Abstract
Purpose
Traumatic brain injury is one of the leading causes of disability worldwide. Mild traumatic brain injury (TBI) is the most common and benign form of TBI, usually referred to by the medical term “concussion”. The purpose of our systematic review and meta-analysis was to explore the role of serum and CSF neurofilament light chain (NfL) as a potential biomarker in concussion.
Methods
We systematically searched PubMed, Web of Science, and Cochrane databases using specific keywords. As the primary outcome, we assessed CSF or serum NfL levels in patients with concussion and head impacts versus controls. The role of NfL in patients with concussion and head impacts compared to healthy controls was also assessed, as well as in sports-related and military-related conditions.
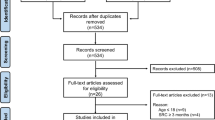
Results
From the initial 617 identified studies, we included 24 studies in our qualitative analysis and 14 studies in our meta-analysis. We found a statistically significant increase of serum NfL in patients suffering from a concussion or head impacts compared to controls (p = 0.0023), highlighting its potential role as a biomarker. From our sub-group analyses, sports-related concussion and mild TBI were mostly correlated with increased serum NfL values. Compared to controls, sports-related concussion was significantly associated with higher NfL levels (p = 0.0015), while no association was noted in patients suffering from head impacts or military-related TBI.
Conclusion
Serum NfL levels are higher in all patients suffering from concussion compared to healthy controls. The sports-related concussion was specifically associated with higher levels of NfL. Further studies exploring the use of NfL as a diagnostic and prognostic biomarker in mild TBI and head impacts are needed.











Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Schiller JS, Lucas JW, Peregoy JA Summary health statistics for u.s. Adults: national health interview survey, 2011. Vital Health Stat. 10 2012;2012(256):1–218.
Sussman ES, et al. Mild traumatic brain injury and concussion: terminology and classification. Handb Clin Neurol. 2018;158:21–4.
Unden J, et al. Scandinavian guidelines for initial management of minimal, mild and moderate head injuries in adults: an evidence and consensus-based update. BMC Med. 2013;11:50.
Balestreri M, et al. Predictive value of glasgow coma scale after brain trauma: change in trend over the past ten years. J Neurol Neurosurg Psychiatry. 2004;75(1):161–2.
Harmon KG, et al. American medical society for sports medicine position statement on concussion in sport. Clin J Sport Med. 2019;29(2):87–100.
Choe MC. The pathophysiology of concussion. Curr Pain Headache Rep/. 2016;20(6):42.
Rawlings S, Takechi R, Lavender AP. Effects of sub-concussion on neuropsychological performance and its potential mechanisms: a narrative review. Brain Res Bull. 2020;165:56–62.
Mainwaring L, et al. Subconcussive head impacts in sport: A Systematic review of the evidence. Int J Psychophysiol. 2018;132(Pt A):39–54.
Broglio SP, et al. Cognitive decline and aging: the role of concussive and subconcussive impacts. Exerc Sport Sci Rev. 2012;40(3):138–44.
Bailes JE, et al. Role of subconcussion in repetitive mild traumatic brain injury. J Neurosurg. 2013;119(5):1235–45.
Gaetani L, et al. Neurofilament light chain as a biomarker in neurological disorders. J Neurol Neurosurg Psychiatry. 2019;90(8):870–81.
Khalil M, et al. Neurofilaments as biomarkers in neurological disorders. Nat Rev Neurol. 2018;14(10):577–89.
Mondello S, et al. Neuronal and glial markers are differently associated with computed tomography findings and outcome in patients with severe traumatic brain injury: a case control study. Crit Care. 2011;15(3):R156.
Shahim P, et al. Serum neurofilament light protein predicts clinical outcome in traumatic brain injury. Sci Rep. 2016;6:36791.
Wirsching A, et al. Association of acute increase in plasma neurofilament light with repetitive subconcussive head impacts: a pilot randomized control trial. J Neurotrauma. 2019;36(4):548–53.
Guedes VA, et al. Exosomal neurofilament light: a prognostic biomarker for remote symptoms after mild traumatic brain injury? Neurology. 2020;94(23):e2412–23.
Moher D et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Management of Concussion/m, T.B.I.W.G., VA/DoD Clinical Practice Guideline for Management of Concussion/Mild Traumatic Brain Injury. J Rehabil Res Dev. 2009;46(6):CP1–68.
McCrea M, et al. Official position of the military TBI task force on the role of neuropsychology and rehabilitation psychology in the evaluation, management, and research of military veterans with traumatic brain injury. Clin Neuropsychol. 2008;22(1):10–26.
McCrory P, et al. Consensus statement on concussion in sport-the 5(th) international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838–47.
Silverberg ND, et al. Management of concussion and mild traumatic brain injury: a synthesis of practice guidelines. Arch Phys Med Rehabil. 2020;101(2):382–93.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13.
Bernick C, et al. Longitudinal performance of plasma neurofilament light and tau in professional fighters: the professional fighters brain health study. J Neurotrauma. 2018;35(20):2351–6.
Bevilacqua ZW, Huibregtse ME, Kawata K. In vivo protocol of controlled subconcussive head impacts for the validation of field study data. J Vis Exp. 2019;(146).
Boutte AM et al. Brain-related proteins as serum biomarkers of acute, subconcussive blast overpressure exposure: a cohort study of military personnel. PLoS One. 2019;14(8):e0221036.
Dickstein DL et al. Brain and blood biomarkers of tauopathy and neuronal injury in humans and rats with neurobehavioral syndromes following blast exposure. Mol Psychiatry. 2020. https://doi.org/10.1038/s41380-020-0674-z.
McCrea M et al. Association of blood biomarkers with acute sport-related concussion in collegiate Athletes: findings From the NCAA and department of defense CARE consortium. JAMA Netw Open. 2020;3(1):e1919771.
Oliver JM, et al. Serum neurofilament light in American football athletes over the course of a season. J Neurotrauma. 2016;33(19):1784–9.
Shahim P, et al. Neurofilament light and tau as blood biomarkers for sports-related concussion. Neurology. 2018;90(20):e1780–8.
Shahim P, et al. Neurofilament light as a biomarker in traumatic brain injury. Neurology. 2020;95(6):e610–22.
Shahim P, et al. Serum neurofilament light as a biomarker for mild traumatic brain injury in contact sports. Neurology. 2017;88(19):1788–94.
Thangavelu B et al. Overpressure exposure from .50-caliber rifle training is associated with increased amyloid beta peptides in serum. Front Neurol 2020;11:620.
Wallace C et al. Heading in soccer increases serum neurofilament light protein and SCAT3 symptom metrics. BMJ Open Sport Exerc Med. 2018;4(1):e000433.
Wallace C et al. No change in plasma tau and serum neurofilament light concentrations in adolescent athletes following sport-related concussion. PLoS One. 2018;13(10):e0206466.
Abu-Rumeileh S, et al. The CSF neurofilament light signature in rapidly progressive neurodegenerative dementias. Alzheimers Res Ther. 2018;10(1):3.
Neselius S et al. CSF-biomarkers in Olympic boxing: diagnosis and effects of repetitive head trauma. PLoS One. 2012;7(4):e33606.
Asken BM, et al. Acute effects of sport-related concussion on serum glial fibrillary acidic protein, ubiquitin C-terminal hydrolase L1, total tau, and neurofilament light measured by a multiplex assay. J Neurotrauma. 2020;37(13):1537–45.
Oliver JM et al. Fluctuations in blood biomarkers of head trauma in NCAA football athletes over the course of a season. J Neurosurg 2018;1–8.
Pattinson CL et al. Plasma biomarker concentrations associated with return to sport following sport-related concussion in collegiate athletes-a concussion assessment, research, and education (CARE) consortium study. JAMA Netw Open 2020;3(8):e2013191.
Rubin LH, et al. NFL blood levels are moderated by subconcussive impacts in a cohort of college football players. Brain Inj. 2019;33(4):456–62.
Sandmo SB, et al. Neurofilament light and tau in serum after head-impact exposure in soccer. Brain Inj. 2020;34(5):602–9.
Taghdiri F, et al. Neurofilament-light in former athletes: a potential biomarker of neurodegeneration and progression. Eur J Neurol. 2020;27(7):1170–7.
Edwards KA, et al. Blast exposure results in tau and neurofilament light chain changes in peripheral blood. Brain Inj. 2020;34(9):1213–21.
Misquitta K, et al. The relationship between brain atrophy and cognitive-behavioural symptoms in retired Canadian football players with multiple concussions. Neuroimage Clin. 2018;19:551–8.
Winston CN, et al. Assessing neuronal and astrocyte derived exosomes from individuals with mild traumatic brain injury for markers of neurodegeneration and cytotoxic activity. Front Neurosci. 2019;13:1005.
Powell JR, et al. Neuroinflammatory biomarkers associated with mild traumatic brain injury history in special operations forces combat soldiers. J Head Trauma Rehabil. 2020;35(5):300–7.
Centers for Disease, C. and Prevention, Nonfatal traumatic brain injuries related to sports and recreation activities among persons aged </=19 years--United States, 2001–2009. MMWR Morb Mortal Wkly Rep. 2011;60(39):1337–42.
Castile L, et al. The epidemiology of new versus recurrent sports concussions among high school athletes, 2005–2010. Br J Sports Med. 2012;46(8):603–10.
Bouvier D, et al. Interest of blood biomarkers to predict lesions in medical imaging in the context of mild traumatic brain injury. Clin Biochem. 2020;85:5–11.
Unden J, Romner B. Can low serum levels of S100B predict normal CT findings after minor head injury in adults?: an evidence-based review and meta-analysis. J Head Trauma Rehabil. 2010;25(4):228–40.
Gan ZS, et al. Blood biomarkers for traumatic brain injury: a quantitative assessment of diagnostic and prognostic accuracy. Front Neurol. 2019;10:446.
Edalatfar M et al. Biofluid Biomarkers in Traumatic Brain Injury: A Systematic Scoping Review. Neurocrit Care. 2021. https://doi.org/10.1007/s12028-020-01173-1.
Shahim P, et al. Blood biomarkers for brain injury in concussed professional ice hockey players. JAMA Neurol. 2014;71(6):684–92.
Jin M, Cao L, Dai YP. Role of Neurofilament light chain as a potential biomarker for Alzheimer’s disease: a correlative meta-analysis. Front Aging Neurosci. 2019;11:254.
Karantali E et al. The role of neurofilament light chain in frontotemporal dementia: a meta-analysis. Aging Clin Exp Res, 2021;33(4):869–881.
Gao W et al. Neurofilament light chain level in traumatic brain injury: A system review and meta-analysis. Medicine (Baltimore). 2020;99(38):e22363.
Hiskens MI, et al. Blood biomarkers for assessment of mild traumatic brain injury and chronic traumatic encephalopathy. Biomarkers. 2020;25(3):213–27.
Khalil M, et al. Serum neurofilament light levels in normal aging and their association with morphologic brain changes. Nat Commun. 2020;11(1):812.
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
Conceptualization: MI; methodology: MI, KE; formal analysis and investigation: MI, KE; writing—original draft preparation: KE; writing—review, and editing: KD, CS, MJ, PF, MI; supervision: MI, KD.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
The final version of the paper has been read and approved by all authors.
Rights and permissions
About this article
Cite this article
Karantali, E., Kazis, D., McKenna, J. et al. Neurofilament light chain in patients with a concussion or head impacts: a systematic review and meta-analysis. Eur J Trauma Emerg Surg 48, 1555–1567 (2022). https://doi.org/10.1007/s00068-021-01693-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-021-01693-1