Abstract
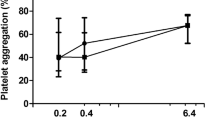
Reduced effectiveness of the most common antiplatelet drug, acetylsalicylic acid (ASA, aspirin), in diabetes mellitus has been associated with a lowered platelet sensitivity to ASA and related to glycemic control in diabetic patients. Our objectives were (a) to monitor the chemical background of how chronic hyperglycemia affects platelet response to ASA in diabetes and (b) to study a chemical competition between the amount of bound acetyl residues and the extent of protein glycation in blood platelets. Using whole-blood impedance aggregometry and platelet function analyzer (PFA-100) we observed a reduced platelet response to ASA in diabetic patients (14% vs. 79% for PFA-100 collagen-epinephrine occlusion time) and an association between the index of glycemic control and platelet refractoriness to ASA (rS=−0.378). Impaired platelet response to ASA was related to enhanced platelet protein glycation (3.6±0.4 in diabetes vs. 2.3±0.4 µmol fructosamine/µg protein in control) and reduced incorporation of acetyl residue into proteins of platelets from diabetic patients (47.4±2.0 in control vs. 33.1±0.7 µmol acetyl/µg protein in diabetic subjects). Incubation of blood platelets with increasing concentrations of glucose and ASA under in vitro conditions led to excessive modification in protein amino groups: glucose and ASA competed with each other in the course of nonenzymatic modifications, glycosylation, or acetylation, and their contributions to the occupancy of protein amino groups (R2=0.22 for glucose, R2=0.43 for ASA) were dependent upon the concentrations of glucose and ASA. Overall the effects of high glucose and high ASA on the overall occupancy of protein free amino groups are not additive. While at higher concentrations ASA overcomes the effects of hyperglycemia and retards glycation, high glucose makes acetylation less efficient, and therefore the resultant chemical modification becomes greatly reduced. In conclusion, diminished susceptibility of various platelet proteins and receptors on blood platelet membranes to acetylation and high ambient glucose might underlie the apparently differentiated sensitivity of blood platelets to ASA and determine platelet “insensitivity to aspirin” in diabetic patients





Similar content being viewed by others
Abbreviations
- AA :
-
Arachidonic acid
- ASA :
-
Acetylsalicylic acid
- [ 14 C]ASA :
-
Acetyl-1-[14C]salicylic acid
- BSA :
-
Bovine serum albumin
- CADP :
-
Collagen and ADP
- CEPI :
-
Collagen and epinephrine
- CS :
-
Comprehensive score
- CT :
-
Closure time
- WBEA :
-
Whole-blood impedance (electrical) aggregometry
References
Colwell JA, the American Diabetes Association (2004) Aspirin therapy in diabetes. Diabetes Care 27 [Suppl 1]:S72–S73
Gum PA, Kottke-Marchant K, Poggio ED, Gurm H, Welsh PA, Brooks L, Sapp SK, Topol EJ (2001) Profile and prevalence of aspirin resistance in patients with cardiovascular disease. Am J Cardiol 88:230–235
Sivenius J, Laakso M, Riekkinen P, Smets P, Lowenthal A (1992) European stroke prevention study: effectiveness of antiplatelet therapy in diabetic patients in secondary prevention of stroke. Stroke 23:851–854
Gum PA, Kottke-Marchant K, Welsh PA, White J, Topol EJ (2003) A prospective, blinded determination of the natural history of aspirin resistance among stable patients with cardiovascular disease. J Am Coll Cardiol 41:961–965
McKee SA, Sane DC, Deliargyris EN (2002) Aspirin resistance in cardiovascular disease: a review of prevalence, mechanisms, and clinical significance. Thromb Haemost 88:711–715
Cambria-Kiely JA, Gandhi PJ (2002) Possible mechanisms of aspirin resistance. J Thromb Thrombolysis 13:49–56
Patrono C (2003) Aspirin resistance: definition, mechanisms and clinical read-outs. J Thromb Haemost 1:1710–1713
Mori TA, Vandongen R, Douglas AJ, McCulloch RK, Burke V (1992) Differential effect of aspirin on platelet aggregation in IDDM. Diabetes 41:261–266
Sacco M, Pellegrini F, Roncaglioni MC, Avanzini F, Tognoni G, Nicolucci A (2003) Primary prevention of cardiovascular events with low-dose aspirin and vitamin E in type 2 diabetic patients: results of the Primary Prevention Project (PPP) trial. Diabetes Care 26:3264–3272
Watala C, Golanski J, Pluta J, Boncler M, Rozalski M, Wieclawska B, Kropiwnicka A, Drzewoski J (2004) Reduced sensitivity of platelets from type 2 diabetic patients to acetylsalicylic acid (aspirin)—its relation to metabolic control. Thromb Res 113:101–113
Tschoepe D, Roesen P, Esser J, Schwippert B, Nieuwenhuis HK, Kehrel B, Gries FA (1991) Large platelets circulate in an activated state in diabetes mellitus. Semin Thromb Hemost 17:433–438
Pampus EC van, Huijgens PC, Zevenbergen A, Twaalfhoven H, van Kamp GJ, Langenhuijsen MM (1993) Influence of aspirin on human megakaryocyte prostaglandin synthesis. Eur J Haematol 50:264–268
Watala C, Boncler M, Pietrucha T, Trojanowski Z (1999) Possible mechanisms of the altered platelet volume distribution in type 2 diabetes—may the increased platelet activation contribute to platelet size heterogeneity? Platelets 10:52–60
Loll PJ, Picot D, Garavito RM (1995) The structural basis of aspirin activity inferred from the crystal structure of inactivated prostaglandin H2 synthase. Nat Struct Biol 2:637–643
Cherian M, Abraham EC (1993) Glycation of human lens crystallins: effect of age and aspirin treatment. Ophthalmic Res 25:349–354
Contreras I, Reiser KM, Martinez N, Giansante E, Lopez T, Suarez N, Postalian S, Molina M, Gonzalez F, Sanchez MR, Camejo M, Blanco MC (1997) Effects of aspirin or basic amino acids on collagen cross-links and complications in NIDDM. Diabetes Care 20:832–835
Hun-Opfer C, Mata-Segreda JF (1986) Non-enzymatic acetylation of proteins by aspirin as protection against the secondary complications of diabetes mellitus. Acta Physiol Pharmacol Latinoam 36:313–316
Jorneskog G, Fatah K, Blomback M (1998) Fibrin gel structure in diabetic patients before and during treatment with acetylsalicylic acid: a pilot study. Fibrinolysis Proteolysis 12:360–365
Malik NS, Meek KM (1994) The inhibition of sugar-induced structural alterations in collagen by aspirin and other compounds. Biochem Biophys Res Commun 199:683–686
Shastri GV, Thomas M, Victoria AJ, Selvakumar R, Kanagasabapathy AS, Thomas K, Lakshmi (1998) Effect of aspirin and sodium salicylate on cataract development in diabetic rats. Indian J Exp Biol 36:651–657
Swamy MS, Abraham EC (1989) Inhibition of lens crystallin glycation and high molecular weight aggregate formation by aspirin in vitro and in vivo. Invest Ophthalmol Vis Sci 30:1120–1126
Winocour PD, Watala C, Perry DW, Kinlough-Rathbone RL (1992) Decreased platelet membrane fluidity due to glycation or acetylation of membrane proteins. Thromb Haemost 68:577–582
Rendell M, Nierenberg J, Brannan C, Valentine JL, Stephen PM, Dodds S, Mercer P, Smith PK, Walder J (1986) Inhibition of glycation of albumin and hemoglobin by acetylation in vitro and in vivo. J Lab Clin Med 108:286–293
Swamy-Mruthinti S, Carter AL (1999) Acetyl-L-carnitine decreases glycation of lens proteins: in vitro studies. Exp Eye Res 69:109–115
Drzewoski J, Watala C (2004) Is aspirin resistance a real problem in people with type 2 diabetes? Response to Sacco et al. Diabetes Care 27:1245–1246
Hanai T, Uchida M, Amao M, Ikeda C, Koizumi K, Kinoshita T (2000) Selective chemiluminescence analysis of amadori form of glycated human serum albumin. J Liq Chrom Rel Technol 23:3119–3131
Zar J (1999) Biostatistical analysis. Simon & Schuster/A Viacom, Prentice-Hall
Benedito MA (1997) Fluorimetric determination of tissue distribution and differences between the activity of aspirin esterases I and II in mice and rats. J Pharm Pharmacol 49:273–276
Rozalski M, Boncler M, Golanski J, Watala C (2001) Effects of fibrinogen receptor antagonist GR144053F and aurintricarboxylic acid on platelet activation and degranulation. Biochem Pharmacol 62:1399–1408
Mammen EF, Comp PC, Gosselin R, Greenberg C, Hoots WK, Kessler CM, Larkin EC, Liles D, Nugent DJ (1998) PFA-100 system: a new method for assessment of platelet dysfunction. Semin Thromb Hemost 24:195–202
Bartlett A, Stableforth P, Voller A (1976) Factor VIII related antigen: measurement by enzyme immunoassay. BMJ 1:994–996
Ray MJ, Hawson GA, Just SJ, McLachlan G, O’Brien M (1994) Relationship of platelet aggregation to bleeding after cardiopulmonary bypass. Ann Thorac Surg 57:981–986
Watala C, Golanski J, Rozalski M, Boncler M, Luzak B, Baraniak J, Korczynski D, Drygas W (2003) Is platelet aggregation a more important contributor than platelet adhesion to the overall platelet-related primary haemostasis measured by PFA-100? Thromb Res 109:299–306
Boncler MA, Golanski J, Paczuski R, Watala C (2002) Polymorphisms of glycoprotein Ib affect the inhibition by aurintricarboxylic acid of the von Willebrand factor dependent platelet aggregation. J Mol Med 80:796–801
Walkowiak B, Michalak E, Koziolkiewicz W, Cierniewski CS (1989) Rapid photometric method for estimation of platelet count in blood plasma or platelet suspension. Thromb Res 56:763–766
Smith PK, Krohn RI, Hermanson GT, Mallia AK, Gartner FH, Provenzano MD, Fujimoto EK, Goeke NM, Olson BJ, Klenk DC (1985) Measurement of protein using bicinchoninic acid. Anal Biochem 150:76–85
Johnson P, Garland PB (1982) Fluorescent triplet probes for measuring the rotational diffusion of membrane proteins. Biochem J 203:313–321
Sashidhar RB, Capoor AK, Ramana D (1994) Quantitation of epsilon-amino group using amino acids as reference standards by trinitrobenzene sulfonic acid. A simple spectrophotometric method for the estimation of hapten to carrier protein ratio. J Immunol Methods 167:121–127
Armitage P, Berry G, Matthews JNS (2002) Statistical methods in medical research. Blackwell, Oxford
Hasegawa Y, Suehiro A, Higasa S, Namba M, Kakishita E (2002) Enhancing effect of advanced glycation end products on serotonin-induced platelet aggregation in patients with diabetes mellitus. Thromb Res 107:319–323
Li Y, Woo V, Bose R (2001) Platelet hyperactivity and abnormal Ca(2+) homeostasis in diabetes mellitus. Am J Physiol Heart Circ Physiol 280:H1480–H1489
Davi G, Ciabattoni G, Consoli A, Mezzetti A, Falco A, Santarone S, Pennese E, Vitacolonna E, Bucciarelli T, Costantini F, Capani F, Patrono C (1999) In vivo formation of 8-iso-prostaglandin F2alpha and platelet activation in diabetes mellitus: effects of improved metabolic control and vitamin E supplementation. Circulation 99:224–229
Colwell JA, Nesto RW (2003) The platelet in diabetes: focus on prevention of ischemic events. Diabetes Care 26:2181–2188
Friend M, Vucenik I, Miller M (2003) Research pointers: platelet responsiveness to aspirin in patients with hyperlipidaemia. BMJ 326:82–83
DiMinno G, Silver MJ, Cerbone AM, Murphy S (1986) Trial of repeated low-dose aspirin in diabetic angiopathy. Blood 68:886–891
Winocour PD (1994) Platelets, vascular disease, and diabetes mellitus. Can J Physiol Pharmacol 72:295–303
Watala C, Gwozdzinski K (1993) Effect of aspirin on conformation and dynamics of membrane proteins in platelets and erythrocytes. Biochem Pharmacol 45:1343–1349
Acknowledgements
This study was supported by the Polish State Committee for Scientific Research (3P05B10222 and 3P05A08022), the Medical University of Lodz (502-11-698, 502-16-699 and 503-130-2), and a NATO Cooperative Linkage Grant (lst.clg.980106).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Watala, C., Pluta, J., Golanski, J. et al. Increased protein glycation in diabetes mellitus is associated with decreased aspirin-mediated protein acetylation and reduced sensitivity of blood platelets to aspirin. J Mol Med 83, 148–158 (2005). https://doi.org/10.1007/s00109-004-0600-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-004-0600-x