Abstract
Aim
The aim of this study was to analyze differences in the timing of invasive management of patients with high-risk acute coronary syndrome without persistent ST-segment elevation (hr-NSTE-ACS) or myocardial infarction without persistent ST-segment elevation (NSTEMI) between on- and off-hours in a German chest pain unit (CPU).
Patients and methods
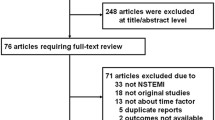
We retrospectively enrolled 160 NSTEMI patients in the study, who were admitted to two German CPUs in 2013. Patients presenting on weekdays between 8 a.m. and 6 p.m. were compared with patients presenting during off-hours. Data analysis included time intervals from admission to invasive management (goals: for hr-NSTE-ACS, <2 h; for NSTEMI, <24 h) and the resulting guideline adherence.
Results
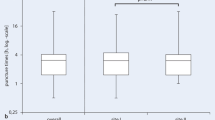
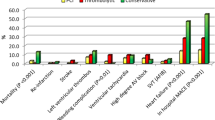
Guideline-adherent timing of an invasive strategy did not differ significantly between the on-hour (6.5 h [3.0–22.0 h], 79.9 %) and off-hour groups (10.5 h [2.0–20.0 h], 75.3 %; p = 0.94), without additional significant differences between admissions during off-hours Monday to Thursday and weekends (10.0 h [2.0–19.0 h], 75.6 % vs. 7.5 h [2.0–20.0 h], 76.2 %; p = 0.96).
Conclusion
Our exemplary experience in two different German CPUs demonstrates adequate timing of coronary catheterization in over 75 % of cases, irrespective of admission during on- or off-hours. Nationwide validation of our findings by the German CPU registry is mandatory.
Zusammenfassung
Zielsetzung
Die aktuelle Studie analysiert die leitliniengerechte zeitliche Initiierung der invasiven Koronardiagnostik beim akuten Koronarsyndrom (ACS) ohne persistierende ST-Strecken-Hebung (NSTE) bzw. Herzinfarkt ohne persistierende ST-Strecken-Hebung (NSTEMI) mit hohem Risiko (HR) im Chest-Pain-Unit(CPU)-Konzept unter Gegenüberstellung von Regelarbeitszeit und Bereitschaftsdienstzeit.
Methoden
Retrospektiv wurden 160 konsekutive Patienten mit Aufnahme in zwei deutschen CPU im Jahr 2013 und mit der Entlassungsdiagnose eines NSTEMI in die Studie eingeschlossen. Die Zeitintervalle von der Aufnahme bis zur invasiven Therapie (Ziel: bei HR-NSTE-ACS <2 h; bei NSTEMI <24 h) zwischen Patienten mit Aufnahmezeitpunkt wochentags von 8 bis 18 h gegenüber einem Aufnahmezeitpunkt während der Bereitschaftsdienstzeit und die resultierende Leitlinienadhärenz wurden verglichen.
Ergebnisse
Im Gesamtkollektiv ergab sich kein signifikanter Unterschied in Bezug auf ein leitliniengerechtes Timing einer invasiven Strategie zwischen Regel- (6,5 h [3,0–22,0 h], 79,9 %) und Bereitschaftsdienstzeit (10,5 h [2,0–20,0 h], 75,3 %; p =0,94) ohne zusätzlichen Unterschied bei Aufnahme im Bereitschaftsdienst in der Zeit von Montag bis Donnerstag (10,0 h [2,0–19,0 h], 75,6 %) gegenüber freitagabends bis montagmorgens (7,5 h [2,0–20,0 h], 76,2 %; p =0,96).
Schlussfolgerung
Unsere exemplarische Analyse in zwei unterschiedlichen deutschen CPU zeigt eine Leitlinienadhärenz von über 75 % in Bezug auf eine zeitgerechte Koronardiagnostik beim NSTEMI unabhängig von Tag und Uhrzeit der Vorstellung. Unter Nutzung des deutschen CPU-Registers ist eine deutschlandweite Validierung zur Verbesserung der Versorgungsqualität sinnvoll.




Similar content being viewed by others
References
Achenbach S, Szardien S, Zeymer U et al (2012) Kommentar zu den Leitlinien der Europäischen Gesellschaft für Kardiologie (ESC) zur Diagnostik und Therapie des akuten Koronarsyndroms ohne persistierende ST-Streckenhebung. Kardiologe 6:283–301
Glaser R, Naidu SS, Selzer F et al (2008) Factors associated with poorer prognosis for patients undergoing primary percutaneous coronary intervention during off-hours: biology or systems failure? JACC Cardiovasc Interv 1(6):681–688
Sadeghi HM, Grines CL, Chandra HR et al (2004) Magnitude and impact of treatment delays on weeknights and weekends in patients undergoing primary angioplasty for acute myocardial infarction (the CADILLAC Trial). Am J Cardiol 94:637–640
Kostis WJ, Demissie K, Marcella SW et al (2007) Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med 356:1099–1109
Birkemeyer R, Rillig A, Miljak T et al (2012) The off-hours paradigm in primary PCI can be overcome by a uniform regional treatment protocol. Int J Cardiol 14;157(3):438–439
Siudak Z, Rakowski T, Dziewierz A et al (2011) Primary percutaneous coronary intervention during on- vs off-hours in patients with ST-elevation myocardial infarction. Results from EUROTRANSFER Registry. Kardiol Pol 69(10):1017–1022
Casella G, Ottani F, Ortolani P et al (2011) Off-hour primary percutaneous coronary angioplasty does not affect outcome of patients with ST-Segment elevation acute myocardial infarction treated within a regional network for reperfusion: The REAL (Registro Regionale Angioplastiche dell’Emilia-Romagna) registry. JACC Cardiovasc Interv 4(3):270–278
Breuckmann F, Hochadel M, Voigtländer T et al (2015) On- versus off-hour supply in acute coronary syndromes with persistent ST-segment elevation in certified German chest pain units. Eur Heart J Acute Cardiovasc Care pii:2048872615624845 (Epub ahead of print)
Breuckmann F, Remberg F, Böse D et al (2016) Guideline-conforming timing of invasive management in troponin-positive or high-risk acute coronary syndrome without persistent ST-segment elevation in German chest pain units: exemplary comparison between urban university maximum care versus rural regional primary care. Herz 41(2):151–158
Hamm CW, Bassand JP, Agewall S (2011) ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 32(23):2999–3054
Roffi M, Patrono C, Collet JP et al (2016) ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 37(3):267–315
Apple FS, Smith SW, Pearce LA et al (2008) Use of the Centaur TnI-Ultra assay for detection of myocardial infarction and adverse events in patients presenting with symptoms suggestive of acute coronary syndrome. Clin Chem 54(4):723–728
Giannitsis E, Becker M, Kurz K et al (2010) High-sensitivity cardiac troponin T for early prediction of evolving non-ST-segment elevation myocardial infarction in patients with suspected acute coronary syndrome and negative troponin results on admission. Clin Chem 56(4):642–650
Breuckmann F, Post F, Giannitsis E et al (2008) Kriterien der Deutschen Gesellschaft für Kardiologie – Herz- und Kreislaufforschung für “Chest Pain Units”. Kardiologe 2(5):389–394
Post F, Gori T, Senges J et al (2012) Establishment and progress of the chest pain unit certification process in Germany and the local experiences of Mainz. Eur Heart J 33(6):682–686
Münzel T (2015) German Society of Cardiology criteria for establishing chest pain units. Eur Heart J 21;36(8):464–467
Breuckmann F, Burt DR, Melching K et al (2015) Chest Pain Centers: A comparison of accreditation programs in Germany and the United States. Crit Pathw Cardiol 14(2):67–73
Breuckmann F, Rassaf T (2015) First update of the criteria for certification of chest pain units in Germany – facelift or new model? Crit Pathw Cardiol 15(1):29–31
Post F, Giannitsis E, Riemer T et al (2012) Pre- and early in-hospital procedures in patients with acute coronary syndromes: first results of the “German chest pain unit registry”. Clin Res Cardiol 101(12):983–991
Breuckmann F, Hochadel M, Darius H et al (2015) Guideline-adherence and perspectives in the acute management of unstable angina – Initial results from the German chest pain unit registry. J Cardiol 66(2):108–113
Breuckmann F, Hochadel M, Münzel T et al (2015) Timing of percutaneous coronary intervention in troponin-negative patients with acute coronary syndrome without persistent ST-segment elevation: preliminary results and status quo in German chest pain units. Crit Pathw Cardiol 14(1):7–11
Pollack CV Jr, Hollander JE, Chen AY et al (2009) Non-ST-elevation myocardial infarction patients who present during off hours have higher risk profiles and are treated less aggressively, but their outcomes are not worse: a report from Can Rapid Risk Stratification of Unstable Angina Patients Suppress ADverse Outcomes with Early Implementation of the ACC/AHA Guidelines CRUSADE initiative. Crit Pathw Cardiol 8(1):29–33
Illmann A, Riemer T, Erbel R et al (2014) Disease distribution and outcome in troponin-positive patients with or without revascularization in a chest pain unit: results of the German CPU-Registry. Clin Res Cardiol 103(1):29–40
Maier LS, Darius H, Giannitsis E et al (2013) The German CPU Registry: comparison of troponin positive to troponin negative patients. Int J Cardiol 168(2):1651–1653
Borna C, Thelin J, Ohlin B (2014) High-sensitivity troponin T as a diagnostic tool for acute coronary syndrome in the real world: an observational study. Eur J Emerg Med 21(3):181–188
Thiele H, Rach J, Klein N et al (2012) Optimal timing of invasive angiography in stable non-ST-elevation myocardial infarction: the Leipzig Immediate versus early and late PercutaneouS coronary Intervention triAl in NSTEMI (LIPSIA-NSTEMI Trial). Eur Heart J 33(16):2035–2043
Acknowledgements
This work is part of the doctoral thesis of F. Remberg.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
F. Breuckmann, F. Remberg, D. Böse, J. Waltenberger, D. Fischer, and T. Rassaf state that there are no conflicts of interest.
The accompanying manuscript does not include studies on humans or animals performed by any of the authors.
Additional information
D. Fischer and T. Rassaf contributed equally and are joint senior authors.
Rights and permissions
About this article
Cite this article
Breuckmann, F., Remberg, F., Böse, D. et al. On- versus off-hour care for patients with non-ST-segment elevation myocardial infarction in Germany. Herz 41, 725–731 (2016). https://doi.org/10.1007/s00059-016-4425-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-016-4425-5
Keywords
- Myocardial infarction, non-ST segment elevation
- Patient admission
- Hospitalization
- Chest pain unit
- Coronary angiography