Abstract
Background
Adiponectin, a protein hormone produced by adipose tissues, exhibits anti-inflammatory functions in various models. This study was investigated the effects of adiponectin on dextran sodium sulfate (DSS)-colonic injury, inflammation, apoptosis, and intestinal barrier dysfunction in Caco-2 cell and mice.
Materials and methods
The results showed that DSS caused inflammatory response and intestinal barrier dysfunction in vitro and in vivo. Adiponectin injection alleviated colonic injury and rectal bleeding in mice. Meanwhile, adiponectin downregulated colonic IL-1β and TNF-α expressions and regulated apoptosis relative genes to attenuate DSS-induced colonic inflammation and apoptosis. Adiponectin markedly reduced serum lipopolysaccharide concentration, a biomarker for intestinal integrity, and enhanced colonic expression of tight junctions (ZO-1 and occludin). The in vitro data further demonstrated that adiponectin alleviated DSS-induced proinflammatory cytokines production and the increased permeability in Caco-2 cells.
Conclusion
Adiponectin plays a beneficial role in DSS-induced inflammation via alleviating apoptosis and improving intestinal barrier integrity.
Similar content being viewed by others
Background
Inflammatory bowel diseases (IBD), characterized by rectal bleeding, diarrhea, intestinal motility disorder, and colonic shortening, are linked with colonic chronic inflammation [1, 2]. Recently, Intestinal macrophages and dendritic cells have been indicated to involve in the initiation of inflammation in IBD through inappropriate responses to enteric microbial stimuli, inefficient clearance of microbes from host tissues, and impaired transition from appropriate proinflammatory responses to anti-inflammatory responses [3,4,5]. Chronic inflammatory response further contributes to the pathogenesis of IBD as highlighted by recent genome-wide association studies [6,7,8,9]. Therefore, anti-inflammatory drugs serve as a potential therapy for IBD patients.
Adiponectin is a protein hormone produced by adipose tissues and has various protective properties. The molecular mechanism of adiponectin is associated with its receptors, including adiponectin receptor 1, 2 and T-cadherin. Activation of adiponectin receptors inhibits inflammatory response and oxidative stress [10, 11]. Compelling evidence has demonstrated the anti-inflammatory function of adiponectin in various inflammatory models, such as skin inflammation [12], peripheral inflammation [13], LPS-induced inflammatory response in adipocytes [14]. However, the anti-inflammatory effect of adiponectin on colonic inflammation is still unknown. Thus, in this study, effects of adiponectin on dextran sodium sulfate (DSS)-colonic inflammation and injury were investigated in Caco-2 cell lines and Kunming mice.
Materials and methods
Animal model and groups
120 female Kunming mice (20.44 ± 0.83 g) were randomly divided into four groups: control group (Cont, n = 30), DSS-treated group (DSS, n = 30), adiponectin group (AG, n = 30), and DSS plus adiponectin group (DA, n = 30). Mice in DSS and DA groups received 4% DSS (average molecular weight 5000, Sigma-Aldrich) instead for tap water to establish IBD model [15]. Mice in AG and DA groups were intraperitoneally administrated with full-length adiponectin (2 µg/g, 0.2 ml/mouse) [16]. The control and untreated challenged animals received the same volume of saline alone.
Ten mice from each group were killed at days 4, 7, and 10 (n = 10). The length and weight of colonic tissues were determined in each mouse. Then, one piece of colon tissues in each mouse was collected and immediately frozen in liquid nitrogen for RT-PCR and western blotting analyses. All experiments involving animals in this study were approved by the animal welfare committee of Shandong University.
Clinical evaluation of DSS colitis
Diarrhea ration from mice were recorded at days 4, 7, and 10. A diarrhea score was used to evaluate diarrhea ratio after DSS exposure as follows: 0 means no diarrhea was noticed; 2 points mean little diarrhea with pasty and semiformed stools; and 4 points mean serious diarrhea with liquid stools [17]. Stool blood concentrations were determined through haemoccult tests (Beckman Coulter) and a bleeding score was used to evaluate the DSS colitis as follows: 0 means no blood was noticed; 2 points mean positive haemoccult; and 4 points mean gross bleeding in mice.
Serum lipopolysaccharide (LPS) determination
Blood samples were collected through eyes orbiting and serum was separated by centrifugation at 3000×g for 10 min and under 4 °C. Serum LPS were determined by A Mouse LPS ELISA kits (Wuhan Cusabio, China).
Cell lines and cell culture
Human epithelial Caco-2 cells were grown in Dulbecco’s modified Eagle medium (DMEM)/F12 supplemented with 10% FBS (HyClone, Logan, UT) and 50 U/mL penicillin–streptomycin and maintained at 37 °C in a humidified chamber of 5% CO2 [18]. Confluent cells (85–90%) were incubated with different concentrations of adiponectin (AD, 10, 50, 100, and 200 µM) and 2% DSS for 4 days to establish inflammatory model [19].
Cellular proinflammatory cytokine measurement
Cellular proinflammatory cytokines (IL-1β, IL-17, and TNF-α) were determined according ELISA kits (CUSABIO, Wuhan, China).
Trans-epithelial electrical resistance (TEER) measurements
Caco-2 cells were grown in a 12-well Transwell system and the changes of TEER were determined using an epithelial voltohmmeter ERS-2 (Merck Millipore, USA). When the filter-grown Caco-2 monolayers reached epithelial resistance of at least 500 Ω cm2, the cells were incubated in different dosages of AD with 2% DSS treatment. Electrical resistance was measured until similar values were recorded on three consecutive measurements. Values were corrected for background resistance due to the membrane insert and calculated as Ω cm2.
Paracellular marker FD-4 (FITC-Dextran 4 kDa) flux measurements
Paracellular permeability was estimated via FD-4 flux. Briefly, Caco-2 cells were seeded in a 12-well Transwell system to reach monolayers. After treatment with AD and DSS, cells were incubated in the upper chamber with Hank’s balanced salt solution for 2 h, which contains 1 mg/mL FD-4 solution. FD-4 signal was determined via Synergy H2 microplate reader (Biotek Instruments, USA).
Real-time PCR
Total RNA was isolated with TRIZOL regent (Invitrogen, USA) and reverse transcribed into the first strand (cDNA) using DNase I, oligo (dT) 20 and Superscript II reverse transcriptase (Invitrogen, USA). Primers were designed with Primer 5.0 according to the gene sequence of mouse to produce an amplification product. The primer sets used as followed: β-Actin, F:GTC CAC CTT CCA GCA GAT GT, R:GAA AGG GTG TAA AAC GCA GC; IL-1β, F:CTG TGA CTC GTG GGA TGA TG R:GGG ATT TTG TCG TTG CTT GT; IL-17, F:TAC CTC AAC CGT TCC ACG TC, R:TTT CCC TCC GCA TTG ACA C; TNF-α, F:AGG CAC TCC CCC AAA AGA T, R:TGA GGG TCT GGG CCA TAG AA; p53, F: GAG GTT CGT GTT TGT GCC TG, R: CTT CAG GTA GCT GGA GTG AGC; Bcl-2, F: GAA CTG GGG GAG GAT TGT GG, R: GCA TGC TGG GGC CAT ATA GT; Bax, F: CTG GAT CCA AGA CCA GGG TG, R: CCT TTC CCC TTC CCC CAT TC. Relative expression was normalized and expressed as a ratio to the expression in control group [20,21,22].
Western bolt
Proteins were extracted with protein extraction reagents (Thermo Fisher Scientific Inc., USA). Proteins (30 µg) were separated by SDS–polyacrylamide gel electrophoresis and electrophoretically transferred to apolyvinylidene difluoride (PVDF) membrane (BioRad, Hercules, CA, USA). Membranes were blocked and then incubated with the following primary antibodies: ZO-1 (ab59720), Claudin1 (ab115225), and Occludin (ab31721) (Abcam, Inc., USA). Mouse β-actin antibody (Sigma) was used for protein loading control. After primary antibody incubation, membranes were washed, incubated with alkaline phosphatase-conjugated anti-mouse or anti-rabbit IgG antibodies (Promega, Madison, WI, USA), and quantified and digitally analyzed using the image J program (NIH).
Statistical analysis
All statistical analyses were performed using SPSS 17.0 software. Group comparisons were performed using the one-way analysis of variance (ANOVA) to test homogeneity of variances via Levene’s test and followed with Tukey’s multiple comparison test. Values in the same row with different superscripts are significant (P < 0.05), while values with same superscripts are not significant different (P > 0.05).
Results
Adiponectin alleviated DSS-induced colonic injury
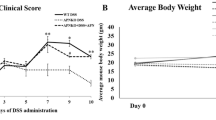
At days 7 and 10, DSS markedly reduced body weight and colonic length (P < 0.05) but adiponectin failed to alleviate the reduction (P > 0.05) (Fig. 1). From days 4 to 10, DSS exposure significantly increased rectal bleeding score and diarrhea score compared with the control group (P < 0.05). Adiponectin injection attenuated DSS-caused rectal bleeding at days 7 and 10 (P < 0.05).
Adiponectin alleviated DSS-induced colonic inflammation
DSS enhanced colonic expressions of IL-1β and TNF-α and day 4 and IL-1β, IL-17, and TNF-α at days 7 and 10 (P < 0.05) (Fig. 2), suggesting that DSS exposure markedly caused colonic inflammation. Although adiponectin injection failed to alleviate colonic inflammatory response at day 4, expressions of IL-1β and TNF-α at days 7 and 10 were markedly lower in DSS plus adiponectin group than that in DSS group (P < 0.05).
Adiponectin alleviated DSS-induced colonic apoptosis
At day 4, DSS treatment upregulated colonic Bax compared with the control group (P < 0.05) (Table 1). At day 7, DSS upregulated p53 and Bax genes and adiponectin injection significantly alleviated the overexpression of Bax caused by DSS (P < 0.05). At day 10, p53 and Bax were upregulated in DSS group, while downregulated in DSS + adiponectin group (P < 0.05). Meanwhile, bcl-2 was significantly lower in DSS group (P < 0.05) but adiponectin failed to attenuate the inhibitory effect (P > 0.05).
Adiponectin alleviated DSS-induced colonic barrier dysfunction
ZO-1, claudin1, and occludin are three major tight junction proteins for intestinal barrier. At day 4, DSS tended to inhibit ZO-1 and occludin, but the difference was insignificant (P > 0.05) (Fig. 3). At day 7, ZO-1 and occludin were significantly downregulated in DSS group and adiponectin enhanced colonic ZO-1 and occludin expressions after DSS exposure (P < 0.05). At day 10, ZO-1, claudin1, and occludin were inhibited in DSS group and adiponectin enhanced colonic ZO-1 and occludin expressions after DSS exposure (P < 0.05).
Blood LPS concentration has been widely used as a biomarker for intestinal barrier. In this study, we found that DSS treatment significantly increased serum LPS abundance at days 7 and 10 (P < 0.05) (Fig. 4), suggesting that DSS caused colonic injury and enhanced colonic permeability. Meanwhile, adiponectin exhibited a protective role in DSS-induced colonic injury evidenced by the lower serum LPS concentrations (P < 0.05).
Adiponectin alleviated DSS-induced cellular inflammation in Caco-2 cells
Cells incubated with DSS exhibited marked inflammatory response evidenced by the increased IL-1β, IL-17, and TNF-α generation (P < 0.05) (Table 2). Adiponectin (100 and 200 nM) significantly alleviated DSS-induced TNF-α generation (P < 0.05), and the protective effect exhibited a dosage-dependent manner. Adiponectin also tended to affect IL-1β and IL-17 production, but the difference was insignificant (P > 0.05).
Adiponectin alleviated DSS-induced increase in cellular permeability in Caco-2 cells
TEER and FD-4 flux were used to estimate the cellular permeability after DSS exposure (Fig. 5). The results showed that DSS markedly enhanced cellular permeability evidenced by the decreased TEER and increased FD-4 flux (P < 0.05) at days 2–4. Meanwhile, adiponectin alleviated DSS-induced increase in cellular permeability (P < 0.05), and the protective effect exhibited a dosage-dependent manner.
Discussion
Adiponectin is an important adipokine and previous reports suggest that adiponectin serves as a protective mechanism in inflammatory response and related diseases [23, 24]. Adiponectin deficiency promotes diarrhea, stool hemoccult, and weight loss in DSS-induced colitis and contributes to inflammation-induced colon cancer [25,26,27], indicating that adiponectin treatment may play a beneficial role in colonic inflammation. In this study, we used DSS to induce colonic inflammation and we found that adiponectin alleviated rectal bleeding and colonic injury.
In this study, DSS induced colonic inflammation and caused colonic injury, which is similar with previous reports [28,29,30]. Adiponectin has been widely demonstrated to mediate inflammatory response and exert an anti-inflammatory effect. In DSS-induced colonic inflammation, adiponectin deficiency exacerbated inflammatory response tumorigenesis [26]. Meanwhile, mice with higher adiponectin had lower expression of proinflammatory cytokines (TNF and IL-1β), adipokines, and cellular stress and apoptosis markers [31]. Shibata et al. reported that the anti-inflammatory function of adiponectin might be associated with suppressing IL-17 production from γδ-T cells [12]. In this study, adiponectin markedly alleviated DSS-induced IL-1β and TNF-α overexpression in mice, which is further demonstrated in Caco-2 cells that adiponectin alleviated DSS-caused TNF-α production.
DSS-induced colonic inflammation is commonly accompanied with apoptosis via influencing apoptosis relative proteins, such as p53, bax, and bcl-2 [32,33,34]. p53, a tumor suppressor, can directly execute apoptosis in response to various cellular stresses, such as inflammation and oxidative stress [35,36,37]. Meanwhile, p53 involves in the apoptotic mechanisms in the mitochondria by regulating bcl-2 family proteins (bax and bcl-2) [38,39,40]. In this study, DSS induced colonic apoptosis by upregulating p53 and bax and inhibiting bcl-2 expression. Meanwhile, adiponectin played a protective role in DSS-induced apoptosis through influencing p53 and bax expressions. Similarly, Long et al. reported that adiponectin treatment prevented palmitate-induced apoptosis by inducing an upregulation of bcl-2 and a downregulation of bax [41]. Adiponectin also has been demonstrated to inhibit neutrophil apoptosis via activation of AMP kinase, PKB, and ERK 1/2 MAP kinase [42].
Intestinal barrier disturbances subsequent with the increased permeability plays a crucial role in the pathogenesis of IBD [43, 44]. In this study, intestinal permeability was significantly increased and tight junctions (ZO-1, claudin1, and occludin) were downregulated in DSS-induced colonic inflammation. Interestingly, adiponectin injection improved intestinal permeability evidenced by decreasing serum LPS and enhancing colonic expressions of tight junctions in mice. The high level of serum LPS is considered to be the consequence of the increased intestinal permeability [45]. Thus, the in vivo results suggested a beneficial role of adiponectin in barrier integrity, which was further demonstrated in Caco-2 cells that adiponectin alleviated DSS-induced the decreased TEER and increased FD-4 flux.
Conclusions
Adiponectin alleviated colonic injury, inflammatory response, and apoptosis in mice. Meanwhile, adiponectin improved intestinal integrity in DSS-challenged mice evidenced by the lowered serum LPS enhanced colonic expressions of tight junctions (ZO-1 and occludin). The in vitro data further demonstrated that adiponectin alleviated DSS-induced proinflammatory cytokines production and the increased permeability in Caco-2 cells. Together, adiponectin plays a beneficial role in DSS-induced inflammation via alleviating apoptosis and improving intestinal barrier integrity.
Change history
31 March 2022
This article has been retracted. Please see the Retraction Notice for more detail: https://doi.org/10.1007/s00011-022-01564-4
References
Lee KH, Park M, Ji KY, Lee HY, Jang JH, Yoon IJ, et al. Bacterial beta-(1,3)-glucan prevents DSS-induced IBD by restoring the reduced population of regulatory T cells. Immunobiology. 2014;219:802–12.
Dominciano LC, Lee SH, Santello JM, Martinis ECD, Corassin CH, Oliveira CA. Effect of oleuropein and peracetic acid on suspended cells and mono-species biofilms formed by Staphylococcus aureus and Escherichia coli. Integr Food Nutr Metab. 2016;3:314–7.
Steinbach EC, Plevy SE. The role of macrophages and dendritic cells in the initiation of inflammation in IBD. Inflamm Bowel Dis. 2014;20:166–75.
Bao XY, Feng ZM, Yao JM, Li TJ, Yin YL. Roles of dietary amino acids and their metabolites in pathogenesis of inflammatory bowel disease. Mediat Inflamm 2017.
Donovan MG, Selmin OI, Doetschman TC, Romagnolo DF. Mediterranean diet: prevention of colorectal cancer. Front Nutr. 2017;4:59.
Rademakers G, Vaes N, Schonkeren S, Koch A, Sharkey KA, Melotte V. The role of enteric neurons in the development and progression of colorectal cancer. Bba-Rev Cancer. 2017;1868:420–34.
Ruhland MK, Coussens LM, Stewart SA. Senescence and cancer: an evolving inflammatory paradox. Bba-Rev Cancer. 2016;1865:14–22.
Colangelo T, Polcaro G, Muccillo L, D’Agostino G, Rosato V, Ziccardi P, et al. Friend or foe? The tumour microenvironment dilemma in colorectal cancer. Bba-Rev Cancer. 2017;1867:1–18.
Maru GB, Hudlikar RR, Kumar G, Gandhi K, Mahimkar MB. Understanding the molecular mechanisms of cancer prevention by dietary phytochemicals: From experimental models to clinical trials. World J Biol Chem. 2016;7:88–99.
Quinones MP, Roberts D, Velligan D, Paredes M, Walss-Bass C. Adiponectin as a potential biomarker of social cognition (SC) abnormalities in schizophrenia. Biol Psychiatry. 2014;75:339 s.
Bai YM, Chen JY, Yang WS, Chi YC, Liou YJ, Lin CC, et al. Adiponectin as a potential biomarker for the metabolic syndrome in Chinese patients taking clozapine for schizophrenia. J Clin Psychiatry. 2007;68:1834–9.
Shibata S, Tada Y, Hau CS, Mitsui A, Kamata M, Asano Y, et al. Adiponectin regulates psoriasiform skin inflammation by suppressing IL-17 production from gamma delta-T cells. Nat Commun 2015;6.
Iannitti T, Graham A, Dolan S. Adiponectin-mediated analgesia and anti-inflammatory effects in rat. PLoS One. 2015;10:e0136819.
Lazra Y, Falach A, Frenkel L, Rozenberg K, Sampson S, Rosenzweig T. Autocrine/paracrine function of globular adiponectin: inhibition of lipid metabolism and inflammatory response in 3T3-L1 adipocytes. J Cell Biochem 2015;116:754–66.
Zhang YZ, Brenner M, Yang WL, Wang P. Recombinant human MFG-E8 ameliorates colon damage in DSS- and TNBS-induced colitis in mice. Lab Investig. 2015;95:480–90.
Liu XW, Perakakis N, Gong HZ, Chamberland JP, Brinkoetter MT, Hamnvik OPR, et al. Adiponectin administration prevents weight gain and glycemic profile changes in diet-induced obese immune deficient Rag1−/− mice lacking mature lymphocytes. Metab Clin Exp. 2016;65:1720–30.
Vlantis K, Polykratis A, Welz PS, van Loo G, Pasparakis M, Wullaert A. TLR-independent anti-inflammatory function of intestinal epithelial TRAF6 signalling prevents DSS-induced colitis in mice. Gut. 2016;65:935–43.
Muto E, Dell’Agli M, Sangiovanni E, Mitro N, Fumagalli M, Crestani M, et al. Olive oil phenolic extract regulates interleukin-8 expression by transcriptional and posttranscriptional mechanisms in Caco-2 cells. Mol Nutr Food Res. 2015;59:1217–21.
Nighot P, Young K, Nighot M, Rawat M, Sung EJ, Maharshak N, et al. Chloride channel ClC-2 is a key factor in the development of DSS-induced murine colitis. Inflamm Bowel Dis. 2013;19:2867–77.
Feng HH, Yu LL, Zhang GJ, Liu GY, Yang C, Wang H, et al. Regulation of autophagy-related protein and cell differentiation by high mobility group box 1 protein in adipocytes. Mediat Inflamm. 2016;2016:1936386.
Liu G, Chen S, Guan GP, Tan J, Al-Dhabi NA, Wang HB, et al. Chitosan modulates inflammatory responses in rats infected with enterotoxigenic Escherichia coli. Mediat Inflamm. 2016;2016:7432845.
Choi GY, Kim HB, Hwang ES, Lee S, Kim MJ, Choi JY, et al. Curcumin alters neural plasticity and viability of intact hippocampal circuits and attenuates behavioral despair and COX-2 expression in chronically stressed rats. Mediat Inflamm. 2017;2017:6280925.
Azambuja RD, Azambuja LSEDS., Costa C, Rufino R. Adiponectin in asthma and obesity: protective agent or risk factor for more severe. Disease? Lung. 2015;193:749–55.
Jin ZX, Du Y, Schwaid AG, Asterholm IW, Scherer PE, Saghatelian A, et al. Maternal adiponectin controls milk composition to prevent neonatal inflammation. Endocrinology. 2015;156:1504–13.
Saxena A, Baliga MS, Ponemone V, Kaur K, Larsen B, Fletcher E, et al. Mucus and adiponectin deficiency: role in chronic inflammation-induced colon cancer. Int J Colorectal Dis. 2013;28:1267–79.
Saxena A, Chumanevich A, Fletcher E, Larsen B, Lattwein K, Kaur K, et al. Adiponectin deficiency: role in chronic inflammation induced colon cancer. Bba-Mol Basis Dis. 2012;1822:527–36.
Ciampolini M. A subjective, reproducible limit of intake in the child and the adult. Integr Food Nutr Metab. 2016;3:345–6.
Martinez Gomez JM, Chen L, Schwarz H, Karrasch T. CD137 facilitates the resolution of acute DSS-induced colonic inflammation in mice. PLoS One. 2013;8:e73277.
Shi C, Liang Y, Yang J, Xia Y, Chen H, Han H, et al. MicroRNA-21 knockout improve the survival rate in DSS induced fatal colitis through protecting against inflammation and tissue injury. PLoS One. 2013;8:e66814.
Pirola L, Ferraz JC. Role of pro- and anti-inflammatory phenomena in the physiopathology of type 2 diabetes and obesity. World J Biol Chem. 2017;8:120–8.
Arsenescu V, Narasimhan ML, Halide T, Bressan RA, Barisione C, Cohen DA, et al. Adiponectin and plant-derived mammalian adiponectin homolog exert a protective effect in murine colitis. Dig Dis Sci. 2011;56:2818–32.
Ranganathan P, Jayakumar C, Li DY, Ramesh G. UNC5B receptor deletion exacerbates DSS-induced colitis in mice by increasing epithelial cell apoptosis. J Cell Mol Med. 2014;18:1290–9.
Park DK, Park HJ. Ethanol extract of cordyceps militaris grown on germinated soybeans attenuates dextran-sodium-sulfate-(DSS-) induced colitis by suppressing the expression of matrix metalloproteinases and inflammatory mediators. Biomed Res Int. 2013.
Radha G, Raghavan SC. BCL2: a promising cancer therapeutic target. Bba-Rev Cancer. 2017;1868:309–14.
Le Borgne F, Ravaut G, Bernard A, Demarquoy J. L-carnitine protects C2C12 cells against mitochondrial superoxide overproduction and cell death. World J Biol Chem. 2017;8:86–94.
Kwon SK, Saindane M, Baek KH. p53 stability is regulated by diverse deubiquitinating enzymes. Bba-Rev Cancer. 2017;1868:404–11.
Miciak J, Bunz F. Long story short: p53 mediates innate immunity. Bba-Rev Cancer. 2016;1865:220–7.
Dashzeveg N, Yoshida K. Crosstalk between tumor suppressors p53 and PKC delta: execution of the intrinsic apoptotic pathways. Cancer Lett. 2016;377:158–63.
Rao PVLNS., Kiranmayi VS, Swathi P, Jeyseelan L, Suchitra MM, Bitla AR. Comparison of two analytical methods used for the measurement of total antioxidant status. J Antioxid Act. 2015;1:22–8.
Cordani M, Butera G, Pacchiana R, Donadelli M. Molecular interplay between mutant p53 proteins and autophagy in cancer cells. Bba-Rev Cancer. 2017;1867:19–28.
Long J, Su YX, Deng HC. Lipoapoptosis pathways in pancreatic beta-cells and the anti-apoptosis mechanisms of adiponectin. Horm Metab Res. 2014;46:722–7.
Rossi A, Lord JM. Adiponectin inhibits neutrophil apoptosis via activation of AMP kinase, PKB and ERK 1/2 MAP kinase. Apoptosis. 2013;18:1469–80.
Antoni L, Nuding S, Wehkamp J, Stange EF. Intestinal barrier in inflammatory bowel disease. World J Gastroenterol. 2014;20:1165–79.
Laukoetter MG, Nava P, Nusrat A. Role of the intestinal barrier in inflammatory bowel disease. World J Gastroenterol. 2008;14:401–7.
Rashti Z, Koohsari H. Antibacterial effects of supernatant of lactic acid bacteria isolated from different Dough’s in Gorgan city in north of Iran. Integr Food Nutr Metab. 2015;2:193–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Responsible Editor: John Di Battista.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Zhao, Q., Liu, Y., Tan, L. et al. RETRACTED ARTICLE: Adiponectin administration alleviates DSS-induced colonic inflammation in Caco-2 cells and mice. Inflamm. Res. 67, 663–670 (2018). https://doi.org/10.1007/s00011-018-1155-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-018-1155-6