Abstract
Background
The aim of this study was to investigate the effects of thin-cap fibroatheromas (TCFAs) on stent neointimal coverage at the 9‑month follow-up after EXCEL stent implantation assessed by optical coherence tomography (OCT).
Methods
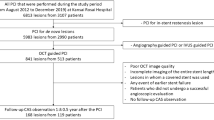
A total of 93 patients with non-ST elevation acute coronary syndrome (NSTEACS) who underwent EXCEL stent implantation were prospectively enrolled in the study and divided into a TCFA group (n = 47) and a non-TCFA group (n = 46) according to whether EXCEL stents covered the TCFAs. A TCFA was defined as a plaque with lipid content in more than one quadrant and fibrous cap thickness measuring less than 65 μm. The effect of TCFAs on stent neointimal coverage at the 9‑month follow-up after stent implantation was evaluated by OCT. The primary study endpoints were the incidence of neointimal uncoverage and stent malapposition.
Results
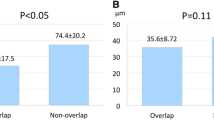
At the 9‑month follow-up, the minimal lumen diameter of the TCFA group tended to be smaller (2.8 ± 0.8 vs. 2.1 ± 0.8, p = 0.08) and the diameter of stenosis in the TCFA group tended to be larger (15.1 ± 10.3% vs. 26.3 ± 15.1%, p = 0.08) than those in the non-TCFA group. The mean intimal thickness of the TCFA group was significantly lower than that of the non-TCFA group (67.2 ± 35.5 vs. 145.1 ± 48.7, p < 0.001). The uncovered struts (10.1 ± 9.7 vs. 4.8 ± 4.3, p = 0.05) and malapposed struts (2.1 ± 4.7 vs. 0.3 ± 0.5, p = 0.003) in the TCFA group were more significant than those in the non-TCFA group. Multivariate analysis showed that TCFAs and lesion types were independent predictors of incomplete neointimal coverage (p < 0.05), and lesion types were independent predictors of stent malapposition (p < 0.05).
Conclusion
In patients with NSTEACS, TCFAs delayed endothelium coverage at 9 months after stent implantation, and TCFAs were independent predictors of incomplete neointimal coverage of the stent.
Zusammenfassung
Ziel
Mittels optischer Kohärenztomographie (OCT) sollten die Auswirkungen von Fibroatheromen mit dünner Endothelschicht (TCFA) auf die neointimale Abdeckung von Stents bei der 9‑Monats-Nachuntersuchung nach EXCEL-Stentimplantation untersucht werden.
Methoden
Prospektiv wurden 93 Patienten mit akutem Koronarsyndrom ohne ST-Hebung, die eine EXCEL-Stentimplantation erhielten, in die TCFA-Gruppe (n = 47) und die Nicht-TCFA-Gruppe (n = 46) eingeteilt, je nachdem, ob EXCEL-Stents TCFA bedeckten. Ein TCFA wurde als Plaque mit Lipidgehalt in > 1 Quadranten und einer Dicke der Faserkappe von weniger als 65 µm definiert. Die Wirkung von TCFA auf die neointimale Abdeckung der Stents bei der Nachuntersuchung nach 9 Monaten nach der Stentimplantation wurde mittels OCT bewertet. Die primären Studienendpunkte waren die Inzidenz der Feststellung einer Neointima und einer Stent-Fehlpositionierung.
Ergebnisse
Bei der Nachuntersuchung nach 9 Monaten war der minimale Lumendurchmesser der TCFA-Gruppe tendenziell kleiner (2,8 ± 0,8 vs. 2,1 ± 0,8; p = 0,08) und der Durchmesser der Stenose in der TCFA-Gruppe tendenziell größer (15,1 ± 10,3 % vs. 26,3 ± 15,1 %; p = 0,08) als in der Nicht-TCFA-Gruppe. Die mittlere Intimadicke der TCFA-Gruppe war signifikant geringer als die der Nicht-TCFA-Gruppe (67,2 ± 35,5 vs. 145,1 ± 48,7; p < 0,001). Die unbedeckten Streben (10,1 ± 9,7 vs. 4,8 ± 4,3; p = 0,05) und die fehlangelegten Streben (2,1 ± 4,7 vs. 0,3 ± 0,5; p = 0,003) in der TCFA-Gruppe waren signifikanter als die in der Nicht-TCFA-Gruppe. Die multivariate Analyse zeigte, dass TCFA und Läsionstypen unabhängige Prädiktoren für eine unvollständige neointimale Abdeckung (p < 0,05) und Läsionstypen unabhängige Prädiktoren für eine Stent-Fehlpositionierung (p < 0,05) waren.
Schlussfolgerung
Bei Patienten mit akutem Koronarsyndrom ohne ST-Hebung verzögerten TCFA die Endothelabdeckung 9 Monate nach der Stentimplantation, und TCFA waren unabhängige Prädiktoren für eine unvollständige neointimale Abdeckung des Stents.

Similar content being viewed by others
References
Garg S, Bourantas C, Serruys PW (2013) New concepts in the design of drug-eluting coronary stents. Nat Rev Cardiol 10(5):248–260
Minha S, Pichard AD, Waksman R (2013) In-stent restenosis of drug-eluting stents. Future Cardiol 9(5):721–731
Finn AV, Joner M, Nakazawa G et al (2007) Pathological correlates of late drug-eluting stent thrombosis: strut coverage as a marker of endothelialization. Circulation 115(18):2435–2441
Zhang L, Wahle A, Chen Z et al (2018) Predicting locations of high-risk plaques in coronary arteries in patients receiving statin therapy. IEEE Trans Med Imaging 37(1):151–161
Cheng JM, Garcia-Garcia HM, de Boer SP et al (2014) In vivo detection of high-risk coronary plaques by radiofrequency intravascular ultrasound and cardiovascular outcome: results of the ATHEROREMO-IVUS study. Eur Heart J 35(10):639–647
Iannaccone M, Quadri G, Taha S, et al (2016) Prevalence and predictors of culprit plaque rupture at OCT in patients with coronary artery disease: a meta-analysis. Eur Heart J Cardiovasc Imaging 17 (10):1128-1137.
Kimura S, Sugiyama T, Hishikari K et al (2016) Impact of optical coherence tomography- and coronary angioscopy-assessed neointimal tissue characteristics on occurrence of periprocedural myonecrosis in patients with in-stent restenosis. Int J Cardiovasc Imaging 32(10):1483–1494
Raber L, Mintz GS, Koskinas KC et al (2018) Clinical use of intracoronary imaging. Part 1: guidance and optimization of coronary interventions. An expert consensus document of the European association of percutaneous cardiovascular interventions. Eur Heart J 39(35):3281–3300
Leone AM, Rebuzzi AG, Burzotta F et al (2019) Stent malapposition, strut coverage and atherothrombotic prolapse after percutaneous coronary interventions in ST-segment elevation myocardial infarction. J Cardiovasc Med (Hagerstown) 20(3):122–130
Im E, Lee SY, Hong SJ et al (2019) Impact of late stent malapposition after drug-eluting stent implantation on long-term clinical outcomes. Atherosclerosis 288:118–123
Stone GW, Maehara A, Lansky AJ et al (2011) A prospective natural-history study of coronary atherosclerosis. N Engl J Med 364(3):226–235
Torii S, Nakazawa G, Ijichi T et al (2018) Comparison of the endothelial coverage in everolimus and zotarolimus-eluting stents in normal, atherosclerotic, and bifurcation rabbit iliac arteries. Cardiovasc Interv Ther 33(1):55–61
Poerner TC, Otto S, Gassdorf J et al (2011) A prospective randomised study using optical coherence tomography to assess endothelial coverage and neointimal proliferation at 6‑months after implantation of a coronary everolimus-eluting stent compared with a bare metal stent postdilated with a paclitaxel-eluting balloon (OCTOPUS Trial): rationale, design and methods. EuroIntervention 7:K93–99
Won H, Kim JS, Shin DH et al (2014) Relationship between endothelial vasomotor function and strut coverage after implantation of drug-eluting stent assessed by optical coherence tomography. Int J Cardiovasc Imaging 30(2):263–270
Baumbach A, Lansky AJ, Onuma Y et al (2018) Optical coherence tomography substudy of a prospective multicentre randomised post-market trial to assess the safety and effectiveness of the firehawk cobalt-chromium coronary stent (rapamycin target-eluting) system for the treatment of atherosclerotic lesions: TARGET all comers. EuroIntervention 14(10):1121–1128
Han Z, Feng L, Du H et al (2015) Impact of age on stent strut coverage and neointimal remodeling as assessed by optical coherence tomography. Medicine 94(50):e2246
Nakata T, Fujii K, Fukunaga M et al (2016) Morphological, functional, and biological vascular healing response 6 months after drug-eluting stent implantation: a randomized comparison of three drug-eluting stents. Catheter Cardiovasc Interv 88(3):350–357
Tang L, Cui QW, Liu DP et al (2019) The number of stents was an independent risk of stent restenosis in patients undergoing percutaneous coronary intervention. Medicine 98(50):e18312
Valgimigli M, Tebaldi M, Borghesi M et al (2014) Two-year outcomes after first- or second-generation drug-eluting or bare-metal stent implantation in all-comer patients undergoing percutaneous coronary intervention: a pre-specified analysis from the PRODIGY study (PROlonging Dual Antiplatelet Treatment After Grading stent-induced Intimal hyperplasia studY). JACC Cardiovasc Interv 7(1):20–28
Xu K, Han Y, Xu B et al (2018) Efficacy and safety of a second-generation biodegradable polymer sirolimus-eluting stent: one-year results of the CREDIT 2 trial. Cardiovasc Ther 36(3):e12327
Jin ZG, Liu HL, Luo JP et al (2011) Long-term effects of biodegradable versus durable polymer-coated sirolimus-eluting stents on coronary arterial wall morphology assessed by virtual histology intravascular ultrasound in patients with acute coronary syndrome. Heart 97(3):A166–A166
Kubo T, Maehara A, Mintz GS et al (2010) Analysis of the long-term effects of drug-eluting stents on coronary arterial wall morphology as assessed by virtual histology intravascular ultrasound. Am Heart J 159(2):271–277
Prati F, Di Vito L, Biondi-Zoccai G et al (2012) Angiography alone versus angiography plus optical coherence tomography to guide decision-making during percutaneous coronary intervention: the Centro per la Lotta contro l’Infarto-optimisation of percutaneous coronary intervention (CLI-OPCI) study. EuroIntervention 8(7):823–829
Kim BK, Shin DH, Kim JS et al (2012) Optical coherence tomography-based evaluation of malapposed strut coverage after drug-eluting stent implantation. Int J Cardiovasc Imaging 28(8):1887–1894
Guagliumi G, Costa MA, Sirbu V et al (2011) Strut coverage and late malapposition with paclitaxel-eluting stents compared with bare metal stents in acute myocardial infarction: optical coherence tomography substudy of the harmonizing outcomes with revascularization and stents in acute myocardial infarction (HORIZONS-AMI) trial. Circulation 123(3):274–281
Farb A, Burke AP, Kolodgie FD et al (2003) Pathological mechanisms of fatal late coronary stent thrombosis in humans. Circulation 108(14):1701–1706
Kubo T, Imanishi T, Kitabata H et al (2008) Comparison of vascular response after sirolimus-eluting stent implantation between patients with unstable and stable angina pectoris: a serial optical coherence tomography study. JACC Cardiovasc Imaging 1(4):475–484
Funding
This work was supported by the Beijing Municipal Science and Technology Project (Z161100000516091).
Author information
Authors and Affiliations
Contributions
J. Zhang, Y. Duan, H. Yu, and H. Liu were involved in the study conception and design, data acquisition, and data analysis. J. Zhang and Y. Duan drafted the manuscript. H. Yu and H. Liu revised the manuscript. L. Jing, Y. Li, X. Jia and D. Jin were involved in the analysis or interpretation of data. All authors read and approved the final manuscript. All authors gave final approval for this version to be published.
Corresponding author
Ethics declarations
Conflict of interest
J. Zhang, Y. Duan, H. Yu, L. Jing, Y. Li, X. Jia, D. Jin, and H. Liu declare that they have no competing interests.
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Ethics Committee of the Third Medical Center of Chinese PLA General Hospital, and written informed consent was obtained from all individual participants included in the study.
Additional information
J. Zhang, Y. Duan, and H. Yu contributed equally to this work.
Availability of data and material
The data used to support the findings of this study are available from the corresponding author upon request.
Rights and permissions
About this article
Cite this article
Zhang, J., Duan, Y., Yu, H. et al. Effects of TCFA on stent neointimal coverage at 9 months after EXCEL drug-eluting stent implantation assessed by OCT. Herz 48, 64–71 (2023). https://doi.org/10.1007/s00059-021-05095-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-021-05095-2
Keywords
- Optical coherence tomography
- Non-ST-elevation acute coronary syndrome
- Thin-cap fibroatheroma
- Neointimal coverage
- Malapposition