Abstract
Gene therapy has entered a new era after decades-long efforts, where the recombinant adeno-associated virus (AAV) has stood out as the most potent vector for in vivo gene transfer and demonstrated excellent efficacy and safety profiles in numerous preclinical and clinical studies. Since the first AAV-derived therapeutics Glybera was approved by the European Medicines Agency (EMA) in 2012, there is an increasing number of AAV-based gene augmentation therapies that have been developed and tested for treating incurable genetic diseases. In the subsequent years, the United States Food and Drug Administration (FDA) approved two additional AAV gene therapy products, Luxturna and Zolgensma, to be launched into the market. Recent breakthroughs in genome editing tools and the combined use with AAV vectors have introduced new therapeutic modalities using somatic gene editing strategies. The promising outcomes from preclinical studies have prompted the continuous evolution of AAV-delivered therapeutics and broadened the scope of treatment options for untreatable diseases. Here, we describe the clinical updates of AAV gene therapies and the latest development using AAV to deliver the CRISPR components as gene editing therapeutics. We also discuss the major challenges and safety concerns associated with AAV delivery and CRISPR therapeutics, and highlight the recent achievement and toxicity issues reported from clinical applications.
Similar content being viewed by others
Development of AAV vector for gene therapy
Adeno-associated virus (AAV) is a small, non-enveloped, single-stranded DNA virus that belongs to the genus Dependovirus in the Parvovirus family. AAV was initially discovered in 1965 as a contaminant of an adenovirus (AdV) preparation [1], and later identified as a new infectant after antibodies to different AAV serotypes were detected in children [2]. As a dependovirus, AAV is replication-defective in the absence of a helper virus such as adenovirus or herpes virus. During the latent phase, AAV will integrate into the host cell genome and remain dormant until co-infection occurs and triggers viral replication [3]. The wild-type AAV (wtAAV) contains a single-stranded DNA genome approximately 4.7 kb in length, which consists of rep and cap genes flanked by two inverted terminal repeats (ITRs). In later years, studies found that the AAV genes could be expressed without integration, and a recombinant DNA sequence between the AAV2 ITRs in an engineered vector could be successfully encapsulated into pseudovirus by providing rep and cap genes in trans [3]. As a result, the engineered AAV vectors possess the capacity to carry a recombinant genome up to ~ 4.7 kb, and can be pseudotyped with ease using different cap genes to generate virions with desired tissue tropisms. Similar to wtAAVs, the recombinant AAVs are low-immunogenic and non-pathogenic, while due to the lack of other viral elements, the AAV vector genome largely remains non-integrative in host cells. Collectively, these features make the AAV system an ideal delivery tool for in vivo gene transfer and gene augmentation therapy [4].
The first AAV-based in vivo gene delivery was reported in 1993 when Flotte et al. stably expressed cystic fibrosis membrane conductance regulator (CFTR) in rabbit lung for up to 6 months [5]. The promising results led to the first phase I clinical trial of AAV-based gene therapy in 1996 which delivered the CFTR gene for treating patients with cystic fibrosis [6]. In 2000, another early study reported the successful delivery of human factor IX (hFIX) using AAV vectors to ameliorate the bleeding symptoms in patients with hemophilia B [7], although the follow-up study of these patients revealed elevated levels of neutralizing antibodies (NAbs) against AAV vectors, which abolished the long-term efficacy of the treatment [8]. As a result, subsequent studies focused on exploring various strategies to overcome the issues associated with adaptive immune responses to AAV vectors. Eventually, successful therapeutic gene transfer was achieved by selectively recruiting patients with low NAbs and administrating short-term anti-T cell immunosuppressive agents [9, 10].
Recent progress of AAV-based gene therapy in clinics
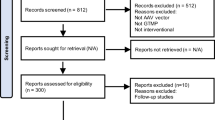
Over the last decade, AAV gene therapy has accomplished remarkable progress and is finding its way into medical practice (Fig. 1). In 2012, the European Medicines Agency (EMA) approved the first-ever AAV-based gene therapy Glybera [11], a recombinant AAV product that delivers the human lipoprotein lipase (LPL) gene to treat hereditary lipoprotein lipase deficiency (LPLD) [12]. Five years later, Luxturna (voretigene neparvovec-rzyl), another AAV gene therapy for RPE65-mediated inherited retinal dystrophy, was approved by the United States Food and Drug Administration (FDA) and entered the US market [13, 14]. Recently, Zolgensma (onasemnogene abeparvovec), an AAV product delivering a functional copy of the SMN1 gene for spinal muscular atrophy type 1 (SMA1), was approved by the FDA in 2019 and became the third AAV-based gene therapy product in the market [15,16,17] (Table 1).
Numbers of clinical trials using AAV vectors for gene transfer. *Data were obtained from http://www.abedia.com/wiley/index.html
The continuous development of AAV vectors has provided an excellent treatment modality for inherited ocular disorders. The eye is considered an attractive target organ due to (i) high accessibility for AAV delivery; (ii) immune-privileged environment maintained by the blood-retinal barrier; and (iii) enclosed structure and small tissue size which allows using lower vector dose to achieve therapeutic benefits [18]. As a result, the number of new clinical trials for ocular gene therapies has been steadily increasing for the past 5 years. Among the ongoing trials, approximately 80% are currently in phase 1/2, with estimated 70% (more than 40 trials) that are using AAV vectors (https://clinicaltrials.gov/) [18].
Gene therapy trials for hemophilia have been actively pursued since the 1990s. The earlier trials showed that AAV delivery was well tolerated in human patients with transient elevation of liver enzymes which then returned to the normal level without manifesting adverse side effects [7]. The clinical data also revealed that the presence of NAbs against natural AAVs abolished the efficacy of the AAV vector-delivered treatment [8]. These findings suggested to adopt strategies such as selective recruitment of patients with low NAbs and co-administration with a short-term anti-T cell suppressants in subsequent clinical trials, which eventually led to the first long-term success for hemophilia B gene therapy in 2011 [9, 10]. The study recruited patients with severe hemophilia B and divided them into three groups to receive a single dose of scAAV2/8-LP1-hFIXco vectors at 2 × 1011, 6 × 1011, and 2 × 1012 vg/kg. The patients from all groups exhibited a stable dose-dependent increase in FIX levels [10]. Markedly, in the high-dose cohort, all six patients showed a consistent increase of plasma FIX that reached 5.1 ± 1.7% of normal level together with bleeding episodes reduced by more than 90% [10]. Seven years later, a follow-up investigation confirmed stable maintenance of the FIX levels and hemostasis in all of these patients [19]. These promising results prompted subsequent clinical trial programs to optimize the AAV delivery and input dose. UniQure carried out a clinical trial delivering the scAAV2/8-LP1-hFIXco vector using AAV5 capsid (AMT-060) at the dose of 5 × 1012 and 2 × 1013 vg/kg, and achieved therapeutic efficacy and safety profile similar to the previous clinical trial using the AAV8 capsid (NCT02396342; EudraCT2013-005579-42) [20]. Spark Therapeutics used a modified-AAV8 capsid (SPK-9001) to deliver hyperactive FIX variant (R338L) Padua in a clinical trial for hemophilia B, which further reduced the input dose (5 × 1011 vg/kg) to achieve sustained FIX activity at around 33.7 ± 18.5% of the normal level [21]. These results provided the data necessary for expanding the clinical trial for SPK-9001 into phase 3 (NCT03587116) as well as testing AAV5- and AAVS3-delivered hFIX-Pauda (NCT03489291, NCT03369444) in new phase 1 trials, where long-term monitoring will be necessary to determine the efficacy of the treatment [22].
The advancement of AAV gene therapy for hemophilia B has also expedited the approvals of clinical trials for hemophilia A. In 2017, BioMarin Pharmaceutical reported the success of their first phase 1/2 clinical trial using AAV5 to deliver the codon-optimized B domain-deleted F8 cDNA (BDD-FVIII) (BMN 270) into patients with severe hemophilia A and achieved FVIII activity at around 77% of the normal level in the high-dose (6 × 1013 vg/kg)-treated group [23]. Immediately, BioMarin expanded the testing of BMN270 into two phase 3 trials, with an estimated 170 patients enrolled for the studies (NCT03370913, NCT03392974). In the following year, Spark Therapeutics quickly followed and unveiled the outcome of their phase 1/2 clinical trial using an engineered capsid AAV-LK03 to deliver BDD-FVIII (SPK-8011) with five out of seven patients treated with the high-dose vectors (2 × 1012 vg/kg) exhibited FVIII at 16–49% of the normal levels [24].
The research using hemophilia as a study model has pioneered liver-based gene therapy [22, 25]. The promising results from optimizing different aspects of recombinant AAV for gene delivery, including vectors, capsids, route, dose, toxicity, and immunogenicity, have paved the way for developing gene therapy for many other liver-based inherited diseases which have led to a number of clinical trials to date [26]. These include the AAV-based treatments for alpha 1-antitrypsin (AAT) deficiency, phenylketonuria (PKU), ornithine transcarbamylase deficiency, Crigler-Najjar syndrome, homozygous familial hypercholesterolemia (FH), and glycogen storage disease type Ia (GSD1a) (https://clinicaltrials.gov/) [27, 28].
A number of trials have also been undertaken to explore the therapeutic potential of AAV-based gene delivery into the central nervous system (CNS) to treat various neurological disorders. In the past, AAV delivery targeting the CNS had been challenging due to the protection of the blood-brain barrier (BBB). Since 2009, a series of studies have addressed the issue of BBB by delivering the AAV9 vectors through the intracerebroventricular or intravenous route, which yielded significant GFP expression in mouse CNS and achieved therapeutic expression of SMN, a gene responsible for the inherited neuromuscular disorder SMA1 [29, 30]. Notably, clinical testing on the AAV9-delivered SMN expression for treating SMA1 [31] has led to the remarkable success of Zolgensma, the AAV gene therapy product approved by the FDA in Dec 2019 [17]. Currently, AAV vectors have been tested in clinical trials for a number of neurological disorders. AAV-based gene therapy using AAV9 and AAVrh10 vectors for Sanfilippo syndrome type A (MPSIIIA) had passed safety tests and entered phase 2/3 clinical trials (NCT04360265; NCT03612869) [32]. Additionally, AAV2-delivered aromatic l-amino acid decarboxylase (AADC) gene therapy has completed phase 1/2 trial for pediatric patients with AADC deficiency (NCT02852213, NCT02926066) [33]. The safety profile and therapeutic potential of AAV-based gene therapy in monogenic neurological disorders have prompted researchers to expand gene therapy clinical trials to treat more complex neurological diseases, such as Parkinson’s disease and Alzheimer’s disease (https://clinicaltrials.gov/) [34].
It is noteworthy that hemophilia is low-hanging fruit because a very low level of gene transfer and expression is sufficient to confer therapeutic benefits [22, 25]. In many other diseases, much higher AAV doses are needed to convey therapeutic benefits from transgenes expression and have been reported to be associated with severe toxicity [15, 16, 26]. In a recent study, a clinical trial named “AT132” injected AAV8 at 1 × 1014 and 3 × 1014 vg/kg to treat X-linked myotubular myopathy (NCT03199469). Six patients treated with low-dose AAV8 showed significant improvement in motor functions. However, three boys from the high-dose group all died from progressive liver dysfunction followed by sepsis [35]. These clinical deaths highlight the risks associated with intravenous administration of high-dose AAVs and prompt a more thorough assessment for patient recruitment, such as taking account of genetic pre-deposition and pre-existing liver disease [36] (Table 2). Together, further investigations are warranted to reduce input dose; the strategies include but are not limited to (i) enhancing transgene expression, (ii) improving viral capsid and cell-type-specific promoters, and (iii) administrating immunosuppressive agents to eliminate NAbs.
The current limitations and future of AAV-based gene therapy
Rapid loss of episomal AAV vectors in proliferating cells
The recombinant AAV vectors do not integrate into the host DNA but mainly remain as episomes in the transduced cells to stably express transgene for a prolonged period in somatic tissues [45]. However, among the tissues that are at either a growing stage or undergoing continuous turnover, cell proliferation will result in a fast and significant loss of transgene expression due to the dilution of non-replicative AAV vectors [46]. As a result, AAV-based gene delivery is rarely used to target fast-proliferating cells such as hematopoietic progenitors and stem cells. Evidences from multiple clinical studies on AAV-based gene therapy in adult patients with hemophilia B have also reported expression loss, despite a significant reduction in bleeding episodes [26]. Young children are seldom recruited in clinical trials for AAV-based gene therapy due to general safety concerns as well as vector dilution [10, 21]. Currently, there is limited data on the long-term efficacy of AAV gene therapy for the younger age group, which, therefore, warrants further investigations to overcome the challenges as mentioned above.
Small packaging capacity of AAV vectors for in vivo gene delivery
Recombinant AAVs are the leading platform for in vivo gene delivery. The most commonly used AAV vector is derived from wtAAV2 with a maximum packaging capacity of ~ 4.7 kb [4]. Several genes used in gene therapy such as dystrophin (for Duchenne muscular dystrophy), FVIII (for hemophilia A), and ABCA4 (for an inherited retinal degeneration) exceed the packaging capacity of AAV and, hence, are difficult to be packaged efficiently. To overcome the size limitation, truncated versions of the transgenes, such as the BDD-FVIII, together with mini promoters and polyA signals, were generated [23]. However, the gene truncation approach was not applicable to the mini-dystrophin gene with a size range of 6–8 kb after the removal of multiple internal regions [47]. Zhang et al. reported a dual-AAV vector approach to deliver split mini-dystrophin genes that will undergo trans-splicing to synthesize the mini-dystrophin protein inside the host cells [48], based on the rationale that the AAV genome undergoes concatemerization in host cells through homologous recombination between their ITR sequences [49]. In order to improve the transfer efficiency of larger genes, intein-mediated trans-splicing technology was also developed [50] and has shown promising gene transfer efficiency in preclinical studies [47, 51].
AAV vector engineering has also aimed at overcoming the slow onset of transgene expression attributed to the time-consuming conversion of single-stranded to double-stranded AAV genome [52]. The rate-limiting step of second-strand synthesis was resolved by introducing mutations into the ITR regions to prevent terminal resolution, thereby promoting self-complementation [53]. The generation of self-complementary AAV (scAAV) vectors allows quicker expression and greater persistence in target cells [53, 54]. The clinical application of scAAV has contributed to the aforementioned triumphant in achieving long-term therapeutic benefits in AAV gene therapy for hemophilia B [9, 10] and the FDA approval of Zolgensma [15,16,17].
Host immune response against AAV
AAVs are highly prevalent, with up to 70% of the world population are positive for AAV serotype 2. Although AAVs have not been reported to cause any clinical disease, humans infected with AAVs often develop immunological memory that renders AAV-based gene therapy ineffective [55].
Humoral immunity against AAV
It is estimated that a considerable proportion of individuals will develop humoral immunity against wtAAV in their lifetime [56]. Among the thirteen naturally occurring AAV serotypes, approximately 70% of the world population are seropositive for AAV1 and AAV2, 45% for AAV6 and AAV9, and 38% for AAV8 [55]. The prevalence of individual serotypes varies across geographical locations [57]. Infants often carry maternal anti-AAV antibodies which decline gradually in a few months after birth [58]. In AAV-based gene therapy, the pre-existing anti-AAV antibodies will recognize and prevent the AAV capsid epitopes from interacting with receptors on the recipient cells, and thus can have a profound impact on cellular transduction and gene delivery efficiencies [59]. Although the pre-existing NAbs may not inhibit gene transfer administered via the eye or parenchyma route, intravenous gene therapy for hemophilia has shown that low titers of pre-existing anti-AAV antibodies are sufficient to neutralize the AAV vectors and abolish the treatment efficacy [60, 61]. Nowadays, prescreening is routinely conducted on clinical trial subjects before receiving AAV-based gene therapy, where subjects with high NAbs, approximately 20–50% in the tested patients as estimated based on the NAbs prelavance [55], are excluded from participating in the majority of the studies [62]. Moreover, re-administration of the same AAV vector is challenging, as previously treated patients develop NAbs which inhibit the efficacy of subsequent treatment [8, 63]. Currently, several clinical trials are testing multiple AAV capsids from different AAV serotypes to deliver the hFIX and hFIX-Padua genes [22, 25, 26] to avoid being targeted by pre-existing NAbs. Generally, NAbs are specific to individual AAV capsids [63]. However, seroprevalence analysis showed that some NAbs exhibited broad cross-reactivity [64], which could render AAV serotypes switching ineffective.
Cellular immunity against AAV
AAV alone does not induce significant inflammatory reactions to trigger cellular immune response. Whereas, AAV co-infected with helper viruses will activate CD4+ and CD8+ T cells which then leaves a pool of memory T cells throughout the lifetime [65]. The number of people with pre-existing memory T cell to wtAAVs is far lesser than those carrying NAbs, but the presence of these AAV-specific memory T cells contributes to the different responses to the AAV treatement as observed in human and experimental animals [62]. Unlike the NAbs that are largely specific to individual capsids, the memory T cells recognize AAV epitopes that are highly conserved across serotypes [66]. Fortunately, gene therapy studies in patients with hemophilia B demonstrated the effectiveness of using immunomodulating drugs to temporarily suppress T cell responses to the AAV capsids [9, 10], and had achieved long-term FIX expression in patients that alleviated hemophilia B-related symptoms [10, 19]. Overall, the results from these trials highlight the important role of memory T cells in influencing the treatment efficacy of AAV-based gene therapy.
Overcoming the current hurdles in AAV-based therapy
Capsid engineering to evade pre-existing AAV antibodies
Seroprevalence analyses indicate that some NAbs can cross-react with multiple wtAAV serotypes [67], and thus, switching to other naturally occurring AAV serotypes offers limited benefits for immune evasion. Studies on capsid biology revealed distinctive residues that are responsible for antibody binding [54], suggesting that AAV capsid engineering could potentially be the solution to overcome the immune barriers [68].
There are two main strategies for AAV capsid engineering: rational protein design and directed evolution [54]. Rational protein design relies on the prior knowledge of the capsid amino acid sequences and their functionalities. For example, a monoclonal antibody A20 was identified to bind AAV2 through residue 265 of VP1 protein. By inserting a different amino acid at residue 265, a mutant AAV2.5 was generated with a weaker binding affinity to A20 [69]. Directed evolution uses error-prone PCR or DNA shuffling strategy to construct a library of mutant capsids and perform a rigorous selection to identify desired mutants [54]. For instance, AAV-DJ is a chimera capsid generated from AAV serotypes 2, 8, and 9 through DNA shuffling , which supports gene delivery with higher efficiency than AAV2 into the liver of both naïve and IVIG (intravenous immunoglobulin) treated mice [70]. Another example of engineered immune-evading AAV is the novel variant SCH9 which can efficiently transduce neural stem cells (NSCs) and is ten times more resistant to NAbs than the parental AAV9 [71]. Collectively, the efforts to diversify AAV capsids put forth a hopeful future for creating more efficient vectors.
Besides capsid engineering, alternative approaches have also been explored to overcome the NAb issue. For instance, recent reports showed that plasmapheresis could efficiently remove NAbs to permit AAV re-delivery and transgene expression in rodent models, which can serve as an alternative solution when anti-AAV NAbs cannot be bypassed through other means [72, 73]. Nonetheless, host immune responses to intravenous AAV delivery is far more complex than previously known [67]. Hence, further research is necessary to unlock the full potential of in vivo gene therapy.
Coupling AAV with integrative vectors to support long-term expression
In parallel with the development of AAV, other delivery vectors such as lentivirus, retrovirus, and transposon system are well-established systems and have been adopted for therapeutic applications [74,75,76]. These vectors have relatively large payloads and can integrate into the genome of both dividing and non-dividing cells to support long-term gene expression. In clinics, integrative vectors have been implemented in ex vivo therapies, to engineer immune cells to treat patients with end-stage cancers [77, 78] or to correct deleterious genetic defects in highly proliferative hematopoietic progenitor cells [79, 80]. However, the application of integrative vectors for in vivo gene transfer is limited.
By taking advantage of the highly efficient AAV-mediated gene delivery system, a hybrid AAV/piggyBac vector system was developed and successfully introduced stable transgene transposition into hepatocyte genome [81, 82]. The high efficiency of in vivo gene delivery using the hybrid AAV/piggyBac vector and stable transgene expression was evident in the livers of neonatal mice, which resulted in the correction of the two genes responsible for inherited urea cycle defects [81]. Recently, the AAV/piggyBac hybrid vector has been adopted to treat cystic fibrosis in pigs using aerosolized AAV vectors carrying CFTR flanked by the piggyBac terminal repeats [83]. Despite the small packaging capacity of AAV and semi-random integrations of transposons, the hybrid AAV/piggyBac vector system offers a stable and long-term transgene expression in treated animals through transgene integrations in transduced cells.
Advancement of in vivo gene editing using AAV-delivered nucleases
Breakthrough in genome editing technologies
The newly developed engineered nucleases, such as zinc-finger nucleases (ZFNs) [84], transcription activator-like effector nucleases (TALENs) [85], and type II bacterial clustered regularly interspaced short palindromic repeats (CRISPR)-associated protein 9 (Cas9) system [86], have revolutionized genome editing technologies and opened up a new avenue for the advancement of targeted gene editing therapy. Both ZFNs and TALENs contain a FokI nuclease domain and an assembly of multiple motifs that are programmable to recognize a selected DNA sequence to guide site-specific cleavage. Distinctly, the CRISPR/Cas9 system utilizes a single guide RNA (sgRNA), complexed with Cas9 nuclease, to recognize a variable 20-nucleotide target DNA sequence adjacent to a protospacer adjacent motif (PAM), and cuts the target DNA [87, 88]. The ZFN, TALEN, and CRISPR/Cas9 can all induce DNA double-strand break (DSB) efficiently at a pre-selected target site, which is then repaired via one of the two main mechanisms, the non-homologous end joining (NHEJ) or homology-directed repair (HDR) pathway [89, 90].
The NHEJ repair is error-prone and introduces small insertions or deletions (indels) at the targeted cleavage points [89], thereby abolishing the function of a target gene [91]. Distinctly, the HDR pathway relies on existing homologous DNA sequences to direct DNA repair through a strand-exchange process [90], which supports the replacement of genome segments with donor DNA based on the flanking homology sequences [92]. The site-specific gene targeting by ZFN, TALEN, and CRISPR/Cas9 systems have been widely adopted in research to introduce a wide range of genomic modifications, such as targeted mutation, insertion, and large deletion [93]. The CRISPR/Cas9 system is particularly praised by the scientific community for its superior simplicity, ease for reprogramming, and robust performance, which has garnered more popularity than other nuclease tools [94, 95].
Therapeutic potential of using AAV-delivered nucleases for in vivo gene editing
The highly customizable and robust gene editing nucleases present appealing opportunities to develop novel therapeutics. As a proof-of-concept, the AAV-delivered ZFN system was first employed to introduce somatic gene editing in mice for disease corrections [96]. Several studies conducted by K. High et al. have provided concrete evidence demonstrating that somatic gene targeting was able to achieve transgene integration, long-term expression, as well as restoration of hemostasis in mice with hereditary hemophilia [96,97,98].
Subsequently, AAV-delivered CRISPR/Cas9 was extensively employed for in vivo gene editing. To ensure the efficient delivery of CRISPR/Cas9 system, small promoters such as mouse Mecp2 promoter (235 bp), miniCMV promoter (180 bp), and hybrid EF1α/HTLV (nEF) promoter (493 bp) have been used to express the widely used Streptococcus pyogenes Cas9 (SpCas9, ~ 4.2 kb) in one AAV vector, and the sgRNA expression cassette(s) is delivered by another AAV vector [99,100,101]. The discoveries of smaller Cas9 proteins from Staphylococcus aureus (SaCas9, ~ 3.3 kb) and Streptococcus thermophiles (St1Cas9, 3.5 kb) enable the packaging of sgRNA and Cas9 in a single AAV vector [102, 103]. Additionally, successful delivery of the intein-split SpCas9 was reported using a dual-AAV vector system [104]. The subsequent analyses in mouse models showed that the cleavage repaired by NHEJ at a single target site introduced indels up to 40–70% of the total alleles [100, 102], while simultaneous cleavages using two sgRNAs induced deletion of pathogenic mutations [105, 106]. Through HDR-mediated DNA replacement, a therapeutic transgene can be inserted at a pre-selected genomic site in the somatic tissues of a living organism, which can potentially be used for correcting inherited diseases [107,108,109].
The expanding CRISPR toolbox prompts the development of novel strategies for gene therapy
Since the advent of engineered nucleases, researchers have been continuously developing new genome editing strategies. In 2014, Auer et al. exploited the NHEJ mechanism to capture large DNA at Cas9-induced DSB sites and established a distinct homology-independent knock-in approach [110]. In 2016, He et al. compared the NHEJ- and HDR-mediated knock-in side-by-side in various human cell types using a promoterless GFP reporter system and found that the homology-independent knock-in via NHEJ repair mechanism showed superior efficiency compared to HDR methods [111, 112]. This is consistent with the understanding that HDR is associated with DNA replication, while the NHEJ mechanism adopts a more flexible process that is largely active throughout the cell cycle [113]. In the same year, Suzuki et al. applied the homology-independent knock-in approach through AAV-mediated delivery to achieve targeted integration in mouse liver [101].
Continuous discoveries and protein engineering are rapidly expanding the CRISPR toolbox [114, 115]. Efforts in searching for new Cas9 orthologues identified a number of smaller Cas9 proteins, such as SaCas9 and St1Cas9 [102, 103], as well as Cas orthologues with higher fidelity such as Cpf1 (Cas12a) [116]. Research on rational engineering gave rise to new Cas9 variants and orthologues with greater specificity [117,118,119]. Investigations using protein fusion strategy developed novel gene editing tools. For instance, fusing catalytically inactivated Cas9 (dCas9) with a transcriptional activator (VP64, p65AD, SunTag, or VPR) or repressor (KRAB) generated synthetic transcription factors [120,121,122,123]. The coupling of dCas9 or mutant Cas9 (D10A) to a cytidine deaminase, such as APOBEC1 and AID, produced the base editor (BE) that can catalyze single base pair substitutions within targeted sequences [124, 125]. Collectively, the adaptation of CRISPR technology coupled with gene editing strategies unveils great potentials and prompts the development of novel gene therapy strategies [126].
Broadening the prospects of AAV-delivered therapeutics through somatic gene editing
Undoubtedly, the advancement of in vivo gene targeting using AAV-mediated delivery of ZFN or CRISPR has propelled intensive research to develop gene editing therapies for treating deleterious inherited diseases that were previously untreatable. In the following sections, we will summarize the recent progress of AAV-based somatic gene editing used in preclinical and clinical studies (Tables 3 and 4), and discuss the inherent challenges from these in vivo studies.
Correcting genetic mutations by HDR-mediated sequence replacement
AAV-CRISPR-mediated DNA replacement via the HDR mechanism has the potential to correct pathogenic mutations in somatic genome. The correction will then remain stable in the genome even in dividing cells, making the genetic correction strategy a suitable treatment option for neonates. Yang et al. carried out a proof-of-concept study by infusing AAV vectors carrying SaCas9, sgRNA, and HDR donor template into neonatal spf-ash mice, which carries the R129H mutation in Otc gene and exhibited a partial deficiency in the urea cycle enzyme ornithine transcarbamylase (OTC) [108]. The study demonstrated the correction of the mutant Otc gene in 10% of the total hepatocytes, as well as increased survival of mice challenged with a high-protein diet [108]. Using a similar approach but targeting human hepatocytes in mouse models with human hepatocyte engraftment, Ginn et al. achieved targeted correction among 29% of human OTC alleles in the patient-derived primary hepatocytes [127]. Similarly, Zhou et al. performed subcutaneous injection to deliver AAV vectors carrying SpCas9, sgRNA, and donor into neonatal LdlrE208X mice that harbors a nonsense mutation E208X in the Ldlr gene to mimic familial hypercholesterolemia (FH). The treatment significantly ameliorated atherosclerosis in mice fed with a high-fat diet [128]. In another study, newborn Pahenu2 mice, a disease model for phenylketonuria (PKU), intravenous delivery of AAV vectors carrying SpCas9, sgRNA, and donor DNA yielded significant correction of the mutations as well as reduction of serum phenylalanine levels [129].
Other than providing a donor template for HDR-based mutation correction, Wang et al. reported that inducing cuts simultaneously at two alleles of a gene could also trigger inter-homolog translocation and allelic exchange, thereby correcting recessive compound heterozygous mutations through the HDR mechanism. By introducing genome cuts into newborn mice, their study showed allelic exchange and disease rescue in Fahneo/PM and Iduaneo/W392X mice to mimic the disease conditions for hereditary tyrosinemia type I (HT1) and mucopolysaccharidosis type I (MPS I), respectively [130].
Targeted insertion of therapeutic sequences in somatic genome
Given the huge diversity of loss-of-function mutations that may occur within a single disease-related gene, targeted DNA insertion at a defined locus is a more direct strategy to restore gene function. Inherited hemophilia B has been used as a study model for testing various targeted integration strategies for gene therapy. Li et al. and Anguela et al. used HDR-based replacement strategy to introduce targeted insertion of hF9 gene exon (hF9 Ex2-8) at a mutant hF9 transgene locus in mouse liver using AAV-delivered ZFN and reported successful production of functional hFIX as well as the reversal of blood coagulation defect in hemophilia B mice [96, 97]. By using the AAV-delivered SaCas9, Ohmori et al. inserted the normal mF9 gene Ex2-8 [107], and Wang et al. knocked-in the Ex2-8 of the hyperactive hF9 variant (hFIXco-Padua), at the mutant mF9 locus [109]. Both studies achieved successful gene targeting, stable production of circulating FIX, and significant improvement of hemophilia B-related symptoms [107, 109].
Much effort was also focused on surveying general target sites that can potentially be used for different therapeutic targeting. Through AAV-ZFN-mediated HDR-replacement, Sharma et al. showed that targeted insertion at intron 1 of Albumin locus (mAlb In1) could achieve long-term expression of human FVIII and FIX at therapeutic levels [98]. By targeting the same site, the group also successfully produced lysosomal enzymes encoded by GAL, GBA, IDUA, and IDS, which are responsible for Fabry and Gaucher diseases as well as Hurler and Hunter syndromes [98]. Likewise, De Caneva et al. successfully rescued neonatal lethality in mice with Crigler-Najjar syndrome by inserting hUGT1A1 at mAlb Ex14 through AAV- and SaCas9-mediated HDR [131]. Together, these studies suggest that the ALB locus could be a potential universal target locus for targeted insertion to express liver secretory proteins.
Homology-independent knock-in mediated by the NHEJ mechanism does not require homology sequences, which makes AAV delivery much easier. By using SpCas9, Suzuki et al. demonstrated the potential of AAV-delivered homology-independent targeted insertion (also named HITI) to restore Merk gene expression and function in the rat retina, which successfully ameliorated visual impairment associated with retinitis pigmentosa [101]. Using AAV-delivered SaCas9, Chen et al. and Zhang et al. reported NHEJ-mediated insertion of BDD-FVIII at mAlb In13 [132] and multiple sites within mAlb In11-13, respectively, which restored FVIII production and hemostasis in mice with hemophilia A [133].
In contrast to AAV-based gene augmentation therapy, gene editing therapy via targeted integration could utilize promoterless donors. Thus, the therapeutic sequences will only be expressed upon correct insertion. Moreover, a well-characterized targeting site can be established to support the insertion and expression of various therapeutic genes in a tissue-specific manner. These new features could further reduce the risks of unwanted gene activation or uncontrolled expression.
Gene (allele) disruption via site-specific targeting followed by NHEJ repair
The versatile AAV-delivered nucleases can also generate frameshift mutations via NHEJ repair in a target gene in the somatic genome to disable the translation of defective proteins. By targeting a cholesterol regulatory gene Pcsk9 in mouse liver using AAV8 encoding SaCas9, Ran et al. introduced indels at around 40% of the target alleles, which significantly reduced serum PCSK9 and total cholesterol levels [102]. Likewise, intravitreal delivery of AAVs carrying CjCas9 [134] and LbCpf1 [135] successfully disrupted angiogenesis-associated genes Vegfa and Hif1a in the mouse retina, which substantially decreased the excessive choroidal neovascularization in a transgenic model for age-related macular degeneration (AMD) [134, 135]. More recently, Chung et al. also demonstrated the therapeutic potentials of AAV-delivered SaCas9 and SpCas9 to treat AMD [136]. Markedly, the AAV-CRISPR-mediated in vivo gene disruption also resolved the gain-of-function mutations in the photoreceptor guanylate cyclase (GUCY2D) gene that causes dominant cone-rod dystrophy (CORD6) in nonhuman primate (NHP) [137].
A sgRNA can also be programmed for allele-specific disruption. In an effort to correct autosomal dominant inherited diseases, Xie et al. disrupted the mutant allele encoding PRKAG2H530R using AAV-delivered SpCas9 while sparing the wild-type allele intact, resulting in successful correction of PRKAG2H530R-induced cardiac syndrome in the transgenic mouse model [138]. Similarly, Giannelli et al. corrected Retinitis Pigmentosa caused by the dominant RhoP23H mutation in mice [139]; and Gyorgy et al. prevented deafness in mice carrying the Beethoven mutation (TMC1T1253A) that causes degeneration of cochlear hair cells and progressive hearing loss [140].
Gene editing using AAV-delivered CRISPR/Cas9 has also been explored as antiviral therapeutics and tested for treating chronic viral infections, such as human immunodeficiency virus (HIV). Intravenous injection of AAV vectors carrying multiplexed sgRNAs and SaCas9 was shown to induce proviral excision, and subsequently decrease viral gene expression in the HIV-1 Tg26 transgenic mice and humanized mice with chronic HIV-1 infection [141]. More recently, the combined application of sequential long-acting slow-effective release antiviral therapy (LASER ART) and CRISPR/Cas9 showed great potential in complete eradication of HIV in HIV-1-infected humanized mice [142].
Restoring gene function through dual-sgRNA-directed deletion
AAV-mediated delivery of Cas9 with dual sgRNAs targeting both sides of a sequence could induce targeted deletion via NHEJ repair and has been exploited to eliminate deleterious mutations, such as cryptic splice sites that cause severe splicing errors. Leber congenital amaurosis-10 (LCA10) is an inherited retinal dystrophy that is often attributed to IVS26 mutation in the CEP290 gene which creates a de novo splice donor site and produces transcripts with a premature stop codon [158]. Using AAV5-delivered SpCas9 and carefully selected dual sgRNAs, Ruan et al. excised the IVS26 mutation in mouse photoreceptor cells, which restored the splicing and function of CEP290 and rescued vision loss [143]. Later on, Maeder et al. developed a gene editing therapy based on subretinal delivery of SaCas9 and two sgRNAs in a single AAV5 vector, named EDIT-101, and demonstrated successful excision of the IVS26 containing region and substantial restoration of the CEP290 function in humanized CEP290 mice [157]. Subsequently, a surrogate vector also achieved successful editing of the CEP290 gene and demonstrated therapeutic benefits in NHP [157]. With these efforts, Allergan and Editas Medicine launched their landmark phase 1/2 clinical trial for EDIT-101 and commenced dosing in the first LCA10 patient in March 2020, which sets the record to be the first in vivo CRISPR medicine administered to patients with FDA approval [159].
A similar therapeutic strategy is also intensively tested for treating Duchenne muscular dystrophy (DMD), the most common form of muscular dystrophy caused by mutations in the DMD gene. Based on the clinical evidence that exon skipping in DMD patients is associated with milder symptoms, research groups first applied the dual-sgRNA strategy to excise exon 23 carrying a nonsense mutation. Studies using mdx mice achieved successful deletion of the mutant Ex23 in both neonatal and adult mice, which yielded shorter yet partially functional dystrophins and significantly improved muscular organizations and functions [99, 105, 106, 144]. Other groups have also used the dual-sgRNA strategy to excise longer genomic regions, such as Dmd Ex21-23 or Ex44-45, to restore muscle function in the mdx mice [145, 146]. Moreover, intramuscular injection of AAV9 carrying intein-split SpCas9 to excise DMD Ex51-52 in DMD pigs also improved their skeletal muscle function [147]. Interestingly, Dwi et al. excised Lama2 Ex2 to eliminate an aberrant splicing donor site causing congenital muscular dystrophy type 1A (MDC1A), which partially restored muscle function in the dy2J/dy2J mouse model [148].
Base editing approach for gene correction and knockout
Base editing is a novel DNA-engineering approach which enables programmable base-substitutions in the genome for correcting pathogenic point mutations. Base editors (BEs) are generated by fusing mutant Cas9 with a cytidine or adenine deaminase [124, 125]. Despite the large sizes of the BEs, in vivo delivery was achieved using dual AAV vector systems [104]. By using the intein-split approach, Ryu et al. demonstrated the therapeutic potential of adenine base editors (ABEs) in correcting a nonsense mutation in the Dmd gene [149]. Yang et al. applied AAV-delivered cytidine base editor (CBE) to restore the start codon of the mutated Fah gene, which yielded functional expression in mouse liver and ameliorated the HT1 symptoms [150]. More recently, Levy et al. reported in vivo base editing at therapeutically relevant efficiencies in a broad range of mouse tissues, including brain (up to 59%), liver (38%), retina (38%), heart (20%), and skeletal muscle (9%) [160]. Through trans-splice strategy, Villiger et al. corrected the Pahenu2 c.835 T > C mutation through intravenous injection of AAVs carrying split CBE, which subsequently restored PAH enzyme activity and serum phenylalanine levels in Pahenu2 mice [151].
BEs are also used to introduce nonsense mutations to inroduce a loss-of-function effect [161]. CBE delivered via adenovirus vector has been tested to reduce the Pcsk9 and Hpd expressions in the mouse model with inherited hypercholesterolemia [162]. In another study, AAV-mediated intein-split delivery of CBE was implemented to disable the mutant SOD1 allele in SOD1G93A mice, which markedly slowed down the progression of amyotrophic lateral sclerosis (ALS) disease and prolonged survival [152].
Feasibility of gene editing therapy in neonate and fetus
In vivo genome editing has presented a promising potential for early gene intervention in neonates or fetuses to treat previously untreatable diseases. Intraperitoneal (i.p.) injection is the most frequently used route of administration and supports the delivery of CRISPR/Cas9 reagents into murine pups at postnatal day 1–4 to correct the congenital or Duchene muscular dystrophy [99, 106, 148]. Intravenous injection (i.v.) via facial or temporal veins is also widely used in neonatal pups and achieved gene editing in the liver to correct metabolic disorders, such as hyperammonemia [108], PKU [129], and hypercholesterolemia [128] which are caused by genetic defects in the Otc, Pah, and Ldrl genes, respectively. Local injections into the muscles or in the cochlear of neonatal pups have also tested and achieved successful somatic gene editing to correct DMD and hearing loss, respectively [99, 140]. The possibility to perform therapeutic gene editing before birth was also examined, wherein in utero editing of Pcsk9 and Hpd genes confirmed the long-term persistence of edited cells in postnatal mice [162]. Collectively, these studies support the feasibility of using gene editing intervention in fetuses and neonates to correct defective genes before disease onset, which is critical for treating diseases with high morbidity and mortality.
Combined delivery of AAV-donor and non-viral CRISPR/Cas9 for ex vivo gene editing therapy
In earlier studies, the AAV vector was rarely used for transducing hematopoietic stem and progenitor cells (HSPC) because the rapid cell proliferation in the subsequent differentiation processes will quickly dilute the vectors and abolish transgene expression. Soon after the advent of engineered nucleases, studies found that AAV6 transduces HSPC with high efficiency and provides single-stranded DNA as donor template, which enables superior HDR-based gene editing when co-delivered with ZFN mRNA or Cas9/sgRNA ribonucleoprotein (RNP) [163,164,165]. As a result, there has been rapid development of ex vivo gene editing therapeutics for treating HSPC-based inherited diseases (Table 5).
Ex vivo gene editing in HSPCs provides an ideal strategy for treating inherited hemoglobinopathies and immunodeficiencies, such as sickle cell disease (SCD), β-thalassemia, and X-linked severe combined immunodeficiency (SCID-X1). Earlier studies used ZFN mRNA and integrative deficient lentivirus vector (IDLV) to demonstrate the HDR-based targeted insertion of a corrective cDNA into the IL2RG locus of the HSPCs isolated from SCID-X1 patient [166]. Using Cas9/sgRNA RNP and oligonucleotide donors, Dewitt et al. corrected the sickle cell anemia mutation HBBE6V in the HSPCs isolated from SCD patients [167]. More strikingly, the co-administration of AAV6 donor and Cas9/sgRNA RNP for HDR-based gene editing in HSPCs derived from SCD patients achieved significantly higher rates for the correction of sickle mutation E6V and targeted insertion. The edited HSPCs were then transplanted into immunodeficient mice and restored normal β-globin expression in vivo [163]. Additionally, Pavel-Dinu et al. reported the correction of X-SCID and long-term engraftment of the edited HSPCs, which provided substantial preclinical evidence supporting the therapeutic potential of using ex vivo editing for X-SCID [168].
Studies also transduced HSPC with Cas9/sgRNA RNP alone to introduce NHEJ-based gene disruption, and applied this strategy to abolish the repression of γ-globin genes HBG1/2 in HSPCs ex vivo for the treatment of SCD and β-thalassemia. The results showed that disruption of the repressor binding motif in the HBG1/2 loci or the β-globin gene HBB locus could re-activate γ-globin expression to ameliorate disease symptoms [171,172,173,174]. Markedly, the CRISPR-disruption of BCL11A enhancer developed by CRISPR Therapeutics and sponsored by Vertex Pharmaceuticals, named CTX001, has been approved as the first human CRISPR trial for SCD (NCT03745287) and transfusion-dependent β-thalassemia (NCT03655678).
The HSPC-based ex vivo gene editing has also provided an appealing treatment strategy for HIV infection. HIV attacks human T cells through binding to the CCR5 receptor [179]. Hence, ex vivo targeting of the CCR5 gene in HSPCs followed by autologous transplantation could potentially provide treatment by preventing HIV entry into the edited HSPCs [164, 175]. Studies using various gene delivery methods have yielded consistent results, showing that the CCR5-ablated human HSPCs indeed conferred HIV-1 resistance in mouse models [175,176,177]. These promising preclinical outcomes are currently being tested in several clinical trials [178].
Besides HSPCs, ex vivo gene editing also presents enormous potentials to engineer immune cells, especially the revolutionary immunotherapy using chimeric antigen receptor (CAR) T cells (CAR-T). Targeted insertion of anti-CD19 CAR at TRAC locus through co-administration of AAV6 donor and Cas9/sgRNA RNP demonstrated a stable CAR expression and improved effectiveness in the CAR-modified T cells [169]. Moreover, the TRAC gene disruption enables allogeneic transplantation, which permits the generation of “universal” CAR-T cells from healthy donors and supports the manufacturing of off-the-shelf CAR-T products [169]. Dai et al. used a similar strategy to insert the CAR at different immune-modulating gene loci, such as B2M, CD52, HLA-1, and generated CAR-T cells with immune-checkpoint knockout (KIKO CAR-T cell) [170]. Compared to lentivirus transduction, the targeted CAR insertion via AAV6-Cas9 RNP co-delivery significantly reduced random integrations as well as chances of undesired side effects in the CAR-T cells. As a result, the new CAR-T cells generated through AAV6-Cas9 RNP using multiplex gene editing by CAR insertion and disruption of TRAC or other immune-modulating genes are widely explored for treating various cancers [180].
Challenges for developing AAV-CRISPR therapy for clinical application
Accumulating preclinical studies and ongoing clinical trials using the AAV delivery system have unveiled new challenges for the development of AAV-CRISPR-based gene editing for clinical application.
Integration of AAV vectors at DSB sites of the genome
The AAV vector genomes mainly persist in transduced cells as episomes, while sporadic integrations through DNA DSB capture have been observed [181]. The likelihood for AAV integration to occur is around 0.05% in neonatal mice and between 10E−4 and 10E−5 in the liver and muscle of nonhuman primates and humans [182, 183]. The integration of AAV vector sequences poses risks of insertional mutagenesis, but the tumorigenic potentials in clinical applications remain controversial. Studies in mice have reported an increased incidence of hepatocellular carcinoma (HCC) that was attributed to random AAV integration that inadvertently activated the transcription of oncogenes [184, 185]. On the contrary, other studies provided evidence supporting that the non-integrative nature of AAV does not pose an increased risk for cancer development. Bell et al. conducted a thorough histology analysis of 695 mouse subjects [186] and Li et al. reported an 18-month follow-up of the mouse subjects [187], after AAV-based gene treatment. Both studies reported no correlation between tumorigenesis and AAV-based gene delivery. Similar investigations were conducted in dogs, NHPs, and human patients, which also showed no associated risk for AAV vector-induced malignancy [188, 189]. Furthermore, several studies also examined the correlation between wtAAV integrations and the occurrence of human hepatocellular carcinoma using clinical samples, which reported contradictory findings and remained inconclusive [190, 191].
Another potential issue related to gene editing therapy using AAV vectors is whether CRISPR and other nucleases will increase the incidence of integration events. A recent study by Nelson et al. showed that, while AAV-CRISPR genome editing in mdx mice exhibited sustained restoration of dystrophin function, unintended genome alterations such as the AAV integrations at sgRNA target sites were detected without apparent consequences on the mice [144]. Similarly, through genome-wide mapping of the mouse brain DNA after stereotactic injection of AAV vectors, a high level of AAV integration with strong preference at the target sites was observed [192]. In both studies, the low levels of random AAV integrations were detected throughout the genome, which was not associated with the CRISPR editing and did not pose a risk higher than that introduced by wtAAVs in humans [144, 192]. Collectively, further investigation should be directed to improve targeting strategies to minimize integration-induced mutagenesis, while the consequences of the high-level AAV integration at specific target sites may need to be evaluated on a case-by-case basis.
Off-target effects in genome editing with CRISPR systems
The sgRNA in CRISPR system can tolerate minor mismatches to guide DNA cleavage at an off-target site [193]. Clinically, the CRISPR/Cas mismatch tolerance raises safety concerns and prompts research groups to explore ways to improve targeting specificity [194]. New algorithms are continuously generated to facilitate the selection of sgRNA with high gene editing activity and fidelity [195, 196]. Additionally, new Cas9 orthologues and engineered Cas9 variants, such as the enhanced specificity SpCas9 (eSpCas9), high fidelity SpCas9 (SpCas9-HF1) [117, 118], and the high fidelity SaCas9 (SaCas9-HF) [119], have achieved greater targeting specificity without sacrificing gene editing activity [114, 115]. Moreover, the shortened expression of Cas9 through lipid nanoparticle delivery of mRNA has greatly reduced off-target editing [197].
Extensive efforts have been made to map out off-target events at the genome level, which were later found to be challenging with the technologies that are currently available. Performing whole-genome sequencing (WGS) for edited cells is prohibitively expensive for identifying rare but potentially deleterious off-target events [198]. Gene analysis by targeted deep sequencing is limited by the sequence homology assumptions inherent in the computational prediction of potential off-target sites. To address these challenges, multiple new analysis platforms have been developed to detect Cas9 off-target events throughout the genome [194]. These include DISCOVER-Seq [199], GUIDE-seq [200], BLESS [201], CIRCLE-seq [202], and SITE-seq [203]. However, each of these platforms can only identify a portion of off-target events, and none of which can deliver a comprehensive characterization of off-target modifications to evaluate the overall functional impact. In future, multiple analysis technologies may be used together for identifying off-target events and safety assessment of a newly developed gene editing therapy.
Risk of horizontal and vertical transmission
In clinical studies, human subjects who received systemic administration of AAV vectors were found to carry AAV particles in bodily fluids, such as serum and urine, for several weeks [8, 204]. Since AAV vectors are replication-defective, the risk for horizontal transmission is low and mainly restricted during vector transfer. However, the persistence of AAV particles with broad tissue tropisms in bodily fluids [205] makes it difficult to target specific tissues or organs without diffusing into other tissues in the human body. Consequently, AAV treatments could result in gene expression or genome editing in non-targeted tissues and potentially give rise to pathological features, which should be evaluated thoroughly.
In AAV-based gene editing therapy, vertical transmission of AAV vectors and germline contamination poses a much more serious concern [206]. Earlier studies detected AAV sequences in human semen samples [207], and a similar observation was reported in the murine testis as confirmed by the presence of AAV-delivered reporter expression [208]. Interestingly, although AAV vector sequences were detected in seminal fluids and epithelial cells from genitourinary tracts, they were not found in germ cells and had not passed through germline transmission [209, 210]. Furthermore, after a close investigation, Rajasekaran et al. reported that AAV2 and AAV9 vectors primarily targeted Leydig cells while a modified-AAV2 targeted Sertoli cells of the testis [211]. Notably, none of these vectors transduced sperm progenitor cells [211]. Consistently, in vivo gene targeting studies found no evidence of genome editing in the sperms or offspring derived from the edited mice [144]. Together, these results eliminate the concern regarding the vertical transmission of AAV and whereby induced germline modifications through systemic administration.
Host immune responses to CRISPR and Cas proteins
Host immune responses to CRISPR/Cas9 and its orthologues may present another challenge to the development of gene editing therapy. In a recent analysis of human serums, a large proportion of the human populations was found to carry naturally occurring antibodies to Cas9. Manno et al. reported that 79% of the examined individuals exhibited anti-SaCas9, and 65% had anti-SpCas9 [212]. Wagner et al. reported 96% of the donors in their study showed pre-existing T cell memory responses against SpCas9 [213]. Consequently, the pre-existing antibody could neutralize Cas9 and impair the gene editing efficiency, while pre-existing anti-Cas9 lymphocytes can trigger immune destruction of edited cells due to Cas9 expression [214].
In order to circumvent the host immune responses to CRISPR/Cas system, it is critical to adjust the delivery parameters and strategies, such as lowering the dosage of vectors, optimizing the vector administration route, and shortening the expression of the Cas9 gene. Previously, transient immune suppression made AAV-based gene therapy possible by protecting AAV-transduced cells from the immune responses [10, 21, 215]. Therefore, it is of interest to investigate the potential of using transient immunosuppression to protect Cas9-expressing cells from immune destruction and to sustain the efficacy of gene editing. Additionally, prescreening for the presence and levels of neutralizing antibodies in patients could be implemented to determine the suitability of a treatment regimen as well as to guide the use of AAV vector capsids and Cas9 variants for each individual patient prior to treatment. Furthermore, developing a novel Cas9 variant via protein engineering to overcome the immune barriers is also worth investigating in future.
Expanding horizons for gene therapy
Non-viral delivery of CRISPR
Recent advancements in drug delivery using synthetic nanoparticles (NPs) have made significant progress. In 2018, a siRNA drug packaged in nanoparticles, marketed under the brand name Onpattro (patisiran), was approved by the FDA for the treatment of hereditary amyloidogenic transthyretin (hATTR, also named ATTRv) amyloidosis [216]. Extensive studies have investigated the potentials of utilizing NPs for CRISPR/Cas9 delivery, among which lipids and lipid-like nanomaterials are potentially suitable for intracellular delivery of genome editing cargos under in vivo conditions [217]. Yin et al. packaged Cas9 mRNA in lipid NPs and used in combination with AAV vectors encoding sgRNA and HDR template to induce gene correction in the Fah-/- mice [197]. Lee et al. applied gold nanoparticles conjugated to DNA and complexed with cationic endosomal disruptive polymers (named CRISPR-Gold) to deliver CRISPR RNPs and donor template to correct DMD mutation in Dmx mice [218]. To maximize the delivery efficiency, Jiang et al. further developed lipid-like nanoparticles to carry Cas9 mRNA and sgRNA to the liver and demonstrated effective disruption of endogenous Pcsk9 gene, as well as pre-delivered HBV DNA in mice [219]. In the November 2020, Intellia Therapeutics dosed the first patient with a lipid nanoparticles (LNPs)-carried CRISPR/Cas9-gene editing therapy to treat hATTR, which becomes the first systemically delivered CRISPR-based drug candidate tested in clinical trials (NCT04601051)[220]. Currently, there are still several obstacles associated with the therapeutic application of non-viral delivery for gene editing therapy; these include short half-life in the systemic circulation, non-specific delivery, and low accumulation in target tissues. Despite these limitations, the non-viral delivery methods provide invaluable additions to the gene delivery arsenal.
Recent advances in CRISPR technologies
The research on CRISPR technology and its applications is on the rise, with new tools and strategies being developed and tested continuously. Primer editors (PEs) are a newly developed gene editing tool, which consists of a chimera PE protein generated through fusing mutant Cas9 (H840A) with a reverse transcriptase and a primer editing guide RNA (pegRNA) that carries desired genetic information and recognizes a target sequence via base-pairing. Together, the PE/pegRNA complex can directly write new genetic information into a specified DNA site [221]. Using the prime editing technology, Anzalone et al. achieved targeted insertions, deletions, and all 12 types of point mutations in human cells, including the correction of mutations that cause sickle cell disease and Tay-Sachs disease [221].
Distinctly, the Cas orthologues in the Cas13 family possess unique properties for RNA editing, which enables a novel RNA editing approach for gene therapy [222]. Compared to RNA interference (RNAi) for RNA editing, the RNA targeting by CRISPR/Cas13 triggers targeted degradation of a selected RNA with high specificity [223, 224]. Lipid-based delivery of Cas13a protein and guide RNA has been used for in vivo experiments to target a mutant KRAS transcript and was found to effectively impair tumor proliferation of pancreatic cancer in a xenograft mouse model [225]. In early 2020, CRISPR/Cas13-based RNA targeting, multiplexed with crRNAs targeting conservative sequences of the coronaviruses, has been shown to effectively degrade more than 90% of coronaviruses, including SARS-CoV-2 sequences and live influenza A virus (IAV) in human lung epithelial cells [226].
Finally, guided transcriptional regulators generated by incorporating a repressor or activator domain to the inactivated Cas9 protein, named CRISPR interference (CRISPRi) and CRISPR activation (CRISPRa) respectively, have also been investigated for disease treatment. Thakore et al. used intein-split dual AAV8 vectors to deliver dCas9-KRAB into the mouse liver to target Pcsk9, which successfully repressed Pcsk9 expression and lowered the cholesterol levels in mice with LPL deficiency [153]. Colasante et al. reported that guided transcription activation using AAV-delivered dCas9-VP64 upregulated Scn1a gene expression to attenuate seizures in a Scn1a haploinsufficiency mouse model of Dravet syndrome [154]. Besides the examples mentioned above, additional gene editing strategies and preclinical studies could also be found in recent reviews [28, 227, 228]. Altogether, these new CRISPR tools showed potentials to treat human diseases through distinct strategies, which warrant more investigations to improve delivery efficiency and address safety concerns in the future.
Conclusions
In this review, we have provided an overview of milestones achieved, current trends, and challenges of gene therapy using AAV vectors. Gene therapy is a multidisciplinary field, significant innovations have been made in the areas of gene editing, vector engineering, nanoparticles, and other technology platforms. The clinical application of using AAV vector as a tool for gene delivery already has a long history of success in preclinical and clinical studies. Currently, the AAV vector is the leading platform for in vivo gene therapy delivery. As with other viral vectors, the toxicity associated with high-dose AAV delivery and risk for inadvertent insertional mutagenesis are the major concerns and warrant further investigation in clinical applications. With the advancement of CRISPR/Cas9 genome editing technology, AAV vector carrying the CRISPR components have been an attractive tool, with therapeutic potentials validated in both in vivo and ex vivo gene editing. Given the encouraging results and continuous expansion of the CRISPR toolbox, the AAV-CRISPR approach will expand the repertoire of gene therapy strategies and pave the way to the new era of innovative medicine. Further improvement in the performance of engineered AAV capsids and mass production technology is essential to streamline the development of any type of AAV-based therapeutics to deliver the cures for diseases, while further confirmation of the safety in using CRISPR in vivo is needed to harness the full potential of the AAV-CRISPR system for gene editing therapy.
Data availability
This article reviews literature and therefore does not contain any associated data and materials.
References
Atchison RW, Casto BC, Hammon WM (1965) Adenovirus-Associated Defective Virus Particles. Science 149:754–756
Blacklow NR, Hoggan MD, Rowe WP (1967) Isolation of adenovirus-associated viruses from man. Proc Natl Acad Sci U S A 58:1410–1415
Balakrishnan B, Jayandharan GR (2014) Basic biology of adeno-associated virus (AAV) vectors used in gene therapy. Curr Gene Ther 14:86–100
Samulski RJ, Muzyczka N (2014) AAV-Mediated Gene Therapy for Research and Therapeutic Purposes. Annu Rev Virol 1:427–451
Flotte TR, Afione SA, Conrad C, McGrath SA, Solow R, Oka H et al (1993) Stable in vivo expression of the cystic fibrosis transmembrane conductance regulator with an adeno-associated virus vector. Proc Natl Acad Sci U S A 90:10613–10617
Flotte T, Carter B, Conrad C, Guggino W, Reynolds T, Rosenstein B et al (1996) A phase I study of an adeno-associated virus-CFTR gene vector in adult CF patients with mild lung disease. Hum Gene Ther 7:1145–1159
Kay MA, Manno CS, Ragni MV, Larson PJ, Couto LB, McClelland A et al (2000) Evidence for gene transfer and expression of factor IX in haemophilia B patients treated with an AAV vector. Nat Genet 24:257–261
Manno CS, Pierce GF, Arruda VR, Glader B, Ragni M, Rasko JJ et al (2006) Successful transduction of liver in hemophilia by AAV-Factor IX and limitations imposed by the host immune response. Nat Med 12:342–347
Nathwani AC, Tuddenham EG, Rangarajan S, Rosales C, McIntosh J, Linch DC et al (2011) Adenovirus-associated virus vector-mediated gene transfer in hemophilia B. N Engl J Med 365:2357–2365
Nathwani AC, Reiss UM, Tuddenham EG, Rosales C, Chowdary P, McIntosh J et al (2014) Long-term safety and efficacy of factor IX gene therapy in hemophilia B. N Engl J Med 371:1994–2004
Yla-Herttuala S (2012) Endgame: glybera finally recommended for approval as the first gene therapy drug in the European union. Mol Ther 20:1831–1832
Scott LJ (2015) Alipogene tiparvovec: a review of its use in adults with familial lipoprotein lipase deficiency. Drugs 75:175–182
Maguire AM, Russell S, Wellman JA, Chung DC, Yu ZF, Tillman A et al (2019) Efficacy, Safety, and Durability of Voretigene Neparvovec-rzyl in RPE65 Mutation-Associated Inherited Retinal Dystrophy: Results of Phase 1 and 3 Trials. Ophthalmology 126:1273–1285
FDA (2017) FDA approves novel gene therapy to treat patients with a rare form of inherited vision loss. Press release
Mendell JR, Al-Zaidy S, Shell R, Arnold WD, Rodino-Klapac LR, Prior TW et al (2017) Single-Dose Gene-Replacement Therapy for Spinal Muscular Atrophy. N Engl J Med 377:1713–1722
Al-Zaidy S, Pickard AS, Kotha K, Alfano LN, Lowes L, Paul G et al (2019) Health outcomes in spinal muscular atrophy type 1 following AVXS-101 gene replacement therapy. Pediatr Pulmonol 54:179–185
Urquhart L (2019) FDA new drug approvals in Q2 2019. Nature Reviews Drug Discovery 18:575
Lee JH, Wang JH, Chen J, Li F, Edwards TL, Hewitt AW et al (2019) Gene therapy for visual loss: Opportunities and concerns. Prog Retin Eye Res 68:31–53
Nathwani AC (2019) Gene therapy for hemophilia. Hematology Am Soc Hematol Educ Program 2019:1–8
Miesbach W, Meijer K, Coppens M, Kampmann P, Klamroth R, Schutgens R et al (2018) Gene therapy with adeno-associated virus vector 5-human factor IX in adults with hemophilia B. Blood 131:1022–1031
George LA, Sullivan SK, Giermasz A, Rasko JEJ, Samelson-Jones BJ, Ducore J et al (2017) Hemophilia B Gene Therapy with a High-Specific-Activity Factor IX Variant. N Engl J Med 377:2215–2227
Perrin GQ, Herzog RW, Markusic DM (2019) Update on clinical gene therapy for hemophilia. Blood 133:407–414
Rangarajan S, Walsh L, Lester W, Perry D, Madan B, Laffan M et al (2017) AAV5-Factor VIII Gene Transfer in Severe Hemophilia A. N Engl J Med 377:2519–2530
High KA, George LA, Eyster ME, Sullivan SK, Ragni MV, Croteau SE et al (2018) A Phase 1/2 Trial of Investigational Spk-8011 in Hemophilia a Demonstrates Durable Expression and Prevention of Bleeds. Blood 132:487
Butterfield JSS, Hege KM, Herzog RW, Kaczmarek R (2020) A Molecular Revolution in the Treatment of Hemophilia. Mol Ther 28:997–1015
Pipe S, Leebeek FWG, Ferreira V, Sawyer EK, Pasi J (2019) Clinical Considerations for Capsid Choice in the Development of Liver-Targeted AAV-Based Gene Transfer. Mol Ther Methods Clin Dev 15:170–178
Kattenhorn LM, Tipper CH, Stoica L, Geraghty DS, Wright TL, Clark KR et al (2016) Adeno-Associated Virus Gene Therapy for Liver Disease. Hum Gene Ther 27:947–961
Wang D, Tai PWL, Gao G (2019) Adeno-associated virus vector as a platform for gene therapy delivery. Nat Rev Drug Discov 18:358–378
Foust KD, Nurre E, Montgomery CL, Hernandez A, Chan CM, Kaspar BK (2009) Intravascular AAV9 preferentially targets neonatal neurons and adult astrocytes. Nat Biotechnol 27:59–65
Foust KD, Wang X, McGovern VL, Braun L, Bevan AK, Haidet AM et al (2010) Rescue of the spinal muscular atrophy phenotype in a mouse model by early postnatal delivery of SMN. Nat Biotechnol 28:271–274
Pattali R, Mou Y, Li XJ (2019) AAV9 Vector: a Novel modality in gene therapy for spinal muscular atrophy. Gene Ther 26:287–295
Pearse Y, Iacovino M (2020) A Cure for Sanfilippo Syndrome? A Summary of Current Therapeutic Approaches and their Promise. Med Res Arch 8
Chien YH, Lee NC, Tseng SH, Tai CH, Muramatsu SI, Byrne BJ et al (2017) Efficacy and safety of AAV2 gene therapy in children with aromatic L-amino acid decarboxylase deficiency: an open-label, phase 1/2 trial. Lancet Child Adolesc Health 1:265–273
Deverman BE, Ravina BM, Bankiewicz KS, Paul SM, Sah DWY (2018) Gene therapy for neurological disorders: progress and prospects. Nature Reviews Drug Discovery 17:641–659
(2020) High-dose AAV gene therapy deaths. Nat Biotechnol 38: 910
Wilson JM, Flotte TR (2020) Moving Forward After Two Deaths in a Gene Therapy Trial of Myotubular Myopathy. Hum Gene Ther 31:695–696
Pipe SW, Giermasz A, Castaman G, Key NS, Lattimore S, Leebeek FW et al (2019) AMT-061 (AAV5-Padua hFIX variant) an Enhanced Vector for Gene Transfer in Adults with Severe or Moderate-Severe Hemophilia B: Follow-up up to 9 Months in a Phase 2b trial. Age (years) 43:47
Rosen S, Tiefenbacher S, Robinson M, Huang M, Srimani J, Mackenzie D et al (2020) Activity of transgene-produced B-domain-deleted factor VIII in human plasma following AAV5 gene therapy. Blood 136:2524–2534
Philippidis A (2020) Pfizer and Sangamo Hemophilia A Gene Therapy Aces First Clinical Test. Hum Gene Ther 31:705–708
Mercuri E, Baranello G, Masson R, Boespflug-Tanguy O, Bruno C, Corti S et al (2020) SMA–THERAPY: P. 258 Onasemnogene aveparvovec gene therapy for spinal muscular atrophy type 1 (SMA1): Phase 3 study update (STR1VE-EU). Neuromuscular Disorders 30:S121
Chand D, Finkel R, Mercuri E, Masson R, Parsons J, Kleyn A et al (2020) SMA–THERAPY: P. 256 Intravenous (IV) onasemnogene abeparvovec for spinal muscular atrophy (SMA): integrated safety report. Neuromuscular Disorders 30:S120–S1S1
Farrar M, Swoboda KJ, Schultz M, McMillan H, Parsons J, Alexander IE et al (2019) 014 AVXS-101 gene-replacement therapy (GRT) in presymptomatic spinal muscular atrophy (SMA): study update. Journal of Neurology, Neurosurgery &. Psychiatry 90:A5–A6
Zhang L, Cho JH, Arnaoutova I, Mansfield BC, Chou JY (2019) An evolutionary approach to optimizing glucose-6-phosphatase-alpha enzymatic activity for gene therapy of glycogen storage disease type Ia. J Inherit Metab Dis 42:470–479
Flanigan KM, Smith NJC, Couce ML, Truxal KV, McBride KL, Simmons T et al (2020) Interim results of Transpher A, a multicenter, single-dose, phase 1/2 clinical trial of ABO-102 gene therapy for Sanfilippo syndrome type A (mucopolysaccharidosis type IIIA). Molecular Genetics and Metabolism 129:S56–SS7
Nakai H, Yant SR, Storm TA, Fuess S, Meuse L, Kay MA (2001) Extrachromosomal recombinant adeno-associated virus vector genomes are primarily responsible for stable liver transduction in vivo. J Virol 75:6969–6976
Cunningham SC, Dane AP, Spinoulas A, Alexander IE (2008) Gene Delivery to the Juvenile Mouse Liver Using AAV2/8 Vectors. Mol Ther 16:1081–1088
Harper SQ, Hauser MA, DelloRusso C, Duan D, Crawford RW, Phelps SF et al (2002) Modular flexibility of dystrophin: implications for gene therapy of Duchenne muscular dystrophy. Nat Med 8:253–261
Zhang Y, Duan D (2012) Novel mini-dystrophin gene dual adeno-associated virus vectors restore neuronal nitric oxide synthase expression at the sarcolemma. Hum Gene Ther 23:98–103
Lai Y, Yue Y, Liu M, Ghosh A, Engelhardt JF, Chamberlain JS et al (2005) Efficient in vivo gene expression by trans-splicing adeno-associated viral vectors. Nat Biotechnol 23:1435–1439
Li J, Sun W, Wang B, Xiao X, Liu XQ (2008) Protein trans-splicing as a means for viral vector-mediated in vivo gene therapy. Hum Gene Ther 19:958–964
Tornabene P, Trapani I, Minopoli R, Centrulo M, Lupo M, de Simone S, et al. (2019) Intein-mediated protein trans-splicing expands adeno-associated virus transfer capacity in the retina. Sci Transl Med 11
Weitzman MD, Linden RM (2011) Adeno-associated virus biology. Methods Mol Biol 807:1–23
McCarty DM, Monahan PE, Samulski RJ (2001) Self-complementary recombinant adeno-associated virus (scAAV) vectors promote efficient transduction independently of DNA synthesis. Gene Ther 8:1248–1254
Li C, Samulski RJ (2020) Engineering adeno-associated virus vectors for gene therapy. Nat Rev Genet 21:255–272
Boutin S, Monteilhet V, Veron P, Leborgne C, Benveniste O, Montus MF et al (2010) Prevalence of serum IgG and neutralizing factors against adeno-associated virus (AAV) types 1, 2, 5, 6, 8, and 9 in the healthy population: implications for gene therapy using AAV vectors. Hum Gene Ther 21:704–712
Calcedo R, Wilson JM (2013) Humoral Immune Response to AAV. Front Immunol 4:341
Calcedo R, Vandenberghe LH, Gao G, Lin J, Wilson JM (2009) Worldwide epidemiology of neutralizing antibodies to adeno-associated viruses. J Infect Dis 199:381–390
Calcedo R, Morizono H, Wang L, McCarter R, He J, Jones D et al (2011) Adeno-associated virus antibody profiles in newborns, children, and adolescents. Clin Vaccine Immunol 18:1586–1588
Li C, Narkbunnam N, Samulski RJ, Asokan A, Hu G, Jacobson LJ et al (2012) Neutralizing antibodies against adeno-associated virus examined prospectively in pediatric patients with hemophilia. Gene Ther 19:288–294
Jiang H, Couto LB, Patarroyo-White S, Liu T, Nagy D, Vargas JA et al (2006) Effects of transient immunosuppression on adenoassociated, virus-mediated, liver-directed gene transfer in rhesus macaques and implications for human gene therapy. Blood 108:3321–3328
Scallan CD, Jiang H, Liu T, Patarroyo-White S, Sommer JM, Zhou S et al (2006) Human immunoglobulin inhibits liver transduction by AAV vectors at low AAV2 neutralizing titers in SCID mice. Blood 107:1810–1817
Mingozzi F, High KA (2017) Overcoming the Host Immune Response to Adeno-Associated Virus Gene Delivery Vectors: The Race Between Clearance, Tolerance, Neutralization, and Escape. Annu Rev Virol 4:511–534
Li H, Lin SW, Giles-Davis W, Li Y, Zhou D, Xiang ZQ et al (2009) A preclinical animal model to assess the effect of pre-existing immunity on AAV-mediated gene transfer. Mol Ther 17:1215–1224
Kruzik A, Fetahagic D, Hartlieb B, Dorn S, Koppensteiner H, Horling FM et al (2019) Prevalence of Anti-Adeno-Associated Virus Immune Responses in International Cohorts of Healthy Donors. Mol Ther Methods Clin Dev 14:126–133
Mingozzi F, Maus MV, Hui DJ, Sabatino DE, Murphy SL, Rasko JE et al (2007) CD8(+) T-cell responses to adeno-associated virus capsid in humans. Nat Med 13:419–422
Hui DJ, Edmonson SC, Podsakoff GM, Pien GC, Ivanciu L, Camire RM et al (2015) AAV capsid CD8+ T-cell epitopes are highly conserved across AAV serotypes. Mol Ther Methods Clin Dev 2:15029
Verdera HC, Kuranda K, Mingozzi F (2020) AAV Vector Immunogenicity in Humans: A Long Journey to Successful Gene Transfer. Mol Ther 28:723–746
Buning H, Srivastava A (2019) Capsid Modifications for Targeting and Improving the Efficacy of AAV Vectors. Mol Ther Methods Clin Dev 12:248–265
Li C, Diprimio N, Bowles DE, Hirsch ML, Monahan PE, Asokan A et al (2012) Single amino acid modification of adeno-associated virus capsid changes transduction and humoral immune profiles. J Virol 86:7752–7759
Grimm D, Lee JS, Wang L, Desai T, Akache B, Storm TA et al (2008) In vitro and in vivo gene therapy vector evolution via multispecies interbreeding and retargeting of adeno-associated viruses. J Virol 82:5887–5911
Ojala DS, Sun S, Santiago-Ortiz JL, Shapiro MG, Romero PA, Schaffer DV (2018) In Vivo Selection of a Computationally Designed SCHEMA AAV Library Yields a Novel Variant for Infection of Adult Neural Stem Cells in the SVZ. Mol Ther 26:304–319
Orlowski A, Katz MG, Gubara SM, Fargnoli AS, Fish KM, Weber T (2020) Successful Transduction with AAV Vectors after Selective Depletion of Anti-AAV Antibodies by Immunoadsorption. Mol Ther Methods Clin Dev 16:192–203
Bertin B, Veron P, Leborgne C, Deschamps JY, Moullec S, Fromes Y et al (2020) Capsid-specific removal of circulating antibodies to adeno-associated virus vectors. Sci Rep 10:864
Kotterman MA, Chalberg TW, Schaffer DV (2015) Viral Vectors for Gene Therapy: Translational and Clinical Outlook. Annu Rev Biomed Eng 17:63–89
Kebriaei P, Izsvak Z, Narayanavari SA, Singh H, Ivics Z (2017) Gene Therapy with the Sleeping Beauty Transposon System. Trends Genet 33:852–870
Yant SR, Meuse L, Chiu W, Ivics Z, Izsvak Z, Kay MA (2000) Somatic integration and long-term transgene expression in normal and haemophilic mice using a DNA transposon system. Nat Genet 25:35–41
Wilkins O, Keeler AM, Flotte TR (2017) CAR T-Cell Therapy: Progress and Prospects. Hum Gene Ther Methods 28:61–66
Kebriaei P, Singh H, Huls MH, Figliola MJ, Bassett R, Olivares S et al (2016) Phase I trials using Sleeping Beauty to generate CD19-specific CAR T cells. J Clin Invest 126:3363–3376
Marktel S, Scaramuzza S, Cicalese MP, Giglio F, Galimberti S, Lidonnici MR et al (2019) Intrabone hematopoietic stem cell gene therapy for adult and pediatric patients affected by transfusion-dependent ss-thalassemia. Nat Med 25:234–241
Aiuti A, Biasco L, Scaramuzza S, Ferrua F, Cicalese MP, Baricordi C et al (2013) Lentiviral hematopoietic stem cell gene therapy in patients with Wiskott-Aldrich syndrome. Science 341:1233151
Cunningham SC, Siew SM, Hallwirth CV, Bolitho C, Sasaki N, Garg G et al (2015) Modeling correction of severe urea cycle defects in the growing murine liver using a hybrid recombinant adeno-associated virus/piggyBac transposase gene delivery system. Hepatology 62:417–428
Siew SM, Cunningham SC, Zhu E, Tay SS, Venuti E, Bolitho C et al (2019) Prevention of Cholestatic Liver Disease and Reduced Tumorigenicity in a Murine Model of PFIC Type 3 Using Hybrid AAV-piggyBac Gene Therapy. Hepatology 70:2047–2061
Cooney AL, Thornell IM, Singh BK, Shah VS, Stoltz DA, McCray PB Jr et al (2019) A Novel AAV-mediated Gene Delivery System Corrects CFTR Function in Pigs. Am J Respir Cell Mol Biol 61:747–754
Maeder ML, Thibodeau-Beganny S, Osiak A, Wright DA, Anthony RM, Eichtinger M et al (2008) Rapid "open-source" engineering of customized zinc-finger nucleases for highly efficient gene modification. Mol Cell 31:294–301
Reyon D, Tsai SQ, Khayter C, Foden JA, Sander JD, Joung JK (2012) FLASH assembly of TALENs for high-throughput genome editing. Nat Biotech 30:460–465
Bhaya D, Davison M, Barrangou R (2011) CRISPR-Cas systems in bacteria and archaea: versatile small RNAs for adaptive defense and regulation. Annu Rev Genet 45:273–297
Jinek M, Chylinski K, Fonfara I, Hauer M, Doudna JA, Charpentier E (2012) A programmable dual-RNA-guided DNA endonuclease in adaptive bacterial immunity. Science 337:816–821
Mali P, Yang L, Esvelt KM, Aach J, Guell M, DiCarlo JE et al (2013) RNA-guided human genome engineering via Cas9. Science 339:823–826
Lieber MR (2010) The mechanism of double-strand DNA break repair by the nonhomologous DNA end-joining pathway. Annu Rev Biochem 79:181–211
Heyer WD, Ehmsen KT, Liu J (2010) Regulation of homologous recombination in eukaryotes. Annu Rev Genet 44:113–139
Wang H, Yang H, Shivalila CS, Dawlaty MM, Cheng AW, Zhang F et al (2013) One-step generation of mice carrying mutations in multiple genes by CRISPR/Cas-mediated genome engineering. Cell 153:910–918
Yang H, Wang H, Shivalila CS, Cheng AW, Shi L, Jaenisch R (2013) One-Step Generation of Mice Carrying Reporter and Conditional Alleles by CRISPR/Cas-Mediated Genome Engineering. Cell 154:1370–1379
Cox DB, Platt RJ, Zhang F (2015) Therapeutic genome editing: prospects and challenges. Nat Med 21:121–131
Doudna JA, Charpentier E (2014) Genome editing. The new frontier of genome engineering with CRISPR-Cas9. Science 346:1258096
Hsu PD, Lander ES, Zhang F (2014) Development and applications of CRISPR-Cas9 for genome engineering. Cell 157:1262–1278
Li H, Haurigot V, Doyon Y, Li T, Wong SY, Bhagwat AS et al (2011) In vivo genome editing restores haemostasis in a mouse model of haemophilia. Nature 475:217–221
Anguela XM, Sharma R, Doyon Y, Miller JC, Li H, Haurigot V et al (2013) Robust ZFN-mediated genome editing in adult hemophilic mice. Blood 122:3283–3287
Sharma R, Anguela XM, Doyon Y, Wechsler T, DeKelver RC, Sproul S et al (2015) In vivo genome editing of the albumin locus as a platform for protein replacement therapy. Blood 126:1777–1784
Long C, Amoasii L, Mireault AA, McAnally JR, Li H, Sanchez-Ortiz E et al (2016) Postnatal genome editing partially restores dystrophin expression in a mouse model of muscular dystrophy. Science 351:400–403
Swiech L, Heidenreich M, Banerjee A, Habib N, Li Y, Trombetta J et al (2015) In vivo interrogation of gene function in the mammalian brain using CRISPR-Cas9. Nat Biotechnol 33:102–106
Suzuki K, Tsunekawa Y, Hernandez-Benitez R, Wu J, Zhu J, Kim EJ et al (2016) In vivo genome editing via CRISPR/Cas9 mediated homology-independent targeted integration. Nature 540:144–149
Ran FA, Cong L, Yan WX, Scott DA, Gootenberg JS, Kriz AJ et al (2015) In vivo genome editing using Staphylococcus aureus Cas9. Nature 520:186–191
Agudelo D, Carter S, Velimirovic M, Duringer A, Rivest JF, Levesque S et al (2020) Versatile and robust genome editing with Streptococcus thermophilus CRISPR1-Cas9. Genome Res 30:107–117
Chew WL, Tabebordbar M, Cheng JK, Mali P, Wu EY, Ng AH et al (2016) A multifunctional AAV-CRISPR-Cas9 and its host response. Nat Methods 13:868–874
Tabebordbar M, Zhu K, Cheng JKW, Chew WL, Widrick JJ, Yan WX et al (2016) In vivo gene editing in dystrophic mouse muscle and muscle stem cells. Science 351:407–411
Nelson CE, Hakim CH, Ousterout DG, Thakore PI, Moreb EA, Castellanos Rivera RM et al (2016) In vivo genome editing improves muscle function in a mouse model of Duchenne muscular dystrophy. Science 351:403–407
Ohmori T, Nagao Y, Mizukami H, Sakata A, Muramatsu SI, Ozawa K et al (2017) CRISPR/Cas9-mediated genome editing via postnatal administration of AAV vector cures haemophilia B mice. Sci Rep 7:4159
Yang Y, Wang L, Bell P, McMenamin D, He Z, White J et al (2016) A dual AAV system enables the Cas9-mediated correction of a metabolic liver disease in newborn mice. Nat Biotechnol 34:334–338
Wang L, Yang Y, Breton CA, White J, Zhang J, Che Y et al (2019) CRISPR/Cas9-mediated in vivo gene targeting corrects hemostasis in newborn and adult factor IX-knockout mice. Blood 133:2745–2752
Auer TO, Duroure K, De Cian A, Concordet JP, Del Bene F (2014) Highly efficient CRISPR/Cas9-mediated knock-in in zebrafish by homology-independent DNA repair. Genome Res 24:142–153
He X, Tan C, Wang F, Wang Y, Zhou R, Cui D, et al. (2016) Knock-in of large reporter genes in human cells via CRISPR / Cas9-induced homology-dependent and independent DNA repair. Nucleic Acids Research: 1-14
Zhang C, He X, Kwok YK, Wang F, Xue J, Zhao H et al (2018) Homology-independent multiallelic disruption via CRISPR/Cas9-based knock-in yields distinct functional outcomes in human cells. BMC Biol 16:151
Yang D, Scavuzzo MA, Chmielowiec J, Sharp R, Bajic A, Borowiak M (2016) Enrichment of G2/M cell cycle phase in human pluripotent stem cells enhances HDR-mediated gene repair with customizable endonucleases. Sci Rep 6:21264
Wang J, Zhang C, Feng B (2020) The rapidly advancing Class 2 CRISPR-Cas technologies: A customizable toolbox for molecular manipulations. J Cell Mol Med
Pickar-Oliver A, Gersbach CA (2019) The next generation of CRISPR–Cas technologies and applications. Nature Reviews Molecular Cell Biology 20:490–507
Zetsche B, Gootenberg Jonathan S, Abudayyeh Omar O, Slaymaker Ian M, Makarova Kira S, Essletzbichler P et al (2015) Cpf1 Is a Single RNA-Guided Endonuclease of a Class 2 CRISPR-Cas System. Cell 163:759–771
Kleinstiver BP, Pattanayak V, Prew MS, Tsai SQ, Nguyen NT, Zheng Z, et al. (2016) High-fidelity CRISPR-Cas9 nucleases with no detectable genome-wide off-target effects. Nature
Slaymaker IM, Gao L, Zetsche B, Scott DA, Yan WX, Zhang F (2016) Rationally engineered Cas9 nucleases with improved specificity. Science 351:84–88
Tan Y, Chu AHY, Bao S, Hoang DA, Kebede FT, Xiong W et al (2019) Rationally engineered Staphylococcus aureus Cas9 nucleases with high genome-wide specificity. Proc Natl Acad Sci U S A 116:20969–20976
Hu J, Lei Y, Wong WK, Liu S, Lee KC, He X et al (2014) Direct activation of human and mouse Oct4 genes using engineered TALE and Cas9 transcription factors. Nucleic Acids Res 42:4375–4390
Thakore PI, Ippolito AMD, Song L, Safi A, Shivakumar NK, Kabadi AM, et al. (2015) Highly specific epigenome editing by CRISPR-Cas9 repressors for silencing of distal regulatory elements. Nature Methods 12
Gilbert LA, Horlbeck MA, Adamson B, Villalta JE, Chen Y, Whitehead EH et al (2014) Genome-Scale CRISPR-Mediated Control of Gene Repression and Activation. Cell 159:647–661
Perez-pinera P, Kocak DD, Vockley CM, Adler AF, Kabadi AM, Polstein LR, et al. (2013) RNA-guided gene activation by CRISPR- Cas9 – based transcription factors. Nature 10
Komor AC, Kim YB, Packer MS, Zuris JA, Liu DR (2016) Programmable editing of a target base in genomic DNA without double-stranded DNA cleavage. Nature 533:420–424
Gaudelli NM, Komor AC, Rees HA, Packer MS, Badran AH, Bryson DI et al (2017) Programmable base editing of A•T to G•C in genomic DNA without DNA cleavage. Nature 551:464
Wang D, Zhang F, Gao G (2020) CRISPR-Based Therapeutic Genome Editing: Strategies and In Vivo Delivery by AAV Vectors. Cell 181:136–150
Ginn SL, Amaya AK, Liao SHY, Zhu E, Cunningham SC, Lee M et al (2020) Efficient in vivo editing of OTC-deficient patient-derived primary human hepatocytes. JHEP Rep 2:100065
Zhao H, Li Y, He L, Pu W, Yu W, Li Y et al (2020) In Vivo AAV-CRISPR/Cas9-Mediated Gene Editing Ameliorates Atherosclerosis in Familial Hypercholesterolemia. Circulation 141:67–79
Richards DY, Winn SR, Dudley S, Nygaard S, Mighell TL, Grompe M et al (2020) AAV-Mediated CRISPR/Cas9 Gene Editing in Murine Phenylketonuria. Mol Ther Methods Clin Dev 17:234–245
Wang D, Li J, Song CQ, Tran K, Mou H, Wu PH et al (2018) Cas9-mediated allelic exchange repairs compound heterozygous recessive mutations in mice. Nat Biotechnol 36:839–842
De Caneva A, Porro F, Bortolussi G, Sola R, Lisjak M, Barzel A, et al. (2019) Coupling AAV-mediated promoterless gene targeting to SaCas9 nuclease to efficiently correct liver metabolic diseases. JCI Insight 5
Chen H, Shi M, Gilam A, Zheng Q, Zhang Y, Afrikanova I et al (2019) Hemophilia A ameliorated in mice by CRISPR-based in vivo genome editing of human Factor VIII. Sci Rep 9:16838
Zhang J-P, Cheng X-X, Zhao M, Li G-H, Xu J, Zhang F, et al. (2019) Curing hemophilia A by NHEJ-mediated ectopic F8 insertion in the mouse. Genome Biology 20
Kim E, Koo T, Park SW, Kim D, Kim K, Cho HY et al (2017) In vivo genome editing with a small Cas9 orthologue derived from Campylobacter jejuni. Nat Commun 8:14500
Koo T, Park SW, Jo DH, Kim D, Kim JH, Cho HY et al (2018) CRISPR-LbCpf1 prevents choroidal neovascularization in a mouse model of age-related macular degeneration. Nat Commun 9:1855
Chung SH, Mollhoff IN, Nguyen U, Nguyen A, Stucka N, Tieu E et al (2020) Factors Impacting Efficacy of AAV-Mediated CRISPR-Based Genome Editing for Treatment of Choroidal Neovascularization. Mol Ther Methods Clin Dev 17:409–417
McCullough KT, Boye SL, Fajardo D, Calabro K, Peterson JJ, Strang CE et al (2019) Somatic Gene Editing of GUCY2D by AAV-CRISPR/Cas9 Alters Retinal Structure and Function in Mouse and Macaque. Hum Gene Ther 30:571–589
Xie C, Zhang YP, Song L, Luo J, Qi W, Hu J et al (2016) Genome editing with CRISPR/Cas9 in postnatal mice corrects PRKAG2 cardiac syndrome. Cell Res 26:1099–1111
Giannelli SG, Luoni M, Castoldi V, Massimino L, Cabassi T, Angeloni D et al (2018) Cas9/sgRNA selective targeting of the P23H Rhodopsin mutant allele for treating retinitis pigmentosa by intravitreal AAV9.PHP.B-based delivery. Hum Mol Genet 27:761–779
Gyorgy B, Nist-Lund C, Pan B, Asai Y, Karavitaki KD, Kleinstiver BP et al (2019) Allele-specific gene editing prevents deafness in a model of dominant progressive hearing loss. Nat Med 25:1123–1130
Yin C, Zhang T, Qu X, Zhang Y, Putatunda R, Xiao X et al (2017) In Vivo Excision of HIV-1 Provirus by saCas9 and Multiplex Single-Guide RNAs in Animal Models. Mol Ther 25:1168–1186
Dash PK, Kaminski R, Bella R, Su H, Mathews S, Ahooyi TM et al (2019) Sequential LASER ART and CRISPR Treatments Eliminate HIV-1 in a Subset of Infected Humanized Mice. Nat Commun 10:2753
Ruan GX, Barry E, Yu D, Lukason M, Cheng SH, Scaria A (2017) CRISPR/Cas9-Mediated Genome Editing as a Therapeutic Approach for Leber Congenital Amaurosis 10. Mol Ther 25:331–341
Nelson CE, Wu Y, Gemberling MP, Oliver ML, Waller MA, Bohning JD et al (2019) Long-term evaluation of AAV-CRISPR genome editing for Duchenne muscular dystrophy. Nat Med 25:427–432
Xu L, Lau YS, Gao Y, Li H, Han R (2019) Life-Long AAV-Mediated CRISPR Genome Editing in Dystrophic Heart Improves Cardiomyopathy without Causing Serious Lesions in mdx Mice. Mol Ther
Zhang Y, Li H, Min YL, Sanchez-Ortiz E, Huang J, Mireault AA et al (2020) Enhanced CRISPR-Cas9 correction of Duchenne muscular dystrophy in mice by a self-complementary AAV delivery system. Sci Adv 6:eaay6812
Moretti A, Fonteyne L, Giesert F, Hoppmann P, Meier AB, Bozoglu T et al (2020) Somatic gene editing ameliorates skeletal and cardiac muscle failure in pig and human models of Duchenne muscular dystrophy. Nat Med 26:207–214
Kemaladewi DU, Maino E, Hyatt E, Hou H, Ding M, Place KM et al (2017) Correction of a splicing defect in a mouse model of congenital muscular dystrophy type 1A using a homology-directed-repair-independent mechanism. Nat Med 23:984–989
Ryu SM, Koo T, Kim K, Lim K, Baek G, Kim ST et al (2018) Adenine base editing in mouse embryos and an adult mouse model of Duchenne muscular dystrophy. Nat Biotechnol 36:536–539
Yang L, Wang L, Huo Y, Chen X, Yin S, Hu Y, et al. (2020) Amelioration of an Inherited Metabolic Liver Disease through Creation of a De Novo Start Codon by Cytidine Base Editing. Mol Ther
Villiger L, Grisch-Chan HM, Lindsay H, Ringnalda F, Pogliano CB, Allegri G et al (2018) Treatment of a metabolic liver disease by in vivo genome base editing in adult mice. Nat Med 24:1519–1525
Lim CKW, Gapinske M, Brooks AK, Woods WS, Powell JE, Zeballos CM et al (2020) Treatment of a Mouse Model of ALS by In Vivo Base Editing. Mol Ther 28:1177–1189
Thakore PI, Kwon JB, Nelson CE, Rouse DC, Gemberling MP, Oliver ML et al (2018) RNA-guided transcriptional silencing in vivo with S. aureus CRISPR-Cas9 repressors. Nat Commun 9:1674
Colasante G, Lignani G, Brusco S, Di Berardino C, Carpenter J, Giannelli S et al (2020) dCas9-Based Scn1a Gene Activation Restores Inhibitory Interneuron Excitability and Attenuates Seizures in Dravet Syndrome Mice. Mol Ther 28:235–253
Ou L, Przybilla MJ, Ahlat O, Kim S, Overn P, Jarnes J et al (2020) A Highly Efficacious PS Gene Editing System Corrects Metabolic and Neurological Complications of Mucopolysaccharidosis Type I. Mol Ther 28:1442–1454
Muenzer J, Prada CE, Burton B, Lau HA, Ficicioglu C, Foo CWP et al (2019) CHAMPIONS: A phase 1/2 clinical trial with dose escalation of SB-913 ZFN-mediated in vivo human genome editing for treatment of MPS II (Hunter syndrome). Mol. Genet. Metab 126:S104
Maeder ML, Stefanidakis M, Wilson CJ, Baral R, Barrera LA, Bounoutas GS et al (2019) Development of a gene-editing approach to restore vision loss in Leber congenital amaurosis type 10. Nat Med 25:229–233
Coppieters F, Lefever S, Leroy BP, De Baere E (2010) CEP290, a gene with many faces: mutation overview and presentation of CEP290base. Hum Mutat 31:1097–1108
Philippidis A (2020) One Small Dose, One Giant Leap for CRISPR Gene Editing. Hum Gene Ther 31:402–404
Levy JM, Yeh WH, Pendse N, Davis JR, Hennessey E, Butcher R et al (2020) Cytosine and adenine base editing of the brain, liver, retina, heart and skeletal muscle of mice via adeno-associated viruses. Nat Biomed Eng 4:97–110
Kuscu C, Parlak M, Tufan T, Yang J, Szlachta K, Wei X et al (2017) CRISPR-STOP : gene silencing through nonsense mutations. Nature Publishing Group 14:2–6
Rossidis AC, Stratigis JD, Chadwick AC, Hartman HA, Ahn NJ, Li H et al (2018) In utero CRISPR-mediated therapeutic editing of metabolic genes. Nat Med 24:1513–1518
Dever DP, Bak RO, Reinisch A, Camarena J, Washington G, Nicolas CE et al (2016) CRISPR/Cas9 beta-globin gene targeting in human haematopoietic stem cells. Nature 539:384–389
Wang J, Exline CM, DeClercq JJ, Llewellyn GN, Hayward SB, Li PW et al (2015) Homology-driven genome editing in hematopoietic stem and progenitor cells using ZFN mRNA and AAV6 donors. Nat Biotechnol 33:1256–1263
Bak RO, Porteus MH (2017) CRISPR-Mediated Integration of Large Gene Cassettes Using AAV Donor Vectors. Cell Rep 20:750–756
Genovese P, Schiroli G, Escobar G, Di Tomaso T, Firrito C, Calabria A et al (2014) Targeted genome editing in human repopulating haematopoietic stem cells. Nature 510:235–240
Dewitt MA, Magis W, Bray NL, Wang T, Berman JR, Urbinati F et al (2016) Selection-free genome editing of the sickle mutation in human adult hematopoietic stem / progenitor cells. Science Translational Medicine 8:360ra134
Pavel-Dinu M, Wiebking V, Dejene BT, Srifa W, Mantri S, Nicolas CE et al (2019) Gene correction for SCID-X1 in long-term hematopoietic stem cells. Nat Commun 10:1634
Eyquem J, Mansilla-Soto J, Giavridis T, van der Stegen SJ, Hamieh M, Cunanan KM et al (2017) Targeting a CAR to the TRAC locus with CRISPR/Cas9 enhances tumour rejection. Nature 543:113–117
Dai X, Park JJ, Du Y, Kim HR, Wang G, Errami Y et al (2019) One-step generation of modular CAR-T cells with AAV-Cpf1. Nat Methods 16:247–254
Traxler EA, Yao Y, Wang YD, Woodard KJ, Kurita R, Nakamura Y et al (2016) A genome-editing strategy to treat beta-hemoglobinopathies that recapitulates a mutation associated with a benign genetic condition. Nat Med 22:987–990
Ye L, Wang J, Tan Y, Beyer AI, Xie F, Muench MO et al (2016) Genome editing using CRISPR-Cas9 to create the HPFH genotype in HSPCs: An approach for treating sickle cell disease and beta-thalassemia. Proc Natl Acad Sci U S A 113:10661–10665
Martyn GE, Wienert B, Yang L, Shah M, Norton LJ, Burdach J et al (2018) Natural regulatory mutations elevate the fetal globin gene via disruption of BCL11A or ZBTB7A binding. Nat Genet 50:498–503
Antoniani C, Meneghini V, Lattanzi A, Felix T, Romano O, Magrin E et al (2018) Induction of fetal hemoglobin synthesis by CRISPR/Cas9-mediated editing of the human beta-globin locus. Blood 131:1960–1973
Holt N, Wang J, Kim K, Friedman G, Wang X, Taupin V et al (2010) Human hematopoietic stem/progenitor cells modified by zinc-finger nucleases targeted to CCR5 control HIV-1 in vivo. Nat Biotechnol 28:839–847
DiGiusto DL, Cannon PM, Holmes MC, Li L, Rao A, Wang J et al (2016) Preclinical development and qualification of ZFN-mediated CCR5 disruption in human hematopoietic stem/progenitor cells. Mol Ther Methods Clin Dev 3:16067
Xu L, Yang H, Gao Y, Chen Z, Xie L, Liu Y et al (2017) CRISPR/Cas9-Mediated CCR5 Ablation in Human Hematopoietic Stem/Progenitor Cells Confers HIV-1 Resistance In Vivo. Mol Ther 25:1782–1789
Xu L, Wang J, Liu Y, Xie L, Su B, Mou D et al (2019) CRISPR-Edited Stem Cells in a Patient with HIV and Acute Lymphocytic Leukemia. N Engl J Med 381:1240–1247
Quillent C, Oberlin E, Braun J, Rousset D, Gonzalez-Canali G, Métais P et al (1998) HIV-1-resistance phenotype conferred by combination of two separate inherited mutations of CCR5 gene. The Lancet 351:14–18
Li C, Mei H, Hu Y (2020) Applications and explorations of CRISPR/Cas9 in CAR T-cell therapy. Brief Funct Genomics 19:175–182
Miller DG, Petek LM, Russell DW (2004) Adeno-associated virus vectors integrate at chromosome breakage sites. Nat Genet 36:767–773
Kaeppel C, Beattie SG, Fronza R, van Logtenstein R, Salmon F, Schmidt S et al (2013) A largely random AAV integration profile after LPLD gene therapy. Nat Med 19:889–891
Borel F, Kay MA, Mueller C (2014) Recombinant AAV as a platform for translating the therapeutic potential of RNA interference. Mol Ther 22:692–701
Donsante A, Miller DG, Li Y, Vogler C, Brunt EM, Russell DW et al (2007) AAV vector integration sites in mouse hepatocellular carcinoma. Science 317:477
Wang PR, Xu M, Toffanin S, Li Y, Llovet JM, Russell DW (2012) Induction of hepatocellular carcinoma by in vivo gene targeting. Proc Natl Acad Sci U S A 109:11264–11269
Bell P, Wang L, Lebherz C, Flieder DB, Bove MS, Wu D et al (2005) No evidence for tumorigenesis of AAV vectors in a large-scale study in mice. Mol Ther 12:299–306
Li H, Malani N, Hamilton SR, Schlachterman A, Bussadori G, Edmonson SE et al (2011) Assessing the potential for AAV vector genotoxicity in a murine model. Blood 117:3311–3319
Niemeyer GP, Herzog RW, Mount J, Arruda VR, Tillson DM, Hathcock J et al (2009) Long-term correction of inhibitor-prone hemophilia B dogs treated with liver-directed AAV2-mediated factor IX gene therapy. Blood 113:797–806
Gil-Farina I, Fronza R, Kaeppel C, Lopez-Franco E, Ferreira V, D’Avola D et al (2016) Recombinant AAV Integration Is Not Associated With Hepatic Genotoxicity in Nonhuman Primates and Patients. Mol Ther 24:1100–1105
Park KJ, Lee J, Park JH, Joh JW, Kwon CH, Kim JW (2016) Adeno-Associated Virus 2-Mediated Hepatocellular Carcinoma is Very Rare in Korean Patients. Ann Lab Med 36:469–474
Berns KI, Byrne BJ, Flotte TR, Gao G, Hauswirth WW, Herzog RW et al (2015) Adeno-Associated Virus Type 2 and Hepatocellular Carcinoma? Hum Gene Ther 26:779–781
Hanlon KS, Kleinstiver BP, Garcia SP, Zaborowski MP, Volak A, Spirig SE et al (2019) High levels of AAV vector integration into CRISPR-induced DNA breaks. Nat Commun 10:4439
Mali P, Aach J, Stranges PB, Esvelt KM, Moosburner M, Kosuri S et al (2013) CAS9 transcriptional activators for target specificity screening and paired nickases for cooperative genome engineering. Nat Biotechnol
Chen S, Yao Y, Zhang Y, Fan G (2020) CRISPR system: Discovery, development and off-target detection. Cell Signal 70:109577
Liu G, Zhang Y, Zhang T (2020) Computational approaches for effective CRISPR guide RNA design and evaluation. Comput Struct Biotechnol J 18:35–44
Manghwar H, Li B, Ding X, Hussain A, Lindsey K, Zhang X et al (2020) CRISPR/Cas Systems in Genome Editing: Methodologies and Tools for sgRNA Design, Off-Target Evaluation, and Strategies to Mitigate Off-Target Effects. Adv Sci (Weinh) 7:1902312
Yin H, Song CQ, Dorkin JR, Zhu LJ, Li Y, Wu Q et al (2016) Therapeutic genome editing by combined viral and non-viral delivery of CRISPR system components in vivo. Nat Biotechnol 34:328–333
Kim D, Bae S, Park J, Kim E, Kim S, Yu HR et al (2015) Digenome-seq: genome-wide profiling of CRISPR-Cas9 off-target effects in human cells. Nat Methods 12:237–243 1 p following 43
Wienert B, Wyman SK, Richardson CD, Yeh CD, Akcakaya P, Porritt MJ et al (2019) Unbiased detection of CRISPR off-targets in vivo using DISCOVER-Seq. Science 364:286–289
Tsai SQ, Zheng Z, Nguyen NT, Liebers M, Topkar VV, Thapar V et al (2015) GUIDE-seq enables genome-wide profiling of off-target cleavage by CRISPR-Cas nucleases. Nat Biotechnol 33:187–197
Crosetto N, Mitra A, Silva MJ, Bienko M, Dojer N, Wang Q et al (2013) Nucleotide-resolution DNA double-strand break mapping by next-generation sequencing. Nat Methods 10:361–365
Tsai SQ, Nguyen NT, Malagon-Lopez J, Topkar VV, Aryee MJ, Joung JK (2017) CIRCLE-seq: a highly sensitive in vitro screen for genome-wide CRISPR-Cas9 nuclease off-targets. Nat Methods 14:607–614
Cameron P, Fuller CK, Donohoue PD, Jones BN, Thompson MS, Carter MM et al (2017) Mapping the genomic landscape of CRISPR-Cas9 cleavage. Nat Methods 14:600–606
Favre D, Provost N, Blouin V, Blancho G, Cherel Y, Salvetti A et al (2001) Immediate and long-term safety of recombinant adeno-associated virus injection into the nonhuman primate muscle. Mol Ther 4:559–566
Srivastava A (2016) In vivo tissue-tropism of adeno-associated viral vectors. Curr Opin Virol 21:75–80
Baltimore D, Berg P, Botchan M, Carroll D, Charo RA, Church G et al (2015) Biotechnology. A prudent path forward for genomic engineering and germline gene modification. Science 348:36–38
Erles K, Rohde V, Thaele M, Roth S, Edler L, Schlehofer JR (2001) DNA of adeno-associated virus (AAV) in testicular tissue and in abnormal semen samples. Hum Reprod 16:2333–2337
Wang Z, Zhu T, Qiao C, Zhou L, Wang B, Zhang J et al (2005) Adeno-associated virus serotype 8 efficiently delivers genes to muscle and heart. Nat Biotechnol 23:321–328
Arruda VR, Fields PA, Milner R, Wainwright L, De Miguel MP, Donovan PJ et al (2001) Lack of germline transmission of vector sequences following systemic administration of recombinant AAV-2 vector in males. Mol Ther 4:586–592
Favaro P, Downey HD, Zhou JS, Wright JF, Hauck B, Mingozzi F et al (2009) Host and vector-dependent effects on the risk of germline transmission of AAV vectors. Mol Ther 17:1022–1030
Rajasekaran S, Thatte J, Periasamy J, Javali A, Jayaram M, Sen D et al (2018) Infectivity of adeno-associated virus serotypes in mouse testis. BMC Biotechnol 18:70
Charlesworth CT, Deshpande PS, Dever DP, Camarena J, Lemgart VT, Cromer MK et al (2019) Identification of preexisting adaptive immunity to Cas9 proteins in humans. Nat Med 25:249–254
Wagner DL, Amini L, Wendering DJ, Burkhardt LM, Akyuz L, Reinke P et al (2019) High prevalence of Streptococcus pyogenes Cas9-reactive T cells within the adult human population. Nat Med 25:242–248
Crudele JM, Chamberlain JS (2018) Cas9 immunity creates challenges for CRISPR gene editing therapies. Nat Commun 9:3497
McIntosh J, Lenting PJ, Rosales C, Lee D, Rabbanian S, Raj D et al (2013) Therapeutic levels of FVIII following a single peripheral vein administration of rAAV vector encoding a novel human factor VIII variant. Blood 121:3335–3344
Kulkarni JA, Witzigmann D, Chen S, Cullis PR, van der Meel R (2019) Lipid Nanoparticle Technology for Clinical Translation of siRNA Therapeutics. Acc Chem Res 52:2435–2444
Rui Y, Wilson DR, Green JJ (2019) Non-Viral Delivery To Enable Genome Editing. Trends Biotechnol 37:281–293
Lee K, Conboy M, Park HM, Jiang F, Kim HJ, Dewitt MA et al (2017) Nanoparticle delivery of Cas9 ribonucleoprotein and donor DNA in vivo induces homology-directed DNA repair. Nat Biomed Eng 1:889–901
Jiang C, Mei M, Li B, Zhu X, Zu W, Tian Y et al (2017) A non-viral CRISPR/Cas9 delivery system for therapeutic gene targeting in vivo. Cell Res
Dolgin E (2020) Specter of eye toxicity looms over BCMA-targeted therapy. Nat Biotechnol 38:1363–1365
Anzalone AV, Randolph PB, Davis JR, Sousa AA, Koblan LW, Levy JM, et al. (2019) Search-and-replace genome editing without double-strand breaks or donor DNA. Nature
Abudayyeh OO, Gootenberg JS, Konermann S, Joung J, Slaymaker IM, Cox DBT et al (2016) C2c2 is a single-component programmable RNA-guided RNA-targeting CRISPR effector. Science 353:aaf5573
Abudayyeh OO, Gootenberg JS, Essletzbichler P, Han S, Joung J, Belanto JJ, et al. (2017) RNA targeting with CRISPR-Cas13. Nature
Konermann S, Lotfy P, Brideau NJ, Oki J, Shokhirev MN, Hsu PD (2018) Transcriptome Engineering with RNA-Targeting Type VI-D CRISPR Effectors. Cell 173:665–76 e14
Zhao X, Liu L, Lang J, Cheng K, Wang Y, Li X et al (2018) A CRISPR-Cas13a system for efficient and specific therapeutic targeting of mutant KRAS for pancreatic cancer treatment. Cancer Lett 431:171–181
Abbott TR, Dhamdhere G, Liu Y, Lin X, Goudy L, Zeng L, et al. (2020) Development of CRISPR as a prophylactic strategy to combat novel coronavirus and influenza. bioRxiv preprint
Cring MR, Sheffield VC (2020) Gene therapy and gene correction: targets, progress, and challenges for treating human diseases. Gene Ther
Li H, Yang Y, Hong W, Huang M, Wu M, Zhao X (2020) Applications of genome editing technology in the targeted therapy of human diseases: mechanisms, advances and prospects. Signal Transduct Target Ther 5:1
Funding
This study was supported by funds provided by the Research Grants Council of Hong Kong (14119518, 14116719, 14115520 to B.F.; T13-605/18-W to N.I.; and T13-402/17-N to L.Q.), and in part by the Children’s Thalassaemia Foundation in Hong Kong (CTFHK 2018/02 to B.F.), the National Natural Science Foundation of China (31771635 to B.F.), and the Health@InnoHK Program launched by Innovation Technology Commission of the Hong Kong SAR, China. Z. Z. received a graduate studentship award from the Chinese University of Hong Kong.
Author information
Authors and Affiliations
Contributions
X. H. and Z. Z. drew the figure and the tables; X. H., B. U., Z. Z., C. N. and B. F. wrote the paper. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
This article reviews literature and therefore does not require ethics approval and consent to participate.
Conflict of interest
The authors declare that they have no competing interests.
Consent for publication
Not applicable
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
He, X., Urip, B.A., Zhang, Z. et al. Evolving AAV-delivered therapeutics towards ultimate cures. J Mol Med 99, 593–617 (2021). https://doi.org/10.1007/s00109-020-02034-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-020-02034-2