Abstract
Aims/hypothesis
The aim of this study was to measure mitochondrial reactive oxygen species (ROS) production directly from skeletal muscle biopsies obtained from obese insulin-resistant non-diabetic and type 2 diabetic participants.
Methods
Ten lean healthy, ten obese non-diabetic and ten type 2 diabetic participants received a euglycaemic–hyperinsulinaemic clamp to measure whole body insulin sensitivity. Mitochondria were isolated from skeletal muscle biopsies, and mitochondrial ATP synthesis and hydrogen peroxide production were measured ex vivo under conditions that maximally stimulate ATP synthesis and ROS production using chemiluminescent and fluorescent techniques, respectively.
Results
Compared with lean controls, both obese non-diabetic and type 2 diabetic participants were resistant to insulin, and had a reduced rate of mitochondrial ATP production. Obese insulin-resistant participants had a decreased rate of mitochondrial ROS production, while ROS production rate in participants with type 2 diabetes was similar to that in lean healthy participants. In non-diabetic participants, the rate of ROS production was strongly correlated with the rate of ATP synthesis and the glucose disposal rate measured with the euglycaemic–hyperinsulinaemic clamp. The ROS/ATP ratio in obese insulin-resistant participants was similar to that in lean insulin-sensitive participants, while the ratio was significantly elevated in type 2 diabetes participants.
Conclusions/interpretation
Since, in absolute terms, the maximal capacity for mitochondrial ROS production was not increased in either obese insulin-resistant participants or in type 2 diabetic participants, these results do not favour a role for increased mitochondrial ROS production in the pathogenesis of insulin resistance in human skeletal muscle. However, care should be taken in extrapolating these ex vivo observations to the in vivo situation.
Similar content being viewed by others
Introduction
Insulin resistance in skeletal muscle is a characteristic feature of type 2 diabetes [1] and the insulin resistance (metabolic) syndrome [2, 3]. Impaired insulin signalling, as well as post-signalling defects, contribute to muscle insulin resistance in type 2 diabetes (see review by DeFronzo [4]).
Increased oxidative stress has been implicated in the pathogenesis of type 2 diabetes [5–9] and in the development of diabetic micro- and macrovascular complications [10]. Increased oxidative stress has been hypothesised to activate a variety of stress kinases, e.g. c-Jun-NH[2]-kinase (JNK), which through serine phosphorylation of insulin receptor substrate 1 (IRS-I) impair the insulin signalling cascade and lead to insulin resistance in skeletal muscle [5, 9]. Although this hypothesis has been widely promulgated to explain the development of insulin resistance in skeletal muscle, convincing evidence for increased oxidative stress in skeletal muscle in insulin-resistant participants has yet to be provided. The assumption that oxidative stress is increased in the skeletal muscle of insulin-resistant participants is based upon indirect evidence, including: [1] increased plasma and urinary levels of oxidised lipid and protein products in obese insulin-resistant and type 2 diabetic participants [11–15]; and [2] improved whole body insulin sensitivity following treatment of type 2 diabetic patients with antioxidants [16, 17]. No previous study has reported reactive oxygen species (ROS) production measured directly in skeletal muscle in insulin-resistant participants. The aim of this study was to measure ROS generation directly in skeletal muscle and to relate ROS generation to insulin sensitivity measured with the euglycaemic–hyperinsulinaemic clamp technique. Since most of the ROS in the cell originate from the mitochondria [18], we quantitated the rate of ROS production in mitochondria isolated from insulin-sensitive lean participants, insulin-resistant obese non-diabetic participants and type 2 diabetic participants.
Methods
Participants
Ten lean (BMI < 27.5 kg/m2), ten obese (BMI > 30 kg/m2) and ten type 2 diabetic participants were studied (Table 1). Lean and obese participants had a normal 75 g OGTT. Diabetic participants were treated with diet alone, or with metformin and/or sulfonylurea. No participants had ever received thiazolidinediones or insulin. All participants had normal liver, cardiopulmonary and kidney functions as determined by medical history, physical examination, screening blood tests, electrocardiogram and urinalysis. None of the non-diabetic participants was taking any medication and no participant participated in a regular exercise programme. Body weight had been stable (±2 kg) for at least 3 months before the study in all participants. The study protocol was approved by the Institutional Review Board of the University of Texas Health Science Center at San Antonio. Informed written consent was obtained from all participants before their participation. All studies were performed at the General Clinical Research Center (GCRC) of the University of Texas Health Science Center at 08:00 hours following a 10–12 h overnight fast.
OGTT
Prior to the OGTT, a catheter was placed into an antecubital vein. Blood samples were collected at –30, –15, 0, 30, 60, 90 and 120 min for the measurement of plasma glucose and insulin concentrations.
Euglycaemic–hyperinsulinaemic clamp
Before the start of the insulin clamp [19], a catheter was placed into an antecubital vein for the infusion of all test substances. A second catheter was inserted retrogradely into a vein on the dorsum of the hand, and the hand was placed into a thermoregulated box heated to 70°C. At 08:00 hours, all participants received a prime (0.925 MBq × fasting plasma glucose [mmol/l]/5)–continuous (9.25 kBq/min) infusion of [3-3H]glucose (DuPont NEN Life Science Products, Boston, MA, USA). After a 2 h (3 h in type 2 diabetic participants) basal tracer equilibration period, participants received a prime–continuous insulin infusion at the rate of 240 pmol min−1 m−2 (80 mU min−1 m−2) for 240 min. During the last 30 min of the basal equilibration period, plasma samples were taken at 5–10 min intervals for determination of plasma glucose and insulin concentrations, and [3H]glucose radioactivity. During the insulin infusion, plasma glucose concentration was measured every 5 min, and a variable infusion of 20% (wt/vol.) glucose was adjusted, based on the negative feedback principle, to maintain the plasma glucose concentration at each participant’s fasting plasma glucose level in non-diabetic participants and at ∼5.6 mmol/l in participants with type 2 diabetes, with a coefficient of variation of <5%. Plasma samples were collected every 15 min from 0 to 180 min and every 5–10 min from 180 to 240 min for the determination of plasma glucose and insulin concentrations and [3H]glucose specific activity.
Muscle biopsies
Sixty minutes before the start of the insulin clamp, when participants were at their fasting plasma glucose level, a vastus lateralis muscle biopsy (∼300 mg) was obtained under local anaesthesia (1% lidocaine) with a percutaneous needle, as previously described [20]. The muscle biopsy was placed in buffer on ice for mitochondrial isolation and measurement of mitochondrial ATP synthesis and ROS production rate.
Analytical techniques
Plasma glucose was measured by the glucose oxidase reaction (Glucose Oxidase Analyzer; Beckman, Fullerton, CA, USA). Plasma insulin concentration was measured by radioimmunoassay (Coat A Count; Diagnostic Products, Los Angeles, CA, USA). Plasma NEFA was measured by an enzymatic colorimetric method (Wako Chemicals, Neuss, Germany).
Mitochondrial purification
Mitochondria were purified from muscle tissue as previously described [21]. Mitochondrial integrity was assessed by respiratory control ratio (>6 with pyruvate) at the end of each experiment. All procedures were performed on ice and the entire isolation procedure lasted about 60–70 min. The final mitochondrial solution was kept on ice and used immediately following isolation.
Mitochondrial ATP production
Aliquots of the final mitochondrial suspension were used for measurement of mitochondrial ATP production rate with a chemiluminescent technique. The reaction mixture included a luciferin–luciferase ATP-monitoring reagent (Roche, Berlin, Germany), substrates for oxidation and 75 μmol/l ADP. Substrates added were as follows: 5 mmol/l glutamate plus 5 mmol/l malate; 10 mmol/l succinate plus 1 µmol/l rotenone. These conditions allow the measurement of the maximal mitochondrial production rate. Initially, mitochondrial aliquots were incubated at 37°C for 5 min in buffer containing (mmol/l): 124 KCl, 5 MgCl2, 2 K2HPO4, 10 HEPES at pH 7.44. Substrates were then added and the reaction was started with the addition of luciferin–luciferase with ADP. The reaction was performed in a 96-well plate and plate readings were made with Flouroskan Ascent instrument (Thermo, Boston, MA, USA). A blank well (mitochondria without substrate) was used to measure background and its value was subtracted from all other wells. All reactions for a given sample were monitored simultaneously and calibrated with addition of an ATP standard (Roche).
Mitochondrial ROS production
The maximal rate of mitochondrial ROS production was measured indirectly as H2O2 release from the mitochondria. H2O2 was determined with Amplex Red (Molecular Probes, Eugene, OR, USA), as described previously [22]. Horseradish peroxidase (1 unit/ml) (HRP), which catalyses the H2O2-dependent oxidation of non-fluorescent Amplex Red (80 µmol/l) to fluorescent Resorufin Red superoxide dismutase (Sigma, St Louis, MI, USA), was added at 30 U/ml to convert all superoxide into H2O2. This is necessary since superoxide produced outside the mitochondria reacts very rapidly with HRP and HRP–compound (I). Compound (I) is an intermediate state of peroxidases, formed by the reaction of the enzyme with H2O2. We monitored resorufin formation (Amplex Red oxidation by H2O2) at a λ excitation of 545 nm and a λ emission of 590 nm using a Fluoroskan-FL Ascent Type 374 multi-well plate reader (Labsystems, Helsinki, Finland). The slope of resorufin formation was converted into the rate of H2O2 production using a standard curve. Fluorescence remained linear, with a H2O2 concentration ranging from 0 to 2 µmol/l. The lowest H2O2 concentration detected was <1 nmol/l. Since the volume of the reaction mixture is 100 μl, the assay detects the production of 0.1 pmol H2O2. The assay was performed in 96-well plates at 100 µl per well with a measuring duration of 20 ms, every 2 s for 6 min. All samples were run in duplicate and the CV for complex I substrate was 5.4% and for succinate was 7.5%. We performed all assays at 37°C in 125 mmol/l KCl, 10 mmol/l HEPES, 5 mmol/l MgCl2 and 2 mmol/l K2HPO4 (pH 7.44), with 20–40 µg of mitochondrial protein per 100 µl of reaction buffer. H2O2 generation was completely inhibited with the mitochondrial uncoupler carbonyl cyanide 4-(trifluoromethoxy) phenylhydrazone (FCCP; 1 μmol/l) indicating that H2O2 originated from the mitochondria.
Statistical analysis and calculations
Following an overnight fast, steady-state conditions prevail; endogenous glucose production (EGP) was calculated as the [3H]glucose infusion rate (dpm/min) divided by the plasma [3H]glucose specific activity (dpm/mmol). During the insulin clamp, non-steady-state conditions for [3H]glucose specific activity prevail; the rate of glucose appearance (R a) was calculated with Steele’s equation [23]. The rate of residual EGP during the insulin clamp was calculated by subtracting the exogenous glucose infusion rate from the tracer-derived rate of glucose appearance. The insulin-stimulated total glucose disposal (TGD) rate was calculated by adding the rate of residual EGP to the exogenous glucose infusion rate and dividing by the steady-state plasma insulin concentration (SSPI) during the last hour of the insulin clamp (TGD/SSPI).
ATP synthesis rate was measured as the slope of chemiluminescence over time. The slope of the blank well (mitochondria without substrate) was subtracted from the slope obtained with any given substrate, and then normalised per mg mitochondrial protein per min. Similarly, the rate of H2O2 production was measured as the slope of fluorescence over time. The slope of the blank well was subtracted from the slope obtained with any given substrate and normalised per mg mitochondrial protein per min. All values are presented as the mean ± standard error. For comparison between groups, ANOVA was used. Statistically significant differences were confirmed by the Bonferroni test. Simple Pearson correlation was used to assess correlation between variables. All statistical analyses were performed with SPSS (version 14) (SPSS, Chicago, IL, USA) and statistical significance was considered at p < 0.05.
Results
Table 1 presents the anthropometric and metabolic characteristics of the three study groups. Participants were well matched for age and sex. Obese and type 2 diabetic participants had significantly greater BMI and lower TGD rate than lean participants. Obese and type 2 diabetic participants had similar BMI and TGD rates.
Compared with lean healthy controls, obese and type 2 diabetic participants had significantly lower rates of mitochondrial ATP synthesis with both complex I substrates (glutamate, pyruvate and palmitoyl carnitine) and complex II substrate (succinate). Figure 1 presents the rate of mitochondrial ATP synthesis with glutamate and succinate. Compared with lean healthy controls, obese and type 2 diabetic participants had significantly lower rates of mitochondrial ATP synthesis with both substrates. The rate of ATP synthesis with complex I substrate was decreased by 33%, 42% and 32%, respectively (p = 0.02) in obese participants, and by 39%, 33% and 31%, respectively (p = 0.02) in type 2 diabetic participants. ATP synthesis with succinate was decreased by 46% and 45% in obese and type 2 diabetic participants, respectively (p < 0.002).
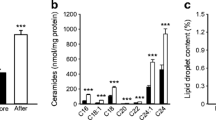
Mitochondrial ROS production was greater with complex I substrate compared with complex II substrate (Fig. 2a,b). In lean healthy individuals, the rate of ROS production with glutamate was 263 ± 55 pmol [mg protein]−1 min−1 compared with 81 ± 11 pmol [mg protein]−1 min−1 with succinate (p < 0.002). Obese participants had a significantly lower rate of ROS production with both substrates compared with lean and type 2 diabetic participants: 106 ± 16, 263 ± 56 and 216 ± 56 pmol (mg protein)−1 min−1 with glutamate and 24 ± 6, 81 ± 11 and 70 ± 18 pmol (mg protein)−1 min−1 with succinate, respectively (p < 0.05 with ANOVA, for glutamate and succinate).
When non-diabetic participants (lean and obese) were pooled, ROS production with both substrates strongly correlated with the rate of mitochondrial ATP production (r = 0.69, p < 0.001 for glutamate [Fig. 3a] and r = 0.80, p < 0.0001 for succinate [Fig. 3b]) and with TGD rate (r = 0.71, p < 0.0004 for glutamate [Fig. 4a] and r = 0.63, p < 0.002 for succinate [Fig. 4b]).
Relationship between ROS generation with complex I (glutamate plus malate) (r = 0.71, p = 0.0004) (a) and complex II (succinate plus rotenone) (r = 0.63, p < 0.002) (b) substrates vs insulin-stimulated TGD rate during the last hour of the euglycaemic–hyperinsulinaemic clamp in non-diabetic (lean plus obese) participants. SSPI, steady-state plasma insulin concentration during the last hour of the euglycaemic–hyperinsulinaemic clamp
Since mitochondrial metabolism is driven by the energy demand of the cell, and ROS generation is a by-product of normal metabolism, we calculated the ratio of ROS generation to ATP production rate. This ratio reflects the number of ROS molecules generated during the production of one ATP molecule. The ratio between mitochondrial H2O2 generation rate and mitochondrial ATP synthesis rate was 3.6 × 10−3, 2.7 × 10−3 and 6.5 × 10−3 with complex I substrate and 1.0 × 10−3, 0.8 × 10−3 and 2.6 × 10−3 with complex II substrate in lean, obese, and type 2 diabetic participants, respectively (Fig. 5) (p < 0.001 for glutamate and p < 0.05 for succinate with ANOVA).
Ratio between hydrogen peroxide generation and ATP production rate in lean insulin-sensitive participants, obese non-diabetic participants and type 2 diabetic participants (T2DM). Black bars, ratio with complex I substrate (glutamate plus malate); white bars, ratio with complex II substrate (succinate plus rotenone). *p < 0.05, ***p < 0.001 vs corresponding lean group
The relationship between ROS production and HbA1c with both glutamate and succinate was divergent in diabetic and non-diabetic individuals. In non-diabetic participants increased HbA1c levels were associated with a decrease in mitochondrial ROS production rate, while in type 2 diabetic individuals increased HbA1c levels were associated with increase in ROS production rate. Thus, the relationship between mitochondrial ROS production rate and HbA1c was described by a U-shaped curve (Fig. 6a, b).
Discussion
Increased oxidative stress has been implicated in the pathogenesis of type 2 diabetes [6], diabetic complications [10], cardiovascular disease [24], cancer and the normal ageing process [25]. Increased oxidative stress has been suggested to cause insulin resistance in skeletal muscle by activating stress kinases, e.g. JNK and nuclear factor kappa B (NFκB), that impair insulin signalling via serine phosphorylation of the insulin receptor and IRS-1 [5, 7]. Although this hypothesis has been suggested by many authors, direct evidence for increased ROS production in skeletal muscle in insulin-resistant individuals has yet to be provided. In this study we demonstrate that the maximal mitochondrial ROS production capacity in mitochondria isolated from obese non-diabetic, insulin-resistant individuals is lower than in lean normal-glucose-tolerant insulin-sensitive individuals. We also demonstrate that, in non-diabetic participants, the maximal mitochondrial ROS production capacity of both complex I and complex II is strongly correlated with the maximal rate of mitochondrial ATP production. Since obese insulin-resistant individuals have a significant decrease in mitochondrial ATP synthesis rate, and since ROS production is a by-product of the normal oxidative phosphorylation process, the decrease in mitochondrial ROS production observed in this study probably reflects the reduced rate of mitochondrial ATP synthesis associated with increased insulin resistance and decreased insulin-stimulated glucose disposal. The comparable ROS/ATP ratio in lean healthy insulin-sensitive and obese insulin-resistant individuals supports this hypothesis. Although these results demonstrate that the maximal ROS production capacity measured ex vivo is diminished, caution should be employed when extrapolating to the in vivo situation. The ratio of ROS/ATP production indicates the number of ROS molecules generated per 1000 ATP molecules synthesised. Our results demonstrate that in lean insulin-sensitive individuals, skeletal muscle mitochondria generate ∼3.5 molecules of H2O2 with complex I substrate per 1,000 ATP molecules synthesised, while, with complex II substrate, approximately one molecule of H2O2 is generated per 1000 ATP molecules synthesised. The ROS/ATP ratio in obese insulin-resistant individuals is similar to that in lean insulin-sensitive participants for both complex I substrate and complex II substrate, suggesting that the decrease in mitochondrial ROS production in obese insulin-resistant individuals is the result of decreased oxidative phosphorylation, rather than a functional change in mitochondrial activity in obese insulin-resistant participants.
Decreased mitochondrial oxidative phosphorylation has been reported in vivo using magnetic resonance spectroscopy (MRS) in a variety of insulin resistance states, including participants with a positive family history for type 2 diabetes, elderly participants and type 2 diabetic participants (see review by Schrauwen-Hinderling et al. [26]). However, the precise relationship between decreased mitochondrial oxidative phosphorylation and insulin resistance remains unclear [26–29]. Whether decreased mitochondrial function is the cause or the effect of insulin resistance or not, our results indicate that reduced oxidative phosphorylation, when measured ex vivo, is associated with a decrease in the rate of mitochondrial ROS production in skeletal muscle. If a similar decrease in mitochondrial ROS production occurred in vivo in association with the well-documented decrease in oxidative phosphorylation reported in insulin-resistant participants with MRS, this would not support a role for increased mitochondrial ROS production in the pathogenesis of muscle insulin resistance in obesity. However, even if a decrease in mitochondrial ROS production were to be demonstrated in vivo, this would not exclude a causal role of increased oxidative stress in the development of insulin resistance. Previous studies have reported increased plasma and urinary levels of products of fat and protein oxidation in obese insulin-resistant individuals [5–9]. In this regard, ROS can be generated from other sources in the body, e.g. adipocytes [30]. NADPH oxidase [31] also may contribute to the generalised increased level of oxidative stress in obese insulin-resistant individuals. Alternatively, decreased levels of defence mechanism, with an unchanged level of ROS production, could also lead to an increase in oxidative stress markers in obese insulin-resistant individuals [32].
As for obese insulin-resistant non-diabetic individuals, participants with type 2 diabetes also had a decrease in the maximal rate of mitochondrial ATP synthesis compared with lean insulin-sensitive individuals. Our observation of decreased mitochondrial ATP synthesis in diabetic participants is consistent with the reduced oxidative phosphorylation demonstrated in type 2 diabetic participants in vivo using MRS [33], and it is probably related to the insulin resistance (decreased rate of TGD) rather than to the diabetic state, since a similar decrease was observed in the obese insulin-resistant non-diabetic participants. Because our study is cross-sectional, we can not determine what is the cause and what is the effect. However, unlike the obese participants, the maximum rate of ROS production ex vivo in type 2 diabetes was normal when viewed in absolute terms, and, when expressed relative to the rate of ATP production, ROS generation was increased twofold compared with obese individuals (6.5-fold for complex I and 2.6-fold for complex II in type 2 diabetic participants compared with 3.6- and 1.0-fold in lean and 2.7- and 0.8-fold in obese individuals, respectively). These results indicate that, relative to their metabolic rate, type 2 diabetic participants had an increased rate of mitochondrial ROS production ex vivo compared with age- and BMI-matched non-diabetic participants. However, it should be emphasised that the present studies were carried out ex vivo, and muscle ROS production has yet to be measured in vivo. It also should be noted that under our experimental conditions, which used saturating substrate concentrations, mitochondrial ATP synthesis rate and ROS generation are maximally stimulated. However, under physiological conditions in vivo, the mitochondria operate under sub-maximal conditions and mitochondrial metabolism is driven by the cellular energy demand (ATP/ADP ratio). Thus, our data indicate that for the production of the same amount of ATP, type 2 diabetes participants generated twice the amount of ROS than did non-diabetic participants, both insulin-sensitive (lean) and insulin-resistant (obese). Since type 2 diabetic participants have rates of ATP production and insulin-stimulated glucose disposal rates that are reduced similarly to those in obese insulin-resistant non-diabetic individuals, our results indicate that the increased ROS/ATP production ratio in type 2 diabetic participants is probably the result of some aspect of the diabetic state. Moreover, the increase in ROS production relative to the rate of total body glucose disposal and ATP synthesis is consistent with the hypothesis that oxidative stress is increased in diabetic participants and may play a role in the development of diabetic vascular complications [10].
Although the molecular defect that could be responsible for ATP synthesis rate and increased ROS production in participants with type 2 diabetes has yet to be defined, a defect in complex V could explain the results. Thus, a decrease in complex V activity in participants with type 2 diabetes would result in a decreased rate of mitochondrial ATP synthesis accompanied by an increased proton gradient across the inner mitochondrial membrane, leading to an increase in the rate of ROS production. Consistent with this hypothesis, a recent study [34] has reported an increased rate of phosphorylation of mitochondrial complex V in diabetic participants compared with lean healthy controls. However, complex V activity was not reported in that study. It remains to be seen whether a change in the phosphorylation state of mitochondrial complex V could explain the current results (increased ROS production and decreased ATP synthesis) in type 2 diabetic participants.
A limitation of the present study is that the measurement of mitochondrial function was performed ex vivo. Removal of the mitochondria from their physiological environment could alter their metabolic characteristics. In addition to the change in substrate availability, which is an important regulator of mitochondrial activity, removal of intracellular metabolites that could influence mitochondrial activity could also alter mitochondrial metabolism. For example, we have shown previously that elevated concentrations of fatty acyl Co-A inhibit oxidative phosphorylation in skeletal muscle mitochondria, and an increased level of intracellular fatty acyl Co-A has been reported in both type 2 diabetic and obese non-diabetic insulin-resistant individuals compared with lean insulin-sensitive participants [21]. Thus, mitochondrial metabolism measured in vivo may differ from that measured ex vivo. However, at present there is no in vivo method to measure ROS production.
It is noteworthy that in humans the rate of ROS production in complex I is about threefold greater than that of complex II. This rate of ROS production is in marked contrast to that observed in rodents, where the rate of ROS production in complex II is about twice that of complex I [22]. Since complex II produces superoxide to both sides of the inner mitochondrial membrane [35] while complex I produces superoxide only toward the inner mitochondrial matrix, this suggests that, for the same level of metabolism, the level of cytosolic oxidative stress would be greatly (five- to sixfold) increased in rodents compared with humans.
In conclusion, we have demonstrated in this study that the maximal mitochondrial ROS production capacity measured ex vivo in obese and type 2 diabetic participants is not increased, in absolute terms, in mitochondria isolated from skeletal muscle. However, the ratio of ROS/ATP production in obese non-diabetic participants is similar to that in lean healthy individuals, and increased in participants with type 2 diabetes. Taken together, these results do not favour a role for increased mitochondrial ROS production in the development of insulin resistance. However, the present results were obtained under ex vivo conditions. In vivo measurement of mitochondrial ROS production will be necessary to validate the relevance of the present observations. Unfortunately, the measurement of muscle ROS production in vivo is not currently feasible.
Abbreviations
- EGP:
-
endogenous glucose production
- MRS:
-
magnetic resonance spectroscopy
- ROS:
-
reactive oxygen species
- TGD:
-
total glucose disposal
References
DeFronzo RA (2004) Pathogenesis of type 2 diabetes mellitus. Med Clin North Am 88:787–835
DeFronzo RA (1997) Insulin resistance: a multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidaemia and atherosclerosis. Neth J Med 50:191–197
Reaven GM (1988) Banting lecture 1988. Role of insulin resistance in human disease. Diabetes 37:1595–1607
DeFronzo RA (1997) Pathogenesis of type 2 diabetes mellitus: metabolic and molecular implications for identifying diabetes genes. Diabetes Rev 5:117–269
Bloch-Damti A, Bashan N (2005) Proposed mechanisms for the induction of insulin resistance by oxidative stress. Antioxid Redox Signal 7:1553–1567
Evans JL, Goldfine ID, Maddux BA, Grodsky GM (2003) Are oxidative stress-activated signaling pathways mediators of insulin resistance and beta-cell dysfunction? Diabetes 52:1–8
Evans JL, Maddux BA, Goldfine ID (2005) The molecular basis for oxidative stress-induced insulin resistance. Antioxid Redox Signal 7:1040–1052
Houstis N, Rosen ED, Lander ES (2006) Reactive oxygen species have a causal role in multiple forms of insulin resistance. Nature 440:944–948
Wei Y, Chen K, Whaley-Connell AT, Stump CS, Ibdah JA, Sowers JR (2008) Skeletal muscle insulin resistance: role of inflammatory cytokines and reactive oxygen species. Am J Physiol 294:R673–R680
Brownlee M (2001) Biochemistry and molecular cell biology of diabetic complications. Nature 414:813–820
Hitsumoto T, Iizuka T, Takahashi M et al (2003) Relationship between insulin resistance and oxidative stress in vivo. J Cardiol 42:119–127
Katsuki A, Sumida Y, Urakawa H et al (2004) Increased oxidative stress is associated with serum levels of triglyceride, insulin resistance, and hyperinsulinemia in Japanese metabolically obese, normal-weight men. Diabetes Care 27:631–632
Lee KU (2001) Oxidative stress markers in Korean subjects with insulin resistance syndrome. Diabetes Res Clin Pract 54(Suppl 2):S29–S33
Meigs JB, Larson MG, Fox CS, Keaney JF Jr, Vasan RS, Benjamin EJ (2007) Association of oxidative stress, insulin resistance, and diabetes risk phenotypes: the Framingham Offspring Study. Diabetes Care 30:2529–2535
Urakawa H, Katsuki A, Sumida Y et al (2003) Oxidative stress is associated with adiposity and insulin resistance in men. J Clin Endocrinol Metab 88:4673–4676
Jacob S, Henriksen EJ, Schiemann AL et al (1995) Enhancement of glucose disposal in patients with type 2 diabetes by alpha-lipoic acid. Drug Res 45:872–874
Jacob S, Ruus P, Hermann R et al (1999) Oral administration of rac-α-lipoic acid modulates insulin sensitivity in patients with type 2 diabetes mellitus a placebo controlled pilot trial. Free Radic Biol Med 27:309–314
Jackson MJ, Pye D, Palomero J (2007) The production of reactive oxygen and nitrogen species by skeletal muscle. J Appl Physiol 102:1664–1670
DeFronzo RA, Tobin JD, Andres R (1979) Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol 237:E214–E223
Cusi K, Maezono K, Osman A et al (2000) Insulin resistance differentially affects the PI 3-kinase- and MAP kinase-mediated signaling in human muscle. J Clin Invest 105:311–320
Abdul-Ghani MA, Muller FL, Liu Y et al (2008) Deleterious action of FA metabolites on ATP synthesis: possible link between lipotoxicity, mitochondrial dysfunction and insulin resistance. Am J Physiol 295:E678–E685
Muller FL, Liu Y, Abdul-Ghani MA et al (2008) High rates of superoxide production in skeletal-muscle mitochondria respiring on both complex I- and complex II-linked substrates. Biochem J 409:491–499
Steele RW, Wall JS, DeBodo RC, Altszuler N (1956) Measurement of size and turnover rate of body glucose pool by the isotope dilution method. Am J Physiol 187:15–24
Zalba G, Fortuño A, San José G, Moreno MU, Beloqui O, Díez J (2007) Oxidative stress, endothelial dysfunction and cerebrovascular disease. Cerebrovasc Dis 24(Suppl 1) 1:24–29
Ishii N (2007) Role of oxidative stress from mitochondria on aging and cancer. Cornea 9(Suppl 1):S3–S9
Schrauwen-Hinderling VB, Roden M, Kooi ME, Hesselink MK, Schrauwen P (2007) Muscular mitochondrial dysfunction and type 2 diabetes mellitus. Curr Opin Clin Nutr Metab Care 10:698–703
Phielix E, Schrauwen-Hinderling VB, Mensink M et al (2008) Lower intrinsic ADP-stimulated mitochondrial respiration underlies in vivo mitochondrial dysfunction in muscle of male type 2 diabetic patients. Diabetes 57:2943–2949
Asmann YW, Stump CS, Short KR et al (2006) Skeletal muscle mitochondrial functions, mitochondrial DNA copy numbers, and gene transcript profiles in type 2 diabetic and nondiabetic subjects at equal levels of low or high insulin and euglycemia. Diabetes 55:3309–3319
Pospisilik JA, Knauf C, Joza N et al (2007) Targeted deletion of AIF decreases mitochondrial oxidative phosphorylation and protects from obesity and diabetes. Cell 131:476–491
Furukawa S, Fujita T, Shimabukuro M et al (2004) Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest 114:1752–1761
Fortuño A, San José G, Moreno MU, Beloqui O, Díez J, Zalba G (2006) Phagocytic NADPH oxidase overactivity underlies oxidative stress in metabolic syndrome. Diabetes 55:209–215
Paolisso G, Di Maro G, Pizza G et al (1992) Plasma GSH/GSSG affects glucose homeostasis in healthy subjects and non-insulin-dependent diabetics. Am J Physiol 263:E435–E440
Szendroedi J, Schmid AI, Chmelik M et al (2007) Muscle mitochondrial ATP synthesis and glucose transport/phosphorylation in type 2 diabetes. PLoS Med 4:e154
Hojlund K, Yi Z, Lefort N et al (2008) Identification of multiple phosphorylation sites on ATP synthase β subunit in human muscle. Increased phosphorylation at Thr213 and Tyr361 in obesity and type 2 diabetes. Diabetes 57(Suppl I):A19 (Abstract)
Muller FL, Liu Y, Van Remmen H (2004) Complex II releases superoxide to both sides of the inner mitochondrial membrane. J Biol Chem 279:49064–49073
Acknowledgements
We would like to thank our GCRC nurses for their assistance in performing these studies and K. Delgado and L. Albarado (University of Texas Health Center at San Antonio) for their help in preparing the manuscript. This work was supported by NIH grant 24092, a VA Merit Award (R.A. DeFronzo) and GCRC grant RR01346.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abdul-Ghani, M.A., Jani, R., Chavez, A. et al. Mitochondrial reactive oxygen species generation in obese non-diabetic and type 2 diabetic participants. Diabetologia 52, 574–582 (2009). https://doi.org/10.1007/s00125-009-1264-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-009-1264-4