and validity in both clinical and non-clinical samples [51]. Internal consistency in this sample was excellent (α = 0.944).
The Psychological Treatment Inventory-Attachment Styles Scale (PTI-ASS)
The PTI-ASS [39] is a 22-item self-report measure of all four adult attachment styles. The “unresolved” subscale provides a measure of disorganised attachment but like most measures of adult attachment the measure focussed on perceptions of oneself in the context of romantic relationships. Participants were required to indicate their level of agreement with each item, using a five-point Likert scale (1—“not at all”; 2—“somewhat”; 3—“moderately”; 4—“a good deal”; “very much”). Psychometric evaluation of the PTI-ASS provided evidence for its structural validity and internal consistency [36]. Internal consistency in the present sample was α = 0.73. The PTI-ASS was the only measure that was not administered in either Degnan et al. [44] nor Humphrey et al.’s [44] studies.
The Relationship Questionnaire (RQ)
The RQ [52] is a self-report measure designed to measure the four adult attachment styles. It consists of four paragraphs and respondents are required to rate to what extent they reflect their general relationship style, using a seven point Likert Scale (1—Disagree strongly; 7—Agree strongly). The “fearful” subscale is often considered as a proxy measure of disorganised attachment, but this has been contested in the literature [38]. The RQ is a widely used self-report measure of attachment, and reasonable psychometric properties have been reported [53].
The Revised Psychosis Attachment Measure (PAM-R)
The PAM-R [41] is 23-item self-report measure of anxious, avoidant, and disorganised attachment in psychosis. Participants were asked to rate to what extent each statement reflected how they relate to key people in their life, using a four-point Likert scale (“not at all”; “A little”; “quite a bit”; “very much”). Pollard et al. [41] reported promising psychometric properties in their initial validation study, including excellent test–retest reliability and preliminary evidence for the measure’s three-factor structure.
Procedure
All procedures were then approved by The University of Manchester’s University Research Ethics Committee (Ref: 2020-10240-17162), which included permission to utilise the data from the previous studies. Advertisement materials were developed and were posted on social media platforms (Facebook, Twitter, Reddit, and Instagram). Participants were also recruited via mental health charities and peer support groups, who disseminated the study information via their social media accounts, website, or email lists where appropriate. The study link provided information about the study. Once participants provided their consent to participate, they were directed to the demographics form. The subsequent measures were presented in a random order to reduce order effects; however, the BBTS was placed in the middle to minimise participant distress. When the questionnaires were completed, participants were asked whether they could be contacted again in 2 weeks to complete the PAM-R. This step was not included in the previous studies [43, 44]. Participants were then presented with a debrief sheet, and were given the option to provide their email if they wanted to receive a summary of research findings and/or be entered into a prize draw. The participants who opted to complete the PAM-R 2 weeks later also completed this online, following the same format.
Data analysis
Descriptive statistics, and tests of reliability and construct validity were carried out using IBM SPSS Statistics Version 25 [54]. The quality and distribution of the combined data was assessed first, which indicated that missing data were very low and that most variables were not normally distributed (Table 2). Accordingly, missing data were pro-rated with the median. BBTS responses were analysed according to age group (before 18 and after 18) and level of betrayal (high, medium, and low) as both factors were considered to be pertinent to the development of attachment styles. For construct validity, Spearman’s rank-order correlations were carried out as the data were not normally distributed for most measures. Confirmatory factor analysis (CFA) was conducted using the structural equation modelling module of JASP (version 0.16.00) [55], which is based on the R-package lavaan [56]. Diagonally Weighted Least Squares with robust error calculations was chosen as the estimation method, as this approach has been shown to perform well with ordinal data [57]. Model fit was evaluated using the Comparative Fit Index (CFI), Root-Mean-Square Error of Approximation (RMSEA), the Tucker-Lewis Index (TLI), and the Goodness-of-Fit Index (GFI). Schermelleh-Engel et al. [58] noted that acceptable model fit is indicated by CFI ≥ 0.95, RMSEA ≤ 0.08, TLI ≥ 0.95, and GFI ≥ 0.90.
Results
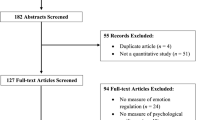
The new data collected were combined with the previous datasets; this was considered appropriate given the inclusion criteria and recruitment methods were the same, and to achieve the sample size required for factor analysis. The results reported are based on the combined dataset unless otherwise stated. A total of 466 participants completed the demographic questionnaire; however, 59 individuals did not go on to provide responses for any of the study measures and were therefore excluded from the analysis. The final sample size across therefore 407.
Sample characteristics
Demographic and clinical characteristics are presented in Table 1. The number of men and women was comparable; the majority identified as white and were aged between 18 and 34 years. Almost all participants reported that they had received a psychiatric diagnosis relating to psychosis, and most had a history of antipsychotic medication and/or mental health support (e.g., through a community mental health team).
Descriptive statistics for the study measures can be found in Table 2. Of the 360 participants who completed the BBTS “Before 18” scale, 81.1% reported having experienced at least one trauma and 70.3% reported a “high” betrayal trauma, whereby they were physically, psychologically, or sexually abused by someone that they considered themselves to be very close to. A total of 74.4% stated that they had experienced a traumatic event after the age of 18, with 63.9% endorsing items that were indicative of “high” betrayal. Mean scores for the DES-II exceeded 30, the threshold that is considered to denote “clinically significant” levels of dissociation [50].
Structural validity
Factor loadings of individual items are presented in Table 3, alongside Pollard et al.’s [38] EFA results. All items loaded onto the expected factors; all item loadings were > 0.4 [59]. The three-factor model based on Pollard et al.’s [38] research met the criteria for the CFI (0.955), TLI (0.950), and GFI (0.956). It was noted, however, that the three-factor model did not meet the RMSEA criteria (RMSEA = 0.107). Individual items were, therefore, re-evaluated according to the attachment literature, and modification indices, expected parameter change, and the standardised residual covariance matrix were examined for potential sources of misfit. Four items (9, 13, 15, and 22) were identified as potentially describing features of attachment which were not unique to the target attachment style and may be contributing to misspecification. As an experiment, these items were removed and CFA was conducted on the revised model—RMSEA was adequate (0.077), whilst the remaining three indices (CFI = 0.978; TLI = 0.975; GFI = 0.976) indicated a “good” model fit [58]. However, given that RMSEA can be influenced by sample size and all items loaded onto hypothesised factors above 0.4, all items were retained for subsequent analyses.
Reliability
Internal consistency
Cronbach’s alpha for the three subscales of the PAM-R was as follows: Avoidant = 0.804, Anxious = 0.845, and Disorganised = 0.887. Alphas if deleted statistics exceeded 0.770 suggesting that all individual items were relevant to their respective scales.
Test–retest reliability
Fifty-nine participants from this study provided responses to the PAM-R at Time 1 and Time 2. ICCs (absolute agreement, two-way mixed-effects model) with 95% Confidence Intervals: Avoidant = 0.863 (0.770–0.918), Anxious = 0.957 (0.927–0.974), and Disorganised = 0.910 (0.839–0.948).
Construct validity
Correlations and significance values are presented in Tables 4 and 5. The disorganised subscale had a large positive correlation with the fearful subscale of the RQ, and a moderate positive correlation with the unresolved scale of the PTI-ASS. Moderate positive correlations were also observed between the disorganised subscale and the frequency of positive symptoms, and the level of distress associated with these symptoms, as measured by the CAPE-42 Positive Symptoms subscale. Similarly, the PAM-R disorganised factor was moderately positively correlated with the DES-II, which captured dissociative experiences. Responses on the BBTS were grouped according to the level of betrayal (high, medium, and low) and whether the traumatic experience happened before or after 18 (Table 5). There was a small, but highly significant, positive correlation between the disorganised subscale and all BBTS groups except for the “low betrayal” group after aged 18. Traumatic experiences within each betrayal group had stronger associations with the disorganised subscale if they occurred before the age of 18. “High betrayal” items before aged 18 were most strongly associated with the disorganised subscale (r = 0.275)—the observed correlations were progressively weaker across the lower betrayal group. This pattern of correlations was also observed in the “after 18” groups. Compared to the other PAM-R subscales, the strongest correlations within each group were found for the disorganised scale.
Discussion
The CFA provided evidence for a three-factor model of the PAM-R (hypothesis 1), which included avoidant, anxious, and disorganised factors. Replication of Pollard et al.’s suggested factor structure resulted in an adequate-good fit across three out of the four fit indices. Further refinement of this model was achieved through removal of four items, which led to a “good” fit according to the CFI, TLI, and GFI, and “adequate” fit according to the RMSEA. Hypotheses 2 and 3 were also met—internal consistency and test–retest reliability exceeded the critical cut-offs for all three subscales using all the items. Notably, the disorganised subscale demonstrated “excellent” test–retest reliability across the 2-week timescale. This was in line with Pollard et al.’s. [38] findings; in their study, ICCs exceeded 0.823 and Cronbach’s alphas were greater than 0.791 across for all scales.
The disorganised subscale correlated in the expected directions with other related measures (hypotheses 4 and 5). However, a moderate correlation was found between the disorganised factor and the unresolved subscale of the PTI-ASS, whilst a large positive relationship was observed with the fearful subscale of the RQ. These findings suggest that the PAM-R may be more closely related to the fearful attachment captured by the RQ compared to disorganised attachment captured by the PTI-ASS. Nonetheless, the disorganised scale was not perfectly correlated with the RQ, perhaps because the RQ describes disorganised/fearful attachment in a single paragraph based on two dimensions: dependence and avoidance of intimacy [52]. Although these are core features of the disorganised PAM-R scale, the PAM-R also includes items relating to confusion, disorientation, and freezing—experiences which are characteristic of this attachment style according to both the child and adult literature [33, 34]. Similarly, the moderate correlation with the PTI-ASS may be explained by the fact that the PTI-ASS was designed with romantic, intimate relationships in mind [39], and may be less accessible to the target population given that these individuals are at greater risk of being socially isolated [5]. In addition, PTI-ASS’ unresolved items predominantly target aggression and mistreatment within relationships, as opposed to the emotional experience of the individual, which is a central focus of the PAM-R.
A moderate, highly significant, association was observed between the Disorganised PAM-R scale and measures of dissociative experiences and positive psychotic symptoms. This supports previous studies which have reported associations between these constructs and the disorganised attachment style [35, 36]. A small, positive relationship was established between with disorganised factor and the measure of trauma (BBTS); the magnitude of this correlation fell somewhat below expectations and Pollard et al.’s [41] findings (r > 0.3 for both age groups). This may in part be explained by the fact that the data for the BBTS were positively skewed, indicating that most participants had experienced one or more traumatic events “once or twice”. As this study did not collect information about potential protective factors, such as close relationships, supportive communities, and positive coping strategies [60], it is possible that impact of infrequent traumatic events was offset by significant positive and/or reparative experiences. However, it is noted that more significant abuse histories (as denoted by the “high” and “medium” betrayal groups of the BBTS) were more strongly associated with the disorganised factor, compared to the anxious or avoidant subscales. This is in line with previous research (e.g., [37]), which indicates that disorganised attachment is associated with higher proportions of interpersonal trauma.
Strengths and limitations
The COSMIN criteria for good measurement properties [42] informed the development of study hypotheses and the statistical methods employed. As such, the results were evaluated against globally recognised standards that indicate whether a measure is “good enough” to be used in research or clinical settings. With respects to the sample, men and women were both well represented, as were varied self-reported psychiatric diagnoses. Despite the research team being based in the UK, almost 60% of participants were not British, which highlights the potential for the PAM-R to be used beyond its country of origin. It was noted that over 53% of the sample identified as LGBTQ +. Arguably people may have felt more comfortable reporting their LGBTQ + status online compared to in face-to-face research, but the proportion of our sample within this group far exceeds general population estimates in the US and UK, which are less than 10% [61, 62]. As the LGBTQ + community is both underserved within research, and reportedly at heightened risk of developing mental health issues [63], there is value in the relative over-representation of this group in the present sample. However, the authors recognise that there may be some developmental and interpersonal experiences which are relatively unique to and/or ubiquitous within the LGBTQ + community which may impact upon attachment behaviour [64], thus limiting the generalisability of this study. It is possible that advert for our study was distributed disproportionately to groups representing people from LGBTQ + communities, but to the best of our knowledge, our recruitment strategy was not different from other online studies conducted by members of our research group.
A further limitation of this study was that the majority of the sample (> 83%) identified as white. Although this was broadly in line with data from the UK and US censuses [65, 66], the absolute number of participants from other ethnic groups, particularly the black community, was very low. As several studies have indicated that the weighted prevalence of psychosis is much higher amongst the black population (e.g., [67, 68]) compared to white communities in the UK, it would be important for this limitation to be addressed in future research to ensure that the PAM-R is accessible and appropriate for a range of ethnic groups. This study also relied on self-reported experiences of psychosis and approximately 7% of the sample did not report a diagnosis of psychiatric diagnosis. Whilst a substantial majority (> 65%) described previous inpatient experience and clinically significant levels of dissociation, the risk that these findings may not generalise to a clinical setting, where the original PAM was tested, is noted. In addition, the online methodology and merged data set created a risk of participants completing the questionnaires more than once. However, as the projects were advertised via independent social media accounts, led by different researchers, and had recruitment windows that were approximately 2 years apart, it is argued that their respective reach and networks would have likely been sufficiently different, so that risk of repeat responders was not significant. Finally, in terms of the psychometric properties assessed within this study, discriminant validity was one key area which was not explored.
Implications and future research
This study provided further validation of the PAM-R and evidence of its psychometric properties. The PAM-R demonstrated a theoretically relevant factor structure, and all subscales were found to internally consistent and stable over a two-week period. The new disorganised scale correlated in expected directions with other conceptually relevant measures, providing evidence for its concurrent and convergent validity. Together, these findings suggest that the PAM-R has good psychometric properties, giving researchers and clinicians alike access to a time- and cost-effective measure of attachment for individuals with experiences of psychosis. They also further contribute to the research base which indicates a relationship between disorganised attachment and positive psychotic symptoms, dissociation, and trauma. The authors tentatively suggest that the PAM-R may be further improved through the removal or adaptation of four items; however, this assertion would need to be confirmed within a future representative sample. Future research may usefully focus on validating the PAM-R in clinical settings. Kvrgic and colleagues [69] conducted a similar study with the German version of the original PAM; their findings could be extended through the inclusion of the disorganised subscale in an English-speaking population. The inclusion of a non-clinical population for comparison would also allow for the discriminant validity of the PAM-R to be examined. Separately, one of the key motivations for developing the PAM was the lack of valid attachment measures which did not focus on intimate or romantic relationships, as these were argued to be less accessible and less relevant for individuals with psychosis who are more at risk of experiencing interpersonal difficulties [5]. It is noted that individuals who are neurodivergent or experience other significant mental health issues (e.g., people diagnosed with personality or bipolar disorders) can have similar difficulties in in maintaining social connections, and thus, there is scope for future studies to investigate the application of the PAM-R in other potentially socially isolated groups.
Conclusions
This study suggests that the PAM-R is a reliable and valid measure of attachment in psychosis. The findings provide further evidence of its structural dimensionality, internal consistency, test–retest reliability, and convergent validity. A three-factor solution was demonstrated by CFA; however, the authors propose that four of the items which may have contributed to the poor RMSEA statistic require further investigation. Future research is needed to replicate these findings within a representative clinical population and to establish discriminant validity.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Global Burden of Disease Collaborators (2018) Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392:1789–1858. https://doi.org/10.1016/S0140-6736(18)32279-7
Bailey T, Alvarez-Jimenez M, Garcia-Sanchez AM, Hulbert C, Barlow E, Bendall S (2018) Childhood trauma is associated with severity of hallucinations and delusions in psychotic disorders: a systematic review and meta-analysis. Schizophr Bull 44:1111–1122. https://doi.org/10.1093/schbul/sbx161
Bentall RP, Wickham S, Shevlin M, Varese F (2012) Do specific early-life adversities lead to specific symptoms of psychosis? A study from the 2007 the Adult Psychiatric Morbidity Survey. Schizophr Bull 38:734–740. https://doi.org/10.1093/schbul/sbs049
Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, Bentall RP (2012) Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective-and cross-sectional cohort studies. Schizophr Bull 38:661–671. https://doi.org/10.1093/schbul/sbs050
Mueser KT, Deavers F, Penn DL, Cassisi JE (2013) Psychosocial treatments for schizophrenia. Annu Rev Clin Psychol 9:465–497. https://doi.org/10.1146/annurev-clinpsy-050212-185620
Read J, Bentall RP, Fosse R (2009) Time to abandon the bio-bio-bio model of psychosis: exploring the epigenetic and psychological mechanisms by which adverse life events lead to psychotic symptoms. Epidemiol Psychiatr Sci 18:299–310. https://doi.org/10.1017/S1121189X00000257
Berry K, Barrowclough C, Wearden A (2008) Attachment theory: a framework for understanding symptoms and interpersonal relationships in psychosis. Behav Res Ther 46:1275–1282. https://doi.org/10.1016/j.brat.2008.08.009
Bowlby J (1979) The Bowlby-Ainsworth attachment theory. Behav Brain Sci 2:637–638
Bretherton I, Ridgeway D, Cassidy J (1990) Assessing internal working models of the attachment relationship. In: Greenberg MT, Cicchetti D, Cummings EM (eds) Attachment in the preschool years: theory, research, and intervention. University of Chicago Press, Chicago, pp 273–308
Goldsmith DF (2010) The emotional dance of attachment. Clin Soc Work J 38:4–7. https://doi.org/10.1007/s10615-009-0220-6
Bowlby J (1988) A secure base: clinical applications of attachment theory. Routledge, London
McElwain NL, Booth-Laforce C (2006) Maternal sensitivity to infant distress and nondistress as predictors of infant-mother attachment security. J Family Psychol 20:247–255. https://doi.org/10.1037/0893-3200.20.2.247
Ainsworth MS (1979) Infant–mother attachment. Am Psychol 34:932–937. https://doi.org/10.1037/0003-066X.34.10.932
Main M, Solomon J (1986) Discovery of an insecure-disorganized/disoriented attachment pattern. In: Brazelton TB, Yogman MW (eds) Affective development in infancy. Ablex Publishing, New York, pp 95–124
Fraley R (2002) Attachment stability from infancy to adulthood: meta-analysis and dynamic modeling of developmental mechanisms. Pers Soc Psychol Rev 6:123–151. https://doi.org/10.1207/S15327957PSPR0602_03
Pinquart M, Feußner C, Ahnert L (2013) Meta-analytic evidence for stability in attachments from infancy to early adulthood. Attach Hum Dev 15:189–218. https://doi.org/10.1080/14616734.2013.746257
Waters E, Hamilton CE, Weinfield NS (2000) The stability of attachment security from infancy to adolescence and early adulthood: general introduction. Child Dev 71:678–683. https://doi.org/10.1111/1467-8624.00175
Waters E, Merrick S, Treboux D, Crowell J, Albersheim L (2000) Attachment security in infancy and early adulthood: a twenty-year longitudinal study. Child Dev 71:684–689. https://doi.org/10.1111/1467-8624.00176
Saunders R, Jacobvitz D, Zaccagnino M, Beverung LM, Hazen N (2011) Pathways to earned-security: the role of alternative support figures. Attach Hum Dev 13:403–420. https://doi.org/10.1080/14616734.2011.584405
Doinita NE (2015) Adult attachment, self-esteem and emotional intelligence. Proc Soc Behav Sci 187:570–574. https://doi.org/10.1016/j.sbspro.2015.03.106
Sroufe LA (2005) Attachment and development: a prospective, longitudinal study from birth to adulthood. Attach Hum Dev 7:349–367. https://doi.org/10.1080/14616730500365928
Bender A, Ingram R (2018) Connecting attachment style to resilience: contributions of self-care and self-efficacy. Pers Individ Differ 130:18–20. https://doi.org/10.1016/j.paid.2018.03.038
Gleeson G, Fitzgerald A (2014) Exploring the association between adult attachment styles in romantic relationships, perceptions of parents from childhood and relationship satisfaction. Health 6:1643–1661. https://doi.org/10.4236/health.2014.613196
Mikulincer M, Shaver PR (2012) An attachment perspective on psychopathology. World Psychiatry 11:11–15. https://doi.org/10.1016/j.wpsyc.2012.01.003
Carr SC, Hardy A, Fornells-Ambrojo M (2018) Relationship between attachment style and symptom severity across the psychosis spectrum: a meta-analysis. Clin Psychol Rev 59:145–158. https://doi.org/10.1016/j.cpr.2017.12.001
Herstell S, Betz LT, Penzel N, Chechelnizki R, Filihagh L, Antonucci L, Kambeitz J (2021) Insecure attachment as a transdiagnostic risk factor for major psychiatric conditions: a meta-analysis in bipolar disorder, depression and schizophrenia spectrum disorder. J Psychiatr Res 144:190–201. https://doi.org/10.1016/j.jpsychires.2021.10.002
Lavin R, Bucci S, Varese F, Berry K (2020) The relationship between insecure attachment and paranoia in psychosis: a systematic literature review. Br J Clin Psychol 59:39–65. https://doi.org/10.1111/bjc.12231
Pilton M, Bucci S, McManus J, Hayward M, Emsley R, Berry K (2016) Does insecure attachment mediate the relationship between trauma and voice-hearing in psychosis? Psychiatry Res 246:776–782. https://doi.org/10.1016/j.psychres.2016.10.050
Sood M, Carnelley KB, Newman-Taylor K (2022a) How does insecure attachment lead to paranoia? A systematic critical review of cognitive, affective, and behavioural mechanisms. Br J Clin Psychol bjc.12361:781–815. https://doi.org/10.1111/bjc.12361
Rossi R, Jannini TB, Ciocca G, Cipriani C, Socci V, Paitti F, Lorenzo GD (2023) Attachment and resilience as mediators or moderators in the relationships between trauma and psychotic-like experiences. Schizophr Res 258:36–44
Castilho P, Martins MJ, Pinto AM, Viegas R, Carvalho S, Madeira N (2017) Understanding the effect of attachment styles in paranoid ideation: the mediator role of experiential avoidance. J Context Behav Sci 6(1):42–46. https://doi.org/10.1016/j.jcbs.2016.11.00
Liotti G (2004) Trauma, dissociation and disorganized attachment: three strands of a single braid. Psychotherapy 41:472–486. https://doi.org/10.1037/0033-3204.41.4.472
Duschinsky R (2015) The emergence of the disorganized/disoriented (D) attachment classification, 1979–1982. Hist Psychol 18:32–46. https://doi.org/10.1037/a0038524
Paetzold RL, Rholes WS, Kohn JL (2015) Disorganized attachment in adulthood: theory, measurement, and implications for romantic relationships. Rev Gen Psychol 19:146–156. https://doi.org/10.1037/gpr0000042
Liotti G, Gumley A (2008) An attachment perspective on schizophrenia: the role of disorganized attachment, dissociation and mentalization. In: Moskowitz A, Schӓfer I, Dorahy MJ (eds) Psychosis, trauma and dissociation: emerging perspectives on severe psychopathology. Wiley, New Jersey, pp 117–133 https://doi.org/10.1002/9780470699652.ch9
Berry K, Bucci S (2016) What does attachment theory tell us about working with distressing voices? Psychosis 8:60–71. https://doi.org/10.1080/17522439.2015.1070370
Bucci S, Emsley R, Berry K (2017) Attachment in psychosis: a latent profile analysis of attachment styles and association with symptoms in a large psychosis cohort. Psychiatry Res 247:243–249. https://doi.org/10.1016/j.psychres.2016.11.036
Pollard C, Bucci S, Berry K (2023) A systematic review of measures of adult disorganized attachment. Br J Clin Psychol 1–24. https://doi.org/10.1111/bjc.12411
Giannini M, Gori A, De Sanctis E, Schuldberg D (2011) Attachment in psychotherapy: psychometric properties of the Psychological Treatment Inventory Attachment Styles Scale (PTI-ASS). J Psychother Integr 21:363–381. https://doi.org/10.1037/a0025461
de Jager J, Cirakoglu B, Nugter A, van Os J (2017) Intimacy and its barriers: a qualitative exploration of intimacy and related struggles among people diagnosed with psychosis. Psychosis 9:301–309. https://doi.org/10.1080/17522439.2017.1330895
Pollard C, Bucci S, MacBeth A, Berry K (2020) The revised psychosis attachment measure: measuring disorganized attachment. Br J Clin Psychol 59:335–353. https://doi.org/10.1111/bjc.12249
Prinsen CAC, Mokkink LB, Bouter LM, Alonso J, Patrick DL, De Vet HCW, Terwee CB (2018) COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res 27:1147–1157. https://doi.org/10.1007/s11136-018-1798-3
Degnan A, Berry K, Humphrey C, Bucci S (2022) The role of attachment and dissociation in the relationship between childhood interpersonal trauma and negative symptoms in psychosis. Clin Psychol Psychother 29:1692–1706. https://doi.org/10.1002/cpp.2731
Humphrey C, Berry K, Degnan A, Bucci S (2022) Childhood interpersonal trauma and paranoia in psychosis: the role of disorganised attachment and negative schema. Schizophr Res 241:142–148. https://doi.org/10.1016/j.schres.2022.01.043
Goldberg LR, Freyd JJ (2006) Self-reports of potentially traumatic experiences in an adult community sample: gender differences and test-retest stabilities of the items in a brief betrayal-trauma survey. J Trauma Dissociation 7:39–63. https://doi.org/10.1300/J229v07n03_04
Freyd JJ, Klest B, Allard CB (2005) Betrayal trauma: relationship to physical health, psychological distress, and a written disclosure intervention. J Trauma Dissoc 6:83–104. https://doi.org/10.1300/J229v06n03_04
Martin CG, Cromer LD, DePrince AP, Freyd JJ (2013) The role of cumulative trauma, betrayal, and appraisals in understanding trauma symptomatology. Psychol Trauma 5:110–118. https://doi.org/10.1037/a0025686
Stefanis NC, Hanssen M, Smirnis NK, Avramopoulos DA, Evdokimidis IK, Stefanis CN, Verdoux H, van Os J (2002) Evidence that three dimensions of psychosis have a distribution in the general population. Psychol Med 32:347–358. https://doi.org/10.1017/S0033291701005141
Yung AR, Nelson B, Baker K, Buckby JA, Baksheev G, Cosgrave EM (2009) Psychotic-like experiences in a community sample of adolescents: implications for the continuum model of psychosis and prediction of schizophrenia. Aust N Z J Psychiatry 43:118–128. https://doi.org/10.1080/00048670802607188
Carlson EB, Putnam FW (1993) An update on the dissociative experiences scale. Dissociation 6:16–27
Patihis L, Lynn SJ (2017) Psychometric comparison of Dissociative Experiences Scales II and C: a weak trauma-dissociation link. Appl Cogn Psychol 31:392–403. https://doi.org/10.1002/acp.3337
Bartholomew K, Horowitz LM (1991) Attachment styles among young adults: a test of a four-category model. J Pers Soc Psychol 61:226–244. https://doi.org/10.1037/0022-3514.61.2.226
Griffin DW, Bartholomew K (1994) The metaphysics of measurement: the case of adult attachment. In: Bartholomew K, Perlman D (eds) Attachment processes in adulthood. Jessica Kingsley Publishers, London, pp 17–52
Corp IBM (2017) IBM SPSS Statistics for Windows, Version 25. IBM Corp, New York
JASP Team (2021) JASP (Version 0.16) [Computer software]
Rosseel Y (2012) lavaan: an R package for structural equation modeling. J Stat Softw 48:1–36. https://www.jstatsoft.org/v48/i02/
Li CH (2016) The performance of ML, DWLS, and ULS estimation with robust corrections in structural equation models with ordinal variables. Psychol Methods 21:369–387. https://doi.org/10.1037/met0000093
Schermelleh-Engel K, Moosbrugger H, Müller H (2003) Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Methods Psychol Res Online 8:23–74
Matsunaga M (2010) How to factor-analyze your data right: do’s, don’ts, and how-to’s. Int J Psychol Res 3:97–110. https://doi.org/10.21500/20112084.854
Banyard VL, Williams LM, Siegel JA (2003) The impact of complex trauma and depression on parenting: an exploration of mediating risk and protective factors. Child Maltreat 8:334–349. https://doi.org/10.1177/1077559503257106
Newport F (2018) In U.S., estimate of LGBT population rises to 4.5%. https://news.gallup.com/poll/234863/estimate-lgbt-population-rises.aspx. Accessed 8 Mar 2023
Sharfman A, Cobb P (2021) Sexual orientation, UK: 2019. https://www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/sexuality/bulletins/sexualidentityuk/2019. Accessed 8 Mar 2023
Kidd SA, Howison M, Pilling MD, Ross LE, McKenzie K (2016) Severe mental illness in LGBT populations: a scoping review. Psychiatr Serv 67:779–783. https://doi.org/10.1176/appi.ps.201500209
Tharinger D, Wells G (2000) An attachment perspective on the developmental challenges of gay and lesbian adolescents: the need for continuity of caregiving from family and schools. School Psychol Rev 29:158–172. https://doi.org/10.1080/02796015.2000.12086004
White E (2012) Ethnicity and National Identity in England and Wales: 2011. https://www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/ethnicity/articles/ethnicityandnationalidentityinenglandandwales/2012-12-11. Accessed 8 Mar. 2023
Jones N, Marks R, Ramirez R, Ríos-Vargas M (2021) Improved race and ethnicity measures reveal U.S. population is much more multiracial. https://www.census.gov/library/stories/2021/08/improved-race-ethnicity-measures-reveal-united-states-population-much-more-multiracial.html Accessed 8 Mar 2023
Morgan C, Dazzan P, Morgan K, Jones P, Harrison G, Leff J, Fearon P (2006) First episode psychosis and ethnicity: initial findings from the AESOP study. World Psychiatry 5:40–46
Qassem T, Bebbington P, Spiers N, McManus S, Jenkins R, Dein S (2015) Prevalence of psychosis in black ethnic minorities in Britain: analysis based on three national surveys. Soc Psychiatry Psychiatr Epidemiol 50:1057–1064. https://doi.org/10.1007/s00127-014-0960-7
Kvrgic S, Beck EM, Cavelti M, Kossowsky J, Stieglitz RD, Vauth R (2012) Focusing on the adult attachment style in schizophrenia in community mental health centres: validation of the Psychosis Attachment Measure (PAM) in a German-speaking sample. Int J Soc Psychiatry 58:362–373. https://doi.org/10.1177/0020764011399004
Funding
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MJN contributed to the research proposal, collected the data, carried out the analysis and wrote the first draft of the paper. KB developed the idea for the study, supervised and edited drafts of the paper. LM supervised the work and edited drafts of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Patient consent statement
The authors confirm that patient’s consent was obtained for their participation in their study and for the publication of findings, including anonymised data. The study design was approved by The University of Manchester’s University Research Ethics Committee (Ref: 2020-10240-17162).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Justo-Nunez, M., Morris, L. & Berry, K. The revised Psychosis Attachment Measure: further psychometric evidence. Soc Psychiatry Psychiatr Epidemiol (2024). https://doi.org/10.1007/s00127-024-02624-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00127-024-02624-2