Abstract
Background
The study aimed to evaluate the prognostic impact of postdischarge care fragmentation in patients undergoing transcatheter aortic valve replacement (TAVR).
Methods
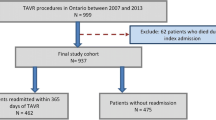
A total of 266 patients undergoing TAVR due to severe aortic stenosis were included in this retrospective cohort study. Patients were assigned to one of two groups based on presence (n = 104) and absence (n = 162) of postdischarge care fragmentation. Fragmented care was defined as at least one readmission to a site other than the implanting TAVR center within 90 days. Prognostic impact of care fragmentation on clinical outcomes and predictors of long-term mortality were investigated.
Results
Increased major vascular complication (16.3 vs 8.0%, p = 0.037), permanent pacemaker implantation (14.4 vs 6.2%, p = 0.025), and acute kidney injury (22.1 vs 14.2%, p < 0.001) were reported in the fragmented care group. Although early mortality (6.7 vs 4.3%, p = 0.152) was similar between groups, there was a significant difference in 5‑year mortality (66.3 vs 45.7%, p < 0.001). In a univariate regression analysis fragmented care, age, chronic obstructive pulmonary disease, pulmonary artery systolic pressure, and paravalvular leakage were significantly associated with 5‑year mortality. Fragmented care (hazard ratio [HR] 1.510, 95% confidence interval [CI] 1.080–2.111; p = 0.016), age (HR 1.024, 95% CI 1.001–1.048; p = 0.045), paravalvular leakage (HR 1.863, 95% CI 1.076–3.228; p = 0.026), and chronic obstructive pulmonary disease (HR 1.616, 95% CI 1.114–2.344; p = 0.012) were found to be significant independent predictors of 5‑year mortality in a multivariate analysis, after adjusting for other risks.
Conclusion
Fragmented care has a significant prognostic impact on clinical outcomes and survival.
Zusammenfassung
Hintergrund
Ziel der Studie war es, die prognostischen Auswirkungen der Fragmentierung der Nachsorge bei Patienten zu untersuchen, die sich einem transkathetergestützten Aortenklappenersatz (TAVR) unterziehen.
Methoden
Insgesamt 266 Patienten, die sich aufgrund einer schweren Aortenstenose einer TAVR unterzogen haben, wurden in diese retrospektive Kohortenstudie eingeschlossen. Die Patienten wurden aufgrund des Vorhandenseins (n = 104) und des Fehlens (n = 162) einer Fragmentierung der Betreuung nach der Entlassung in 2 Gruppen eingeteilt. Fragmentierte Versorgung wurde definiert als mindestens eine Wiederaufnahme an einem anderen Ort als dem implantierenden TAVR-Zentrum innerhalb von 90 Tagen. Die prognostischen Auswirkungen der Fragmentierung der Versorgung auf die klinischen Ergebnisse und die Prädiktoren der Langzeitmortalität wurden untersucht.
Ergebnisse
In der Gruppe mit fragmentierter Versorgung wurde über eine erhöhte Anzahl schwerer vaskulärer Komplikationen (16,3 vs. 8,0%, p = 0,037), die Implantation eines permanenten Schrittmachers (14,4 vs. 6,2%, p = 0,025) und eine akute Nierenverletzung (22,1 vs. 14,2%; p < 0,001) berichtet. Obwohl die frühe Mortalität (6,7 vs. 4,3%; p = 0,152) zwischen den Gruppen ähnlich war, gab es einen signifikanten Unterschied in der 5‑Jahres-Mortalität (66,3 vs. 45,7%, p < 0,001). In einer univariaten Regressionsanalyse waren fragmentierte Versorgung, Alter, chronisch-obstruktive Lungenerkrankung, systolischer Druck in den Lungenarterien und paravalvuläre Lecks signifikant mit der 5‑Jahres-Mortalität assoziiert. Die fragmentierte Versorgung (Hazard-Ratio [HR] 1,510; 95% Konfidenzintervall [KI] 1,080–2,111; p = 0,016), das Alter (HR 1,024; 95% KI 1,001–1,048; p = 0,045), paravalvuläre Lecks (HR 1,863; 95% KI 1,076‑3,228; p = 0,026) und eine chronisch-obstruktive Lungenerkrankung (HR 1,616; 95% KI 1,114–2,344; p = 0,012) erwiesen sich in einer multivariaten Analyse nach Bereinigung um andere Risiken als signifikante unabhängige Prädiktoren für die 5‑Jahres-Mortalität.
Schlussfolgerung
Die fragmentierte Versorgung hat einen signifikanten prognostischen Einfluss auf die klinischen Ergebnisse und das Überleben.


Similar content being viewed by others
References
Linke A, Wenaweser P, Gerckens U et al (2014) Treatment of aortic stenosis with a self-expanding transcatheter valve: the international multi-centre ADVANCE study. Eur Heart J 35:2672–2684
Popma JJ, Adams DH, Reardon MJ et al (2014) Transcatheter aortic valve replacement using a self-expanding bioprosthesis in patients with severe aortic stenosis at extreme risk for surgery. J Am Coll Cardiol 63:1972–1981
Reinöhl J, Kaier K, Reinecke H et al (2015) Effect of availability of transcatheter aortic valve replacement on clinical practice. N Engl J Med 373:2438–2447
Vahl TP, Kodali SK, Leon MB et al (2016) Transcatheter aortic valve replacement: a modern-day ‘through the looking-glass’ adventure. J Am Coll Cardiol 67:1472–1487
Haggerty JL, Reid RJ, Freeman GK et al (2003) Continuity of care: a multidisciplinary review. BMJ 327(7425):1219–1221
Schrag D, Xu F, Hanger M et al (2006) Fragmentation of care for frequently hospitalized urban residents. Med Care 44(6):560–567
Tsai TC, Joynt KE, Orav EJ et al (2013) Variation in surgical-readmission rates and quality of hospital care. N Engl J Med 369(12):1134–1142
Morris MS, Deierhoi RJ, Richman JS et al (2014) The relationship between timing of surgical complications and hospital readmission. JAMA Surg 149(4):348–354
Glance LG, Kellermann AL, Osler TM et al (2014) Hospital readmission after noncardiac surgery: the role of major complications. JAMA Surg 149(5):439–445
Lawson EH, Hall BL, Louie R et al (2013) Association between occurrence of a postoperative complication and readmission: implications for quality improvement and cost savings. Ann Surg 258(1):10–18
Wang A, Li Z, Rymer JA et al (2019) Relation of postdischarge care fragmentation and outcomes in transcatheter aortic valve implantation from the STS/ACC TVT registry. Am J Cardiol 124(6):912–919
Baumgartner H, Falk V, Bax JJ et al (2017) 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J 38:2739–2791
vanWalraven C, Taljaard M, Etchells E et al (2010) The independent association of provider and information continuity on outcomes after hospital discharge: implications for hospitalists. J Hosp Med 5(7):398–405
vanWalraven C, Oake N, Jennings A et al (2010) The association between continuity of care and outcomes: a systematic and critical review. J Eval Clin Pract 16(5):947–956
vanWalraven C, Mamdani M, Fang J et al (2004) Continuity of care and patient outcomes after hospital discharge. J Gen Intern Med 19(6):624–631
Brooke BS, Goodney PP, Kraiss LW et al (2015) Readmission destination and risk of mortality after major surgery: an observational cohort study. Lancet 386:884–895
Tsai TC, Orav EJ, Jha AK (2015) Care fragmentation in the postdischarge period: surgical readmissions, distance of travel, and postoperative mortality. JAMA Surg 150:59–64
Zheng C, Habermann EB, Shara NM et al (2016) Fragmentation of care after surgical discharge: non-index readmission after major cancer surgery. J Am Coll Surg 222:780–789
Birkmeyer JD, Siewers AE, Finlayson EV et al (2002) Hospital volume and surgical mortality in the United States. N Engl J Med 346:1128–1137
Hannan EL, Radzyner M, Rubin D et al (2002) The influence of hospital and surgeon volume on in-hospital mortality for colectomy, gastrectomy, and lung lobectomy in patients with cancer. Surgery 131:6–15
Carroll JD, Vemulapalli S, Dai D et al (2017) Procedural experience for transcatheter aortic valve replacement and relation to outcomes: the STS/ACC TVT registry. J Am Coll Cardiol 70:29–41
Henry TD, Sharkey SW, Burke MN et al (2007) A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation 116:721–728
Nichol G, Aufderheide TP, Eigel B et al (2010) Regional systems of care for out-of-hospital cardiac arrest: a policy statement from the American Heart Association. Circulation 121:709–729
Rodes-Cabau J, Webb JG, Cheung A et al (2012) Long-term outcomes after transcatheter aortic valve implantation: insights on prognostic factors and valve durability from the Canadian multicenter experience. J Am Coll Cardiol 60:1864–1875
Ferraris VA, Ferraris SP, Harmon RC et al (2001) Risk factors for early hospital readmission after cardiac operations. J Thorac Cardiovasc Surg 122:278–286
Cote CL, Singh S, Yip AM et al (2015) Increased distance from the tertiary cardiac center is associated with worse 30-day outcomes after cardiac operations. Ann Thorac Surg 100:2213–2218
Chou S, Deily ME, Li S (2014) Travel distance and health outcomes for scheduled surgery. Med Care 52:250–257
Kind AJ, Bartels C, Mell MW et al (2010) For-profit hospital status and rehospitalizations to different hospitals: an analysis of medicare data. Ann Intern Med 153(11):718–772
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
E. Karacop, A. Enhos and N. Bakhshaliyev declare that they have no competing interests. The authors alone are responsible for the content and writing of the paper. The authors have had full control of all primary data and they agree to allow the journal to review their data if requested.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Karacop, E., Enhos, A. & Bakhshaliyev, N. Impact of postdischarge care fragmentation on clinical outcomes and survival following transcatheter aortic valve replacement. Herz 46 (Suppl 2), 180–186 (2021). https://doi.org/10.1007/s00059-020-04976-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-020-04976-2
Keywords
- Patient readmission
- Aortic stenosis
- Chronic obstructive pulmonary disease
- Paravalvular leakage
- Mortality