Abstract
Aim/hypothesis
Our aim was to investigate the association between the macrophage-activation marker soluble CD163 (sCD163), adiponectin, C-reactive protein (CRP) and changes in glycaemia, insulin resistance and insulin secretion in individuals at high risk of type 2 diabetes mellitus.
Methods
This prospective study included 1014 individuals at high risk of type 2 diabetes mellitus participating in the Danish arm of the Anglo-Danish-Dutch study of Intensive Treatment In PeOple with ScreeN-detected Diabetes in Primary Care (ADDITION-Europe trial) baseline examination in 2001–2006 and follow-up examination (ADDITION-Progression [ADDITION-PRO]) in 2009–2011. Baseline serum samples were analysed for sCD163, adiponectin and CRP. The associations between sCD163, adiponectin and CRP per doubling of concentration, and changes per year in HbA1c, fasting plasma glucose, 2 h glucose, fasting insulin, HOMA-IR and HOMA-β were assessed using a mixed-effects model.
Results
A doubling of sCD163 concentration was positively associated with changes in HOMA-β (β = 1.160 per year, 95% CI 0.345, 1.975) as well as a doubling of CRP concentration (β = 0.410 per year, 95% CI 0.051, 0.769) after adjustment for age and sex. A doubling of adiponectin was inversely associated with changes in 2 h glucose (β =−0.063 per year, 95% CI −0.111, −0.014), HOMA-IR (β =−0.038 per year, 95% CI −0.060, −0.015) and HOMA-β (β =−1.028 per year, 95% CI −1.635, −0.421) after adjustment for age and sex. The associations were robust to adjustment for baseline waist circumference and smoking. Adjustment for CRP did not change the associations for sCD163 or adiponectin.
Conclusions/interpretation
Our findings indicate that mechanisms related to inflammation, including macrophage activation and adipocyte metabolism, may play a role in changes in glucose homeostasis in individuals at high risk of type 2 diabetes mellitus.
Similar content being viewed by others
Introduction
Low-grade inflammation has been proposed to be one of the pathophysiological links between obesity and type 2 diabetes mellitus [1, 2]. This link is potentially clinically important, as inflammatory pathways may be a target for intervention.
Low-grade inflammation in type 2 diabetes mellitus is characterised by increased levels of cytokines such as TNF-α, IL-1β and IL-6, and of acute-phase proteins such as the widely used unspecific marker of systemic inflammation C-reactive protein (CRP) [2]. Adipose tissue is an important contributor to this inflammatory process in obesity. During the development of obesity and the progression of dysglycaemia, the immune cell population changes in number and phenotype—particularly in visceral adipose tissue—with the macrophage as the key immune cell and the principal source of inflammatory mediators [3]. Most previous research on low-grade inflammation in type 2 diabetes mellitus has been carried out on inflammatory markers secreted by more than one inflammatory cell, whereas little is known about inflammatory markers secreted solely by the macrophage.
Soluble CD163 (sCD163) is a specific monocyte/macrophage-derived biomarker that reflects macrophage activation during inflammation [4–6]. High circulating levels of sCD163 are associated with obesity, insulin resistance and type 2 diabetes mellitus in cross-sectional studies [7–9]. sCD163 is furthermore associated with incident type 2 diabetes mellitus in a prospective study [10]. Circulating sCD163 may therefore represent a possible risk indicator for the future development of type 2 diabetes. However, its specific association with more detailed and continuous hallmarks of progression of dysglycaemia remains unclear.
Adiponectin is an adipocyte-derived hormone and the most abundant hormone secreted by adipocytes. Animal studies show that adiponectin suppresses hepatic gluconeogenesis, enhances whole-body insulin sensitivity and reduces inflammation, including promotion of macrophages into the anti-inflammatory state [11, 12]. From human cross-sectional and longitudinal studies, it is well known that adiponectin levels are inversely related to obesity, insulin resistance and type 2 diabetes mellitus [13], but prospective studies on the effect of adiponectin on the progression of dysglycaemia are sparse.
We hypothesised that markers of inflammation including macrophage activation and adipocyte metabolism might be associated with early metabolic changes in glycaemia, insulin resistance and insulin secretion in individuals at high risk of type 2 diabetes mellitus. Thus, the primary aim of the present study was to investigate the association between sCD163, adiponectin and CRP and changes in HbA1c, fasting glucose, 2 h glucose, fasting insulin, insulin resistance and insulin secretion in the ADDITION-Progression (ADDITION-PRO) cohort.
Methods
Study design, setting and participants
The present study is a prospective cohort study of individuals at high risk of type 2 diabetes mellitus identified in 2001–2006 at baseline in a step-wise screening programme in the Danish arm of the Anglo-Danish-Dutch study of Intensive Treatment In PeOple with ScreeN-detected Diabetes in Primary Care (ADDITION-Europe trial) [14]. The first step was a self-administered risk score questionnaire including questions on diabetes risk factors. If a high risk of diabetes was found, individuals were recommended to contact their general practitioner, and a step-wise process of screening using random glucose and HbA1c measurements, followed by fasting glucose and if necessary an OGTT as diagnostic tests, was undertaken.
Individuals eligible for invitation were 40–69 years old at baseline, had not previously been diagnosed with diabetes and were registered at participating practices. Exclusion criteria were pregnancy, lactation, being housebound, life expectancy less than 1 year or an inability to give informed consent due to a psychological or psychiatric issue. ADDITION-PRO was the follow-up health examination of individuals at different incremental levels of diabetes risk defined by the screening procedure but without diabetes at baseline [15]. ADDITION-PRO was performed between 2009 and 2011 at four research centres in Denmark, and blood tests were performed on all participants. All participants provided written informed consent. The methods of the ADDITION-Europe trial and ADDITION-PRO have previously been published [14, 15].
Assessment of sCD163, adiponectin and CRP
Measurements were performed during 2014–2015 at the Department of Clinical Biochemistry, Aarhus University Hospital, Aarhus, Denmark. Due to limited available serum volumes, analyses were carried out in an order of priority—(1) sCD163, (2) adiponectin, and (3) CRP—leading to slight differences in the number of available data points for each of the biomarkers.
The concentration of sCD163 was measured by in-house sandwich ELISA using a BEP 2000 ELISA-analyser (Dade Behring, Deerfield, IL, USA) essentially as previously described [6]. The limit of detection was 6.25 μg/l. External control serum samples were analysed in each run (n = 48) with a total CV of 8.3% (n = 91) at a level of 1.77 mg/l. Serum adiponectin was measured by sandwich immunoassay with electrochemiluminescence detection (Meso Scale Discovery [MSD], Metabolic Assays, Human Adiponectin Kit, Gaithersburg, MD, USA) according to the manufacturer’s instructions. The limit of detection was 0.005 ng/ml. External control serum samples were analysed in each run (n = 17), with a total CV of 14.1% (n = 34) at a level of 11.5 μg/ml. A detailed description for the assessment of sCD163 and adiponectin can be found in the section on assessment of sCD163 and adiponectin in the electronic supplementary material (ESM) Methods. Analysis of CRP was performed by particle-enhanced immunoturbidimetry on a Cobas 6000 automated biochemical analyser (Roche Diagnostics, Indianapolis, IN, USA). The limit of detection was 5.7 nmol/l, and values below the limit of detection were considered to be 5.7 nmol/l.
Assessment of glucose variables, insulin and cholesterol
HbA1c was analysed using ion-exchange HPLC on Tosoh machines at baseline (TOSOH A1c 2.2, Stuttgart, Germany) and follow-up (TOSOH G7, Tokyo, Japan). At baseline, fasting capillary glucose was measured at the same time as biobank materials were being collected. Readings for 2 h capillary glucose concentration were obtained after a standard 75 g OGTT. The capillary whole blood samples were analysed using a glucose dehydrogenase reaction (HemoCue Glucose Analyzer, Ängelholm, Sweden). The average of two capillary blood samples was used and multiplied by 1.11 to calculate the plasma equivalent values [16]. At follow-up, fasting plasma glucose (FPG) and 2 h plasma glucose (2hPG) concentrations were measured in plasma from venous blood samples using the Hitachi 912 system (Roche Diagnostics, Mannheim, Germany) during 2009–2010 and the VITROS 5600 Integrated System (Ortho Clinical Diagnostics, Illkirch Cedex, France) during 2010–2011. Validation analyses between the two systems were carried out, and conversion factors were applied to values measured using the VITROS equipment [15].
Baseline fasting insulin was measured in biobank samples by sandwich immunoassay with electrochemiluminescence detection (MSD) according to the manufacturer’s instructions. The assay was calibrated using human recombinant insulin anchored to international standards. The limit of detection was 1.29 pmol/l. External control serum samples were analysed in each run (n = 18), with a total CV of 16.7% (n = 36) at a level of 98.5 pmol/l. Follow-up fasting insulin concentrations were measured immediately by immunoassay (AutoDELFIA, Perkin Elmer [PE], Waltham, MA, USA). To address potential sources of bias in the insulin assay, 80 follow-up biobank samples were measured employing the MSD assay. Using linear regression analysis, the following equation was used to transform insulin values as measured by the MSD process into insulin measured by PE: PE = 4.2716 + MSD × 0.8020. Insulin resistance was estimated from FPG and fasting insulin using HOMA-IR: [fasting insulin (pmol/l) × fasting glucose (mmol/l)]/135 [17]. Insulin secretion was assessed using HOMA-β: [fasting insulin (pmol/l) × 3.33]/[FPG (mmol/l) − 3.5] [17]. Extreme values of FPG (≤3 or ≥25 mmol/l) and fasting insulin (≤20 or ≥400 pmol/l) were replaced by missing values in the HOMA analysis as they exceeded the range for HOMA calculation [17, 18]. Total cholesterol was measured as previously described [14, 15].
Assessment of anthropometry factors and smoking
BMI was calculated as weight in kilograms divided by the square of the height in metres. Waist circumference (WC) was measured with the participant in a standing position. Systolic BP (SBP) and diastolic BP (DBP) were measured as the mean of two recordings with the participant seated after a 10 min rest. Information on smoking habits was collected from baseline questionnaires, and in this analysis reclassified as yes or no to being a current smoker.
Registry data
Information on sex and date of birth was obtained from the Danish Civil Registry. Known type 2 diabetes mellitus during follow-up was reported by general practitioners based on medical records in addition to self-report at the follow-up examination.
Statistical analysis
Characteristics of study participants were analysed by frequencies and percentages, medians and interquartile interval (25th and 75th percentiles) as appropriate. sCD163, adiponectin and CRP were used as independent variables in separate models for each biomarker. The outcome measures were HbA1c, FPG, 2hPG, fasting insulin, HOMA-IR and HOMA-β.
In order to assess the effect of determinants per doubling of concentration with an intercept at the mean, we centred sCD163, adiponectin and CRP by subtracting their respective mean and calculated the base 2 logarithm (log2). We estimated the time-dependent and time-independent association between the biomarkers and our outcomes using a mixed-effects model. Estimates are given as β coefficients, 95% CI and corresponding p values. Assumptions for the mixed-effects model were tested, and residuals and random intercepts were close to being normally distributed. Further details of the mixed-effects model can be found in the section on the mixed-effects model in ESM Methods.
Based on the direct acyclic graph model, we considered age, sex, baseline WC, smoking and CRP as potential confounders (ESM Fig. 1). Model 0 was the basic analysis. Adjustment for age and sex was carried out in model 1. Model 2 further included baseline WC. Model 2b was additionally adjusted for smoking status at baseline in the analysis of CRP. To account for the general systemic inflammation, model 3 additionally included adjustment for CRP in the analysis of sCD163 and adiponectin. In the mixed-effects model, we excluded individuals with missing data on biomarkers, outcomes and confounders. In addition, two individuals were excluded from the analyses on CRP and 2hPG due to incompatible running of the mixed-effects model in the STATA software. In order to investigate the presence of effect modification by sex, we included sex as an interaction term for both the time-dependent and time-independent associations. Statistical analysis was carried out using STATA version 13 (StataCorp, College Station, TX, USA). Two-sided p values ≤0.05 were considered statistically significant.
Ethics
The study was approved by the local scientific ethics committee (approval no. 1-10-72-137-13) and was conducted according to the principles of the 1996 Helsinki Declaration.
Results
Study population
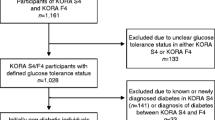
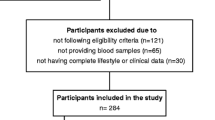
A total of 2082 (50%) out of 4188 invited individuals attended, whereas 2106 did not attend the ADDITION-PRO follow-up examination (Fig. 1). We excluded 336 individuals who had developed type 2 diabetes mellitus during follow-up. These individuals had higher levels of sCD163 (1.8 vs 1.6 mg/l, p < 0.001) and CRP (25.7 vs 16.2 nmol/l, p < 0.001) and lower levels of adiponectin (11.5 vs 14.4 μg/ml, p < 0.001) at baseline compared with individuals who did not develop type 2 diabetes during follow-up. We further excluded 667 individuals who did not have baseline biobank materials. Descriptive characteristics of the individuals with and without biobank materials are shown in ESM Table 1. We additionally excluded 65 individuals with CRP concentrations above 95 nmol/l, taken as evidence of acute infection.
Thus, 1014 individuals were eligible for the present study. Descriptive characteristics of the study population including median levels of the biomarkers are shown in Table 1. Higher levels of adiponectin (17.9 vs 12.1 μg/ml, p < 0.001) and CRP (19.0 vs 12.4 nmol/l, p < 0.001) were found in women than men. No sex differences were found in the level of sCD163. The mean duration of follow-up was 7.5 (SD = 1.4) years.
Changes in glycaemia, insulin resistance and insulin secretion during follow-up
HbA1c, FPG and 2hPG concentrations increased during follow-up after age and sex adjustment: 0.723% (95% CI 0.714, 0.732; 4.971 mmol/mol, 95% CI 4.898, 5.044) per year for HbA1c, 0.762 mmol/l (95% CI 0.752, 0.772) per year for FPG and 0.950 mmol/l (95% CI 0.917, 0.983) per year for 2hPG. The estimates for yearly rates of increase were further strengthened after accounting for baseline levels of each respective variable (ESM Table 2). Fasting insulin, HOMA-IR and HOMA-β values also increased during follow-up after adjustment for age and sex: 5.862 pmol/l (95% CI 5.526, 6.199) per year for fasting insulin, 0.290 (95% CI 0.275, 0.306) per year for HOMA-IR and 8.190 (95% CI 7.771, 8.609) per year for HOMA-β. However, the velocities of increase were attenuated by including baseline insulin levels (ESM Table 2). Further adjustment for baseline WC and smoking did not materially change the estimates, and estimates remained statistically significant.
Baseline sCD163, adiponectin, CRP and changes in glycaemia, insulin resistance and insulin secretion
Baseline sCD163 and CRP were positively associated with changes in HOMA-β, and in addition sCD163 was positively associated with fasting insulin after adjustment for age and sex. Baseline adiponectin was negatively associated with changes in 2hPG, fasting insulin, HOMA-IR and HOMA-β after age and sex adjustment (Tables 2, 3, and 4). In contrast to adiponectin, sCD163 and CRP were not significantly associated with changes in 2hPG or HOMA-IR. Baseline sCD163, adiponectin and CRP were not associated with any statistically significant changes in either HbA1c or FPG. The associations remained stable after further adjustment for baseline WC. In addition, adjustment for baseline smoking status and CRP did not change estimates for sCD163 and adiponectin. Additional adjustment for smoking did not materially change the estimates for CRP. No sex differences were found in analysis of any of the markers.
Baseline sCD163, adiponectin, CRP and time-independent associations with glucose and insulin variables
Baseline sCD163 and CRP showed a positive, and adiponectin a negative, time-independent association with fasting insulin and HOMA-IR after adjustment for age and sex (Tables 2, 3, and 4). In addition, CRP showed a positive time-independent association with 2hPG, and sCD163 a positive time-independent association with HOMA-β. The significant estimates were markedly attenuated by 30–36% for sCD163, by 35–45% for adiponectin and by 50–129% for CRP after additional adjustment for WC. All estimates remained statistically significant except for the association between adiponectin and HOMA-β. Estimates for sCD163 and adiponectin changed minimally after additional adjustment for CRP and remained statistically significant. None of the markers showed a time-independent association with HbA1c or FPG.
Analyses of effect modification by sex showed that although there was no statistically significant overall or sex-specific time-independent association between sCD163 and 2hPG, the magnitude of the effect estimate differed by sex: βwomen =−0.223 (95% CI −0.701, 0.256); βmen = 0.465, (95% CI −0.010, 0.940) (p interaction = 0.046). In addition, women had a less pronounced time-independent association between sCD163 and HOMA-IR than men (βwomen = 0.461, 95% CI 0.090, 0.832; βmen = 1.109, 95% CI 0.774, 1.444; p interaction = 0.011). No statistically significant effect modification by sex was found for any of the other analyses.
Discussion
We found markers of inflammation and adipocyte metabolism to be associated with metabolic changes in glycaemia, insulin resistance and insulin secretion among individuals at high risk of diabetes. sCD163 and CRP were positively associated with subsequent changes in insulin secretion, whereas adiponectin was inversely associated with changes in post-load glucose, insulin resistance and insulin secretion. The associations were robust to adjustment for potential confounders. We also found that sCD163, CRP and adiponectin showed time-independent associations with fasting insulin and insulin resistance, and additionally that sCD163 exhibited a time-independent association with insulin secretion, and CRP with post-load glucose. Our results may reflect the metabolic changes in fasting and post-load glucose, insulin resistance and insulin secretion found in high-risk individuals in the years before the onset of type 2 diabetes mellitus [19].
An increase in insulin resistance, accompanied by a compensatory increase in insulin secretion, is often one of the first abnormal features marking the transition between normal glucose tolerance and a trajectory leading to diabetes. It is only when this compensatory mechanism fails that levels of first post-load glucose, and later also fasting glucose, start to rise [19]. With this model in mind, our finding of an association between adiponectin and changes in post-load glucose, as well as insulin resistance and insulin secretion, may be interpreted as indicating that adiponectin is linked to a broader set of mechanisms and a wider time window in the pathogenesis of dysglycaemic progression than are sCD163 and CRP, which in our study were only associated with changes in insulin secretion and not with changes in insulin resistance or any of the glucose variables. Our findings support the hypothesis that inflammation may be involved in the pathogenesis of dysglycaemic progression in high-risk individuals and the idea that markers of inflammation and adipocyte metabolism and their specific role may vary at different stages.
The present study is to our knowledge the first to investigate the association between sCD163 and changes in glucose and insulin variables. A previous prospective study found an association between sCD163 and risk of incident type 2 diabetes mellitus in the general population during 18 years of follow-up independently of age, BMI and CRP [10]. Our findings strengthen and deepen this notion by documenting the association between sCD163 and changes in insulin secretion in individuals at high risk of diabetes. The relations remained statistically significant after adjustment for CRP, indicating that systemic low-grade inflammation does not explain the effect of sCD163 on changes in insulin secretion. We did not find any association to glucose variables, presumably because increased fasting and post-load glucose are relatively late events in the pathogenesis of dysglycaemic progression, and because participants with diabetes diagnosed during follow-up were excluded by our study design. Our finding of time-independent associations between sCD163 and insulin resistance and insulin secretion strengthens the evidence from previous cross-sectional studies [7, 20].
Our study is in agreement with other studies that found adiponectin to be negatively associated with changes in post-load glucose, insulin resistance and insulin secretion [21–23]. In the ADDITION-PRO study, we did not find any associations linking adiponectin with changes in fasting glucose, as in a previous study from Japan [23], or with changes in HbA1c, as reported in previous studies after adjustment for WC, lipids [24] and baseline fasting glucose [25]. The levels of adiponectin in the above-mentioned studies were 34–55% lower than the adiponectin level in our study and may primarily be due to the different adiponectin assays used. Although the adiponectin levels in our study are higher, any linear difference between the results of different assays is unlikely to bias the relative measures of association we report. The relationships in our study were unaffected by adjustment for CRP, indicating that systemic low-grade inflammation does not confound the association between either adiponectin or sCD163 and measures of dysglycaemia.
We found that CRP levels were positively associated with changes in insulin secretion, but not with any changes in insulin resistance or glucose variables. This is in contrast to two previous studies that found baseline CRP to be associated with changes in HbA1c during 7 years of follow-up [24] and changes in insulin resistance during 5 years of follow-up [26]. The different study populations may explain the differences as we included individuals with a high risk of diabetes, while the previous studies examined a study sample without specific selection for elevated diabetes risk. Since CRP increases less steeply over time among individuals who develop type 2 diabetes mellitus compared with controls [27], our study population may have had a less steep CRP trajectory than populations in previous studies, possibly leading to different results.
None of the previous studies examined time-independent associations, which may also lead to different results. We investigated the time-dependent and time-independent association between the biomarkers and our outcomes in a single mixed-effects model that allowed us to estimate the separate effects for the time-independent and time-dependent associations simultaneously. The time-independent estimates in our model can be compared with cross-sectional analyses, while the time-dependent estimates can be compared with analyses of change. There are, however, some important differences: time-independent outcomes refer to interindividual differences in the level of the outcome, at any age. Time-dependent outcomes refer to interindividual differences in the velocity of change as people age. In traditional cross-sectional analyses, the outcome is not only determined by contemporaneous (time-independent) mechanisms around the time of assessment, but also by the sum of time-dependent effects in the past. Our analysis approach separates these two components by regarding both baseline and follow-up measurements as expressions of the same system, at two different points in time.
Obesity, in particular abdominal obesity, is associated with low-grade inflammation and type 2 diabetes mellitus [2]. Thus, in studies of associations between low-grade inflammation and type 2 diabetes mellitus, it is important to take obesity into account as a confounding factor. As WC estimates abdominal obesity rather than total fat mass, we adjusted for WC instead of BMI. We observed that the time-independent associations were markedly reduced after adjustment for baseline WC. This phenomenon was not observed in the time-dependent associations. Our findings indicate that central obesity, by causing some degree of low-grade inflammation as well as insulin resistance, partially confounds the associations between low-grade inflammation and the levels of different measures of dysglycaemia. However, it does not attenuate the association between low-grade inflammation and the velocity of dysglycaemic progression.
Our study has several strengths. First, it is among the first studies to assess sCD163, adiponectin and CRP and the longitudinal relationship with subsequent changes in different glucose and insulin variables using mixed-effects models, thereby estimating time-independent and time-dependent associations in the same model. Second, our large study population, its representation of all relevant dysglycaemic risk levels and long follow-up period allowed us to home in on precisely the pathophysiological time window where the effects under study are most likely to play out and to describe these processes in detail.
The main limitation of our study is the different assays and methods used to quantify glucose and insulin at baseline and follow-up. Baseline glucose was measured in capillary blood, whereas follow-up glucose was measured in venous blood. Most previous studies found consistently higher glucose concentrations in capillary blood than venous blood [28–30]. As a consequence, we may have underestimated the absolute differences in fasting and post-load glucose levels, and the associations between the biomarkers and changes in glucose variables. Insulin concentrations were quantified using a different insulin assay at baseline and follow-up. Serum insulin may vary by a factor of two for median and maximum value using different assays [31]. To meet this challenge, we compared the two different assays by re-analysing follow-up insulin levels using the baseline methods. As we found a difference between insulin levels measured by the two methods, we applied a correction factor to our baseline insulin values.
Although we found associations between the biomarkers and the longitudinal change in different glucose and insulin variables, and we adjusted for relevant confounders, we cannot conclude that these associations contribute causally to the development of type 2 diabetes mellitus. First, we did not have the possibility to examine changes in glucose and insulin variables among individuals who developed type 2 diabetes mellitus during the follow-up period. As a result the influence of the biomarkers was only investigated in individuals at high risk of type 2 diabetes mellitus. Second, as in any observational epidemiological study, we cannot fully exclude reverse causation or residual confounding as explanations for our findings. Mendelian randomisation studies are needed to elucidate the causality between biomarkers of low-grade inflammation and the metabolic changes leading to type 2 diabetes mellitus. The causality of the association between adiponectin and insulin resistance and type 2 diabetes mellitus has previously been investigated in Mendelian randomisation studies, with diverging results [32, 33], while a similar study for CRP found that its relation to insulin resistance, glycaemia and type 2 diabetes mellitus was probably non-causal [34]. No Mendelian randomisation studies to date have examined the causality of the association between sCD163 and type 2 diabetes mellitus.
In conclusion, our 7 year follow-up study demonstrates that sCD163 and CRP were positively associated with insulin secretion, whereas adiponectin was inversely associated with changes in post-load glucose, insulin resistance and secretion in a population of individuals at high risk of diabetes independently of baseline abdominal obesity. Furthermore, associations of sCD163 and adiponectin were independent of systemic low-grade inflammation. Our findings indicate that mechanisms related to macrophage activation and adipocyte metabolism may play a role in changes of glucose homeostasis in individuals at high risk of type 2 diabetes mellitus.
Change history
04 December 2017
The authors have discovered a coding error in the statistical analysis syntax file used for the mixed-effect model analyses in this paper. The error has led to differences (first decimal) in the estimates for the main results.
Abbreviations
- 2hPG:
-
Two hour plasma glucose
- ADDITION-EUROPE:
-
Anglo-Danish-Dutch study of Intensive Treatment In PeOple with ScreeN-detected, Diabetes in Primary Care
- ADDITION-PRO:
-
ADDITION-Progression
- CRP:
-
C-reactive protein
- DBP:
-
Diastolic BP
- FPG:
-
Fasting plasma glucose
- MSD:
-
Meso Scale Discovery
- PE:
-
Perkin Elmer
- SBP:
-
Systolic BP
- sCD163:
-
Soluble CD163
- WC:
-
Waist circumference
References
Pickup JC, Crook MA (1998) Is type II diabetes mellitus a disease of the innate immune system? Diabetologia 41:1241–1248
Esser N, Legrand-Poels S, Piette J, Scheen AJ, Paquot N (2014) Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res Clin Pract 105:141–150
McNelis JC, Olefsky JM (2014) Macrophages, immunity, and metabolic disease. Immunity 41:36–48
Moller HJ, Peterslund NA, Graversen JH, Moestrup SK (2002) Identification of the hemoglobin scavenger receptor/CD163 as a natural soluble protein in plasma. Blood 99:378–380
Weaver LK, Hintz-Goldstein KA, Pioli PA et al (2006) Pivotal advance: activation of cell surface Toll-like receptors causes shedding of the hemoglobin scavenger receptor CD163. J Leukoc Biol 80:26–35
Moller HJ (2012) Soluble CD163. Scand J Clin Lab Invest 72:1–13
Parkner T, Sorensen LP, Nielsen AR et al (2012) Soluble CD163: a biomarker linking macrophages and insulin resistance. Diabetologia 55:1856–1862
Rojo-Martinez G, Maymo-Masip E, Rodriguez MM et al (2014) Serum sCD163 levels are associated with type 2 diabetes mellitus and are influenced by coffee and wine consumption: results of the Di@bet.es study. PLoS One 9:e101250
Zanni MV, Burdo TH, Makimura H, Williams KC, Grinspoon SK (2011) Relationship between monocyte/macrophage activation marker soluble CD163 and insulin resistance in obese and normal-weight subjects. Clin Endocrinol (Oxf) 77:385–390
Moller HJ, Frikke-Schmidt R, Moestrup SK, Nordestgaard BG, Tybjaerg-Hansen A (2011) Serum soluble CD163 predicts risk of type 2 diabetes in the general population. Clin Chem 57:291–297
Wang ZV, Scherer PE (2016) Adiponectin, the past two decades. J Mol Cell Biol 8:93–100
Ruan H, Dong LQ (2016) Adiponectin signaling and function in insulin target tissues. J Mol Cell Biol 8:101–109
Ghoshal K, Bhattacharyya M (2015) Adiponectin: probe of the molecular paradigm associating diabetes and obesity. World J Diabetes 6:151–166
Sandbaek A, Griffin SJ, Rutten G et al (2008) Stepwise screening for diabetes identifies people with high but modifiable coronary heart disease risk. The ADDITION study. Diabetologia 51:1127–1134
Johansen NB, Hansen AL, Jensen TM et al (2012) Protocol for ADDITION-PRO: a longitudinal cohort study of the cardiovascular experience of individuals at high risk for diabetes recruited from Danish primary care. BMC Public Health 12:1078
D’Orazio P, Burnett RW, Fogh-Andersen N et al (2005) Approved IFCC recommendation on reporting results for blood glucose (abbreviated). Clin Chem 51:1573–1576
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Wallace TM, Levy JC, Matthews DR (2004) Use and abuse of HOMA modeling. Diabetes Care 27:1487–1495
Tabak AG, Jokela M, Akbaraly TN, Brunner EJ, Kivimaki M, Witte DR (2009) Trajectories of glycaemia, insulin sensitivity, and insulin secretion before diagnosis of type 2 diabetes: an analysis from the Whitehall II study. Lancet 373:2215–2221
Fjeldborg K, Christiansen T, Bennetzen M, J Moller H, Pedersen SB, Richelsen B (2013) The macrophage-specific serum marker, soluble CD163, is increased in obesity and reduced after dietary-induced weight loss. Obesity (Silver Spring) 21:2437–2443
Thamer C, Haap M, Heller E et al (2006) Beta cell function, insulin resistance and plasma adiponectin concentrations are predictors for the change of postprandial glucose in non-diabetic subjects at risk for type 2 diabetes. Horm Metab Res 38:178–182
Bennett NR, Boyne MS, Cooper RS et al (2009) Impact of adiponectin and ghrelin on incident glucose intolerance and on weight change. Clin Endocrinol (Oxf) 70:408–414
Yamamoto Y, Hirose H, Saito I, Nishikai K, Saruta T (2004) Adiponectin, an adipocyte-derived protein, predicts future insulin resistance: two-year follow-up study in Japanese population. J Clin Endocrinol Metab 89:87–90
Kluppelholz B, Thorand B, Koenig W et al (2015) Association of subclinical inflammation with deterioration of glycaemia before the diagnosis of type 2 diabetes: the KORA S4/F4 study. Diabetologia 58:2269–2277
Tabak AG, Brunner EJ, Miller MA et al (2009) Low serum adiponectin predicts 10-year risk of type 2 diabetes and HbA1c independently of obesity, lipids, and inflammation: Whitehall II study. Horm Metab Res 41:626–629
Park K, Steffes M, Lee DH, Himes JH, Jacobs DR Jr (2009) Association of inflammation with worsening HOMA-insulin resistance. Diabetologia 52:2337–2344
Tabak AG, Kivimaki M, Brunner EJ et al (2010) Changes in C-reactive protein levels before type 2 diabetes and cardiovascular death: the Whitehall II study. Eur J Endocrinol 163:89–95
Carstensen B, Lindstrom J, Sundvall J, Borch-Johnsen K, Tuomilehto J, DPS Study Group (2008) Measurement of blood glucose: comparison between different types of specimens. Ann Clin Biochem 45:140–148
Kuwa K, Nakayama T, Hoshino T, Tominaga M (2001) Relationships of glucose concentrations in capillary whole blood, venous whole blood and venous plasma. Clin Chim Acta 307:187–192
Kruijshoop M, Feskens EJ, Blaak EE, de Bruin TW (2004) Validation of capillary glucose measurements to detect glucose intolerance or type 2 diabetes mellitus in the general population. Clin Chim Acta 341:33–40
Manley SE, Stratton IM, Clark PM, Luzio SD (2007) Comparison of 11 human insulin assays: implications for clinical investigation and research. Clin Chem 53:922–932
Gao H, Fall T, van Dam RM et al (2013) Evidence of a causal relationship between adiponectin levels and insulin sensitivity: a Mendelian randomization study. Diabetes 62:1338–1344
Yaghootkar H, Lamina C, Scott RA et al (2013) Mendelian randomization studies do not support a causal role for reduced circulating adiponectin levels in insulin resistance and type 2 diabetes. Diabetes 62:3589–3598
Brunner EJ, Kivimaki M, Witte DR et al (2008) Inflammation, insulin resistance, and diabetes—Mendelian randomization using CRP haplotypes points upstream. PLoS Med 5, e155
Acknowledgements
The authors would like to thank N. H. Bruun and A. Hulman, Department of Public Health, Aarhus University, Denmark, for their excellent statistical assistance, and K. B. Pedersen and H. H. Ryom, Department of Clinical Biochemistry, Aarhus University Hospital, Aarhus, Denmark for their excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
ADDITION-Denmark was supported by the National Health Services in the counties of Copenhagen, Aarhus, Ringkøbing, Ribe and South Jutland in Denmark, the Danish Council for Strategic Research, the Danish Research Foundation for General Practice, Novo Nordisk Foundation, the Danish Fund of the Danish Health and Medicines Authority, the Danish Medical Research Council and the Aarhus University Research Foundation. ADDITION-Denmark has been given unrestricted grants from Novo Nordisk AS, Novo Nordisk Scandinavia AB, Novo Nordisk UK, ASTRA Denmark, Pfizer Denmark, Glaxo Smith Kline Pharma Denmark, Servier Denmark A/S and HemoCue Denmark A/S. ADDITION-PRO was supported by unrestricted grants from the European Foundation for the Study of Diabetes/Pfizer for Research into Cardiovascular Disease Risk Reduction in Patients with Diabetes (74550801), by the Danish Council for Strategic Research and by internal research and equipment funds from the Steno Diabetes Center. The present study was supported by Aarhus University and the Danish Strategic Research Council (TRAIN project). The funding bodies played no role in the design, collection, analysis and interpretation of the data, in the writing of the manuscript or in the decision to submit for publication.
Duality of interest
MEJ is employed by Steno Diabetes Center A/S, which is a research and teaching hospital collaborating with the Danish National Health Service and owned by Novo Nordisk A/S. MEJ is principal investigator of a diabetes prevention trial sponsored by Astra Zeneca. MEJ holds shares in Novo Nordisk A/S. NBJ and DRW were supported by the Danish Diabetes Academy, which is funded by the Novo Nordisk Foundation. The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
All authors made substantial contributions to one or more of the following: the study concept and design (PD, DRW, HJM, MVS, BR, AS), acquisition of data or analysis (PD, DRW, HJM, MVS, BR, MEJ, NBJ, AS) and interpretation of the data (PD, DRW, HJM, MVS, BR, AS). PD drafted the paper, and all authors contributed to revising the manuscript critically for important intellectual content. All authors provided their final approval of the version to be published. PD is the guarantor of this work, and as such had full access to all data in the study and takes responsibility for the integrity of the data and the accuracy of data analysis.
Additional information
A correction to this article is available online at https://doi.org/10.1007/s00125-017-4498-6.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM
(PDF 481 kb)
Rights and permissions
About this article
Cite this article
Deichgræber, P., Witte, D.R., Møller, H.J. et al. Soluble CD163, adiponectin, C-reactive protein and progression of dysglycaemia in individuals at high risk of type 2 diabetes mellitus: the ADDITION-PRO cohort. Diabetologia 59, 2467–2476 (2016). https://doi.org/10.1007/s00125-016-4075-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-016-4075-4