Abstract
Objective
An arthroscopic technique for the reconstruction of the posterolateral corner combined with posterior cruciate ligament (PCL) reconstruction was developed.
Indications
Posterolateral rotational instabilities of the knee. Combined lesions of the PCL, the popliteus complex (PLT) and the posterolateral corner. Isolated PLT lesions lacking static stabilizing function.
Contraindications
Neuromuscular disorders; knee deformities or fractures; severe posterolateral soft tissue damage.
Surgical technique
Six arthroscopic portals are necessary. Using the posteromedial portal, resect dorsal septum with a shaver. Visualize the PCL, the lateral femoral condyle and the posterolateral recessus with the PLT. Dissect the popliteomeniscal fibers; retract PLT until sulcus popliteus is visualized. Drill a 6-mm tunnel anteriorly into the distal third of the sulcus popliteus. Visualize femoral footprint of the PLT and place an anatomical drill tunnel. Pull the popliteus bypass graft into the knee and fix with bioscrews. Fix the reconstructed PCL. In cases of additional LCL injury, reconstruct LCL with autologous graft.
Postoperative management
Partial weight-bearing for 6 weeks, range of motion exercises, quadriceps-strengthening exercises on postoperative day 1. Full extension allowed immediately with flexion limited to 20° for 2 weeks, to 45° for up to week 4, and to 60° up to week 6. Use a PCL brace for 3 months, running and squatting exercises allowed after 3 months.
Results
In the 35 patients treated, no technique-related complications. After 1 year, 12 patients had a mean Lysholm Score of 88.6 (± 8.7) points and a side-to-side difference in the posterior drawer test of 2.9 (± 2.2) mm (preoperative 13.3 [± 1.9] mm).
Conclusion
Low complication risk and good and excellent clinical results after arthroscopic posterolateral corner reconstruction.
Zusammenfassung
Operationsziel
Entwicklung einer neuen arthroskopischen Technik zur kombinierten Rekonstruktion der posterolateralen Ecke und des hinteren Kreuzbands (HKB).
Indikationen
Posterolaterale Rotationsinstabilitäten des Kniegelenks. Kombinierte Läsionen des HKB, des Popliteuskomplexes (PLT) und der posterolateralen Ecke. Isolierte PLT-Läsionen mit posterolateraler Instabilität.
Kontraindikationen
Neuromuskuläre Störungen, Kniedeformitäten und -frakturen, schwere Weichteilschäden in der posterolateralen Region.
Operationstechnik
Notwendig sind 6 arthroskopische Portale. Über das posteromediale Portal wird das dorsale Septum reseziert und HKB sowie posterolateraler Rezessus mit dem PLT dargestellt. Am Hiatus popliteus werden popliteomeniskale Fasern durchtrennt, die Popliteussehne aus dem Sulcus luxiert und der distale Anteil des Sulcus popliteus dargestellt. Bohren eines 6-mm-Bohrkanals von ventral in das distale Drittel des Sulcus popliteus. Der femorale Popliteussehnenansatz wird dargestellt und ein anatomischer femoraler Bohrkanal gesetzt. Einziehen des Grazilissehnentransplantats als „Popliteus Bypass Graft“ und Fixation mit Biotenodeseschrauben. Fixation des HKB-Transplantats. Bei einer LCL-Instabilität zusätzliche Rekonstruktion des LCL.
Postoperative Behandlung
Bodenkontaktbelastung für 6 Wochen, Orthese mit Bewegungslimitierung für 3 Monate, Quadrizepskräftigungsübungen direkt postoperativ. Sofort volle Streckung, sukzessive Beugungsfreigabe bis 90° über 6 Wochen. Joggen oder tiefe Kniebeugen frühestens nach 3 Monaten.
Ergebnisse
Keine technikspezifischen Komplikationen bei 35 behandelten Patienten. Nach 1 Jahr hatten 12 Patienten einen mittleren Lysholm-Score von 88,6 (± 8,7) Punkten und eine radiologisch gemessene dorsale Instabilität im Seitenvergleich von 2,9 (± 2,2) mm (präoperativ 13,3 [± 1,9] mm).
Schlussfolgerung
Niedrige Komplikationsraten und gute erste klinische Ergebnisse nach arthroskopischer Rekonstruktion der posterolateralen Ecke.
Similar content being viewed by others
Introductory remarks
The anatomy of the knee is complex, and particularly that of the posterolateral corner ([8]; Fig. 1). The popliteus tendon complex has a static and a dynamic function. The popliteus muscle–tendon (PLT) itself acts in a dynamic function as an active internal rotator of the tibia and adjusts the postural equilibrium during standing [14]. The static biomechanical function of resistance against passive external rotation of the tibia is achieved in combination with the arcuate complex (AC; [11]). The AC mainly comprises the popliteofibular ligament, the fabellofibular ligament, popliteomeniscal fibers, and multiple extensions of the popliteus tendon to the tibia and to the posterior capsule (Fig. 1). Thereby, the AC represents the primary static stabilizer to external rotation [10, 15, 21]. The most prominent structure of the AC is the popliteofibular ligament (Fig. 1, 2a, b).
Dorsal anatomy of the right knee of a human cadaver with the posterolateral corner, consisting out of the lateral collateral ligament (LCL), the popliteus complex, and the posterolateral capsule. The popliteus complex is created by the popliteus tendon and the arcuate complex (AC). The most prominent structure of the AC is the popliteofibular ligament. This ligament mainly secures the static stabilizing function of the popliteus muscle–tendon complex (PLT)
Lateral anatomy of the right knee of a human cadaver in a extension and b 90° of flexion. The femoral footprint of the popliteus muscle–tendon is on average 1.2 cm distal of the femoral footprint of the lateral collateral ligament (distance center to center) [2]
The great importance of the AC for stabilization of the tibia against external rotation especially in flexion has been described previously [10, 15, 17]. If the AC is injured, primary posterior translation and coupled external rotation [13, 21] increases. With an isolated injury of the posterior cruciate ligament (PCL), a posterior instability of up to 10 mm in 90° of flexion results [16]. Additional dissection of the PLT results in a dorsal instability of up to 15 mm in the posterior drawer test in 90° of flexion. These biomechanical results indicate that a dorsal instability of more than 10 mm in 90° of flexion results in a combined posterolateral rotational instability [16]. Up to 70 % of all PCL injuries are combined injuries with additional lesions of the posterolateral corner [8, 16].
For an exact analysis of the kind of instability (dorsal, lateral, rotational, posterolateral, or combined), it has to be considered that the main constraint against tibial external rotation from 0 to 30° is the LCL, while the arcuate complex becomes dominant towards increasing flexion, exhibiting its main function at 90° of flexion [3, 5, 9]. In addition, the LCL is the main stabilizer against varus stress in 0–30° extension. In this study, patients with a posterolateral rotational instability including a posterior drawer of more than 10 mm underwent reconstruction of the popliteus complex with a popliteus bypass graft in combination with PCL reconstruction. LCL was additionally reconstructed only if a lateral instability in 10° of flexion was evident.
The first anatomical reconstruction of the popliteus complex with an anatomical popliteus bypass graft was described by Werner Müller in 1982 [12]. Thereafter, numerous surgical techniques to reconstruct the static stabilizing function of the PLT have been described [1, 4, 6, 7, 18, 20, 22, 23]. Most of these are extraanatomical techniques with limited capacity to stabilize the posterolateral corner. With anatomical techniques for the reconstruction of the posterolateral corner, good and excellent results have been described [9, 19]. However, the described techniques are basically open surgical procedures, without the advantages of an arthroscopic technique.
We therefore developed a novel arthroscopic procedure for anatomic reconstruction of the popliteus complex with a popliteus bypass graft [2]. In this paper, the operative technique is presented in detail.
Surgical principles and objectives
The goal of the surgical procedure is to regain the static stabilizing function of the popliteus complex. The dynamic stabilizing function of the popliteus complex should thereby be preserved. These goals should be achieved by an arthroscopic procedure with exact and anatomic tunnel placement [2].
Advantages
-
Restoration of the anatomy and biomechanics of the knee by anatomical reconstruction
-
Proper visualization of anatomical landmarks, which is not possible with open techniques
-
Utilization of small incisions with a greater likelihood of lower infection rates, lower rates of scar tissue formation, less postoperative pain, faster rehabilitation, and more aesthetic incisions
-
Preparation and visualization of the peroneal nerve are not necessary
Disadvantages
-
Requires advanced arthroscopic skills
-
Requires experience in PCL and PLT surgery due to the demanding technique
-
The use of special instruments is strongly recommended (i. e., tibial drill guide)
-
A flat learning curve
Indications
-
Posterolateral rotational instabilities of the knee joint
Contraindications
-
Fixed dorsal position of the tibia (i. e., after ACL reconstruction)
-
Systemic diseases like rheumatoid arthritis, autoimmune diseases, etc.
-
Neuromuscular disorders
-
Anatomic deformities and acute fractures around the knee
-
Obesity (relative)
Patient information
-
General risk factors related to arthroscopic surgery: infection, complex regional pain syndrome, deep vein thrombosis, pulmonary embolism, neurovascular iatrogenic injuries, failure
-
Duration of hospital stay: 3–4 days
-
Persistent instability
-
Arthrofibrosis with limited range of motion
-
Possible development of degenerative joint disease over time
-
Graft harvesting from the contralateral side
-
Possibility of iatrogenic damage to the infrapatellar branch of the saphenous nerve or the peroneal nerve
-
Prolonged rehabilitation protocol: full extension is allowed immediately, flexion is limited, brace for 3 months (i. e., Jack PCL, Albrecht, Munich, Germany)
-
Clinical assessment at 3, 6, 9, and 12 months
-
Surgical failure may require another open procedure
-
Running and squatting exercises are allowed after 3 months
-
High-level sports may commence 6–9 months after surgery
-
Return to work/sports activities are dependent on the type of work/sports
Preoperative and diagnostic work-up
-
Patient history
-
Clinical assessment with posterior drawer and Dial tests
-
Anterior and medial instability should be ruled out
-
Lateral stability test in full extension (LCL) and 10° and 90° of flexion
-
External rotation test at 30, 60, and 90° in comparison to the contralateral side
-
Brace test (optional, to test whether patient’s symptoms improve by using a PCL brace)
-
Fixed dorsal drawer should be ruled out
-
MRI assessment of the knee
-
Anterior–posterior, lateral, and long x-ray views (in clinically suspected cases of axis deviation)
-
Stress x-rays with anterior and posterior drawer of both knees (Fig. 3)
-
Preoperative management to assure good range of motion (> 0–0–100°)
-
Intensive quadriceps strengthening preoperatively
-
Side which is planned for operation should be marked prior to surgery
Surgical instruments and implants
-
Arthroscopic instruments: hook, grasper, shaver (4 mm blade, not too sharp), radiofrequency electrode, guide wires, tendon harvester, drill bits in different sizes (6–10 mm), WORM (Arthrex, Naples, FL, USA)
-
Drill guide for PCL reconstruction and a special drill guide for arthroscopic posterolateral corner reconstruction (Tibial Popliteal Marking Hook, Arthrex, Naples, FL, USA)
-
Biointerference screws for graft fixation in different diameters (5–9 mm) (Milagro, DePuy Mitek, Norderstedt, Germany or Swivelock, Arthrex, Naples, FL, USA, etc.)
Anesthesia and positioning
-
General or spinal anesthesia
-
Supine position
-
Non-sterile thigh tourniquet
-
Electrical leg holder (Maquet, Germany; Fig. 4)
Surgical technique
(Figs. 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16)
For arthroscopic popliteus reconstruction, the following six arthroscopic portals are necessary: a low and a high anterolateral, a high anteromedial, a posteromedial, a posterolateral, and a lateral portal. After diagnostic arthroscopy hamstring tendons from the ipsilateral side (semitendinosus and gracilis tendon for the posterior cruciate ligament [PCL] graft) and a gracilis tendon from the contralateral side for the popliteus bypass graft are harvested in a typical manner. For the popliteus bypass graft a double-stranded graft (11–12 cm long) is used
a Arthroscopic view from posteromedial portal in a right knee and b sketch of setup: Torn fibers of the posterior cruciate ligament (PCL; red arrow), the lateral femoral condyle, the dorsal septum (partially resected) and the popliteus tendon (green arrow) are exposed. A posterolateral portal was installed under visual control. Care must be taken to remain anterior of the biceps tendon to avoid injury to the peroneal nerve. b The schematic drawing shows a torn PCL and a ruptured popliteofibular ligament (classified as a posterolateral corner injury type A according to Fanelli)
Exposure of the popliteus tendon by resection of popliteomeniscal fibers with a radiofrequency electrode through a posterolateral portal. Care should be taken not to injure the popliteus tendon. If a radiofrequency electrode is used for dissection of the popliteomeniscal fibers, care should be taken not to injure the cartilage at the posterolateral tibial plateau. Customarily, only the lateral popliteomeniscal fibers must be dissected along a length of 1–2 cm
The popliteus tendon (green arrow) is retracted with a hook and the sulcus popliteus (red arrow) can be visualized. The arthroscope enters from posteromedial (right knee). The arcuate complex is observed to be wrapped onto the tendon, leading to a loss of the static stabilizing function of the popliteus tendon. In such cases, the popliteus tendon may be easily retracted to expose the sulcus
a The proper location of the tibial drill channel for the popliteus bypass graft is at the crossing of a horizontal line at the tip of the fibular head with a vertical line at the medial edge of the fibular head. b A special drill guide (through the anteromedial portal; Tibial Popliteal Marking Hook”, Arthrex, Naples, FL, USA) is positioned in the distal third of the sulcus popliteus. c A useful technique to ensure correct tibial tunnel placement is to palpate the fibular head with the tip of the drill guide and to position the center of the tip of the drill guide 5–7 mm below the cranial edge of the popliteus tendon. A guide wire is positioned in the distal part of the sulcus popliteus. The anterior start point of the drill guide is positioned between the lateral edge of the tibial tuberosity and the medial edge of Gerdy’s tubercle. The tibial tunnel was drilled with a 6-mm cannulated drill. It has been shown that the presented arthroscopic technique is highly accurate and reliable [2]. Therefore, intraoperative fluoroscopy to check the location of the tunnel is optional
a For anatomic placement of the femoral tunnel, the arthroscope was introduced in the high anterolateral portal. At 20–30° of knee flexion, a shaver blade (which should not be too aggressive) is inserted in a dorsocaudal direction through a lateral parapatellar portal and directly placed 1 cm dorsal to the craniolateral edge of the patella to expose the femoral origin of the popliteus tendon. For optimal visualization of the femoral footprint of the popliteus tendon, anterior and distal fibers of the knee capsule at the lateral femoral condyle must be resected. b An arthroscopic view through the anterolateral portal at the femoral footprint of the popliteus tendon (right knee) is shown. The tendon is retracted with a hook to expose the femoral footprint. Percutaneously, a 2.3-mm guide wire is placed directly in the femoral footprint of the popliteus tendon. The femoral tunnel is drilled with a 5-mm drill
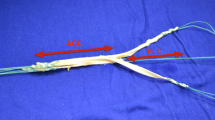
a Arthroscopic view from posteromedial portal (right knee) and b sketch of procedure. A suture loop is inserted in the posterolateral recessus through the tibial tunnel (green arrow) as a shuttle for the popliteus bypass graft. Then, a bent suture grasper is inserted through the lateral incision for the installation of the femoral tunnel and is advanced into the posterolateral recessus along the popliteus tendon (red arrow) to grasp the suture loop. Care must be taken not to interpose soft tissue between the shuttle loop and the femoral drill tunnel
a Arthroscopic view from anterolateral (right knee) and b sketch of procedure. The popliteus bypass graft (single-stranded semitendinosus or double-stranded gracilis tendon, green arrow) is pulled through the tibial tunnel in the femoral tunnel. Care must be taken to assure that the graft is located under the lateral collateral ligament (LCL; seen in the image directly dorsal to the guide wire for the cannulated bioscrew, red arrow)
Arthroscopic view (right knee) from a, b posteromedial and c anterolateral/intraarticular portals. The popliteus bypass graft (red arrow) is located under the popliteus tendon (green arrow) in the sulcus popliteus. The fixation of the graft is performed at first at the femoral side with a bioscrew (diameter 5 mm). The screw is percutanously implanted through a nithinol guidewire
Arthroscopic view from anterolateral. The posterior cruciate ligament (PCL) graft is visualized. After reconstruction and fixation of the PCL, the popliteus bypass graft is fixed at the tibial side with a bioscrew (diameter 6 mm). During fixaton the knee is flexed 90° and 10–20° internally rotated. The LCL needs to be additionally reconstructed only if a lateral instability in 10° of flexion is evident (classified as a posterolateral corner injury type B or C according to Fanelli)
Postoperative management
-
Wound dressing until postoperative day 2
-
Partial weight-bearing (10–20 kg) for 6 weeks
-
PCL brace for 3 months (i. e., Jack PCL, Albrecht, Unterschleißheim, Germany) with limited range of motion 0–0–20° for 2 weeks, 0–0–45° for 2 weeks and 0–0–60° for further 2 weeks. 0–0–90° until week 8 and then free range of motion.
-
Range-of-motion exercises in the prone position and passive flexion against quadriceps contraction up to 60° allowed from postoperative day 1
-
Quadriceps strengthening exercises are allowed from postoperative day 1
-
Active knee flexion is not allowed for the first 6 weeks postoperatively
-
Proprioception loading exercises should be included
-
Running and squatting exercises are begun after 3 months from the index procedure
Results
To date, 35 patients have received a popliteus bypass graft due to a posterolateral rotational instability in combination with a PCL reconstruction. No intra- or postoperative complications have been observed so far. After 1 year, 12 patients (6 women) were examined (study still continuing). The mean age was 35.3 (± 13.6) years with a mean body mass index of 27.1 (± 3.6). The mean time from trauma to surgery was 11 (3–42) weeks. Among all patients who underwent surgery as described above, 3 patients received an additional LCL reconstruction, 1 patient underwent an additional ACL reconstruction, 1 patient had an additional high tibial osteotomy due to 7° of varus deformity (one-stage procedure), and 1 patient had an additional torsional osteotomy of the femur due to torsional deformity after femoral shaft fracture (two-stage procedure). The mean postoperative Lysholm Score was 88.4 (± 8.7) points, whereas the mean Tegner Score was preoperatively 5.6 (± 1.8) and 4.9 (± 1.0) points during follow-up. The Visual Analog Scale function was 2.8 (± 1.5; 0 complete function, 10 no function) and the Visual Analog Scale pain was 1.9 (± 1.8; 0 no pain, 10 maximal pain). In the preoperative stress x-rays with the Telos device, the mean side-to-side difference in the posterior drawer test in 90° of flexion was −13.3 (± 1.9) mm and postoperatively the mean side-to-side difference was −2.9 (± 2.2) mm. The Dial Test was negative in 10 of 12 patients.
The arthroscopic technique of posterolateral corner reconstructions has a low complication rate and leads to good and excellent clinical results.
References
Apsingi S, Nguyen T, Bull AM, Unwin A, Deehan DJ, Amis AA (2009) A comparison of modified Larson and “anatomic” posterolateral corner reconstructions in knees with combined PCL and posterolateral corner deficiency. Knee Surg Sports Traumatol Arthrosc 17(3):305–312
Frosch KH, Akoto R, Maximilian H, Enderle E, Giannakos A, Preiss A (2014) Arthroscopic reconstruction of the popliteus complex: accuracy and reproducibility of a new surgical technique. Knee Surg Sports Traumatol Arthrosc2015 Oct;23(10):3114-20.
Harner CD, Höher J, Vogrin TM, Carlin GJ, Woo SL (1998) The effects of a popliteus muscle load on in situ forces in the posterior cruciate ligament and on knee kinematics. A human cadaveric study. Am J Sports Med 26(5):669–673
Hefti F, Muller W, Jakob RP, Staubli HU (1993) Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc 1(3–4):226–234
Höher J, Harner CD, Vogrin TM, Baek GH, Carlin GJ, Woo SL (1998) In situ forces in the posterolateral structures of the knee under posterior tibial loading in the intact and posterior cruciate ligament-deficient knee. J Orthop Res 16(6):675–681
Jung YB, Jung HJ, Kim SJ, Park SJ, Song KS, Lee YS, Lee SH (2008) Posterolateral corner reconstruction for posterolateral rotatory instability combined with posterior cruciate ligament injuries: comparison between fibular tunnel and tibial tunnel techniques. Knee Surg Sports Traumatol Arthrosc 16(3):239–248
Khanduja V, Somayaji HS, Harnett P, Utukuri M, Dowd GS (2006) Combined reconstruction of chronic posterior cruciate ligament and posterolateral corner deficiency. A two- to nine-year follow-up study. J Bone Joint Surg Br 88(9):1169–1172
LaPrade RF (2006) Posterolateral knee injuries: anatomy, evaluation, and treatment. History of the nomenclature and study of the anatomy of the posterolateral knee. Thieme, New York
LaPrade RF, Johansen S, Wentorf FA, Engebretsen L, Esterberg JL, Tso A (2004) An analysis of an anatomical posterolateral knee reconstruction: an in vitro biomechanical study and development of a surgical technique. Am J Sports Med 32(6):1405–1414
LaPrade RF, Wozniczka JK, Stellmaker MP, Wijdicks CA (2010) Analysis of the static function of the popliteus tendon and evaluation of an anatomic reconstruction: the “fifth ligament” of the knee. Am J Sports Med 38(3):543–549
McCarthy M, Camarda L, Wijdicks CA, Johansen S, Engebretsen L, Laprade RF (2010) Anatomic posterolateral knee reconstructions require a popliteofibular ligament reconstruction through a tibial tunnel. Am J Sports Med 38(8):1674–1681
Müller W (1981) Das Knie – Form, Funktion und ligamentäre Wiederherstellungschirurgie. Springer, Berlin, Heidelberg, New York, p 273
Nau T, Chevalier Y, Hagemeister N, Deguise JA, Duval N (2005) Comparison of 2 surgical techniques of posterolateral corner reconstruction of the knee. Am J Sports Med 33(12):1838–1845
Nyland J, Lachman N, Kocabey Y, Brosky J, Altun R, Caborn D (2005) Anatomy, function, and rehabilitation of the popliteus musculotendinous complex. J Orthop Sports Phys Ther 35(3):165–179
Pasque C, Noyes FR, Gibbons M, Levy M, Grood E (2003) The role of the popliteofibular ligament and the tendon of popliteus in providing stability in the human knee. J Bone Joint Surg Br 85(2):292–298
Petersen W, Zantop T (2006) Biomechanik des hinteren Kreuzbands und der hinteren Instabilität. Arthroskopie 19:207–214
Sekiya JK, Whiddon DR, Zehms CT, Miller MD (2008) A clinically relevant assessment of posterior cruciate ligament and posterolateral corner injuries. Evaluation of isolated and combined deficiency. J Bone Joint Surg Am 90(8):1621–1627
Spiridonov SI, Slinkard NJ, LaPrade RF (2011) Isolated and combined grade-III posterior cruciate ligament tears treated with double-bundle reconstruction with use of endoscopically placed femoral tunnels and grafts: operative technique and clinical outcomes. J Bone Joint Surg Am 93(19):1773–1780
Stannard JP, Brown SL, Robinson JT, McGwin G Jr, Volgas DA (2005) Reconstruction of the posterolateral corner of the knee. Arthroscopy 21(9):1051–1059
Strobel MJ, Schulz MS, Petersen WJ, Eichhorn HJ (2006) Combined anterior cruciate ligament, posterior cruciate ligament, and posterolateral corner reconstruction with autogenous hamstring grafts in chronic instabilities. Arthroscopy 22(2):182–192
Thaunat M, Pioger C, Chatellard R, Conteduca J, Khaleel A, Sonnery-Cottet B (2014) The arcuate ligament revisited: role of the posterolateral structures in providing static stability in the knee joint. Knee Surg Sports Traumatol Arthrosc 22(9):2121–2127
Wajsfisz A, Christel P, Djian P (2010) Does combined posterior cruciate ligament and posterolateral corner reconstruction for chronic posterior and posterolateral instability restore normal knee function? Orthop Traumatol Surg Res 96(4):394–399
Zantop T, Petersen W (2010) Modified Larson technique for posterolateral corner reconstruction of the knee. Oper Orthop Traumatol 22(4):373–386
Acknowledgement
The study was supported by grant (number 2764) from Asklepios proresearch, Hamburg, Germany.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
R. Akoto, T. Drenck, M. Heitmann, C. Pahl, and A. Preiss state that there are no conflicts of interest. The operation technique was developed on human cadaver specimens in cooperation with Arthrex, Naples, USA. K.-H. Frosch received grants from Arthrex, Naples, USA.
The study was approved by the Ethics Committee of the Hamburg Chamber of Physicians and was carried out according to existing rules and regulations of the Asklepios Campus Hamburg, Semmelweis University Budapest (PV4458).
Additional information
Redaktion
W. Petersen, Berlin
Zeichner
J. Kühn, Mannheim
Rights and permissions
Open Access . This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Frosch, KH., Akoto, R., Drenck, T. et al. Arthroscopic popliteus bypass graft for posterolateral instabilities of the knee. Oper Orthop Traumatol 28, 193–203 (2016). https://doi.org/10.1007/s00064-015-0432-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00064-015-0432-6