Abstract
Purpose of Review
Cannabis abstinence, traditionally, is the primary outcome in cannabis use disorder (CUD) treatment trials. Due to the changing legality of cannabis, patient goals, and preliminary evidence suggesting that individuals who reduce their cannabis use may show functional improvements, cannabis reduction is a desirable alternative outcome in CUD trials. We review challenges in measuring cannabis reduction and the evidence to support various definitions of reduction.
Recent Findings
Reduction in number of cannabis use days was associated with improvements in functioning across several studies. Reductions in quantity of cannabis used was inconsistently associated with improvements in functioning, though definitions of quantity varied across studies. Different biomarkers may be used depending on the reduction outcome.
Summary
Biologically confirmed reductions in frequency of cannabis use days may represent a viable endpoint in clinical trials for cannabis use disorder. Additional research is needed to better quantify reduction in cannabis amounts.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hasin DS, Saha TD, Kerridge BT, et al. Prevalence of marijuana use disorders in the United States between 2001-2002 and 2012-2013. JAMA Psychiatry. 2015;72(12):1235–42.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th edition, text revision): Washington,D,C.,American Psychiatric Pub; 2000.
Gates PJ, Sabioni P, Copeland J, Le Foll B, Gowing L. Psychosocial interventions for cannabis use disorder. Cochrane Database of Systematic Reviews 2016, Issue 5. Art. No.: CD005336. https://doi.org/10.1002/14651858.CD005336.pub4
Nielsen S, Gowing L, Sabioni P, Le Foll B. Pharmacotherapies for cannabis dependence. Cochrane Database of Systematic Reviews 2019, Issue 1. Art. No.: CD008940. https://doi.org/10.1002/14651858.CD008940.pub3.
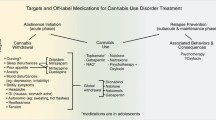
Sherman BJ, McRae-Clark AL. Treatment of cannabis use disorder: current science and future outlook. Pharmacotherapy. 2016;36(5):511–35.
Sahlem GL, Tomko RL, Sherman BJ, Gray KM, McRae-Clark AL. Impact of cannabis legalization on treatment and research priorities for cannabis use disorder. Int Rev Psychiatry. 2018;30(3):216–25.
Masters MN, Haardorfer R, Windle M, Berg C. Psychosocial and cessation-related differences between tobacco-marijuana co-users and single product users in a college student population. Addict Behav. 2018;77:21–7.
McClure EA, Tomko RL, Salazar CA, Akbar SA, Squeglia LM, Herrmann E, et al. Tobacco and cannabis co-use: drug substitution, quit interest, and cessation preferences. Exp Clin Psychopharmacol. 2019;27(3):265–75.
•• Lee DC, Schlienz NJ, Peters EN, Dworkin RH, Turk DC, Strain EC, et al. Systematic review of outcome domains and measures used in psychosocial and pharmacological treatment trials for cannabis use disorder. Drug Alcohol Depend. 2019;194:500–17 This systematic review describes primary and secondary outcome measures typically assessed in psychosocial and pharmacotherapy clinical trials for cannabis use disorder.
Lozano BE, Stephens RS, Roffman RA. Abstinence and moderate use goals in the treatment of marijuana dependence. Addiction. 2006;101(11):1589–97.
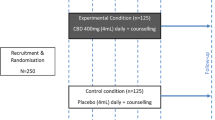
•• Loflin MJE, Huestis MA, Aklin, WM, Budney AJ, D’Souza DC, Dworkin RH, Gray KM, Kiluk BD, Lee D, Le Foll B, Lile JA, Mason BJ, McRae-Clark AL, Montoya I, Peters EN, Ramey T, Turk DC, Vandrey R, Weiss RD, Strain EC. Choosing clinical endpoints for cannabis use disorder clinical trials: ACTTION meeting recommendations. Under Review. This manuscript reviews recommendations from experts in cannabis use disorder with regard to the assessment of cannabis use in clinical trials.
Riggs NR, Conner BT, Parnes JE, Prince MA, Shillington AM, George MW. Marijuana eCHECKUPTO GO: Effects of a personalized feedback plus protective behavioral strategies intervention for heavy marijuana-using college students. Drug Alcohol Depend. 2018;190:13–9.
Food and Drug Administration. Alcoholism: developing drugs for treatment (No FDA D-0152-001) Silver Spring. https://www.fda.gov/files/drugs/published/Alcoholism---Developing-Drugs-for-Treatment.pdf
Creswell KG, Chung T. Treatment for alcohol use disorder: progress in predicting treatment outcome and validating non-abstinent end points. Alcohol Clin Exp Res. 2018;42(10):1874–9.
Witkiewitz K, Finney JW, Harris AH, Kivlahan DR, Kranzler HR. Recommendations for the design and analysis of treatment trials for alcohol use disorders. Alcohol Clin Exp Res. 2015;39(9):1557–70.
Witkiewitz K, Hallgren KA, Kranzler HR, et al. Clinical validation of reduced alcohol consumption after treatment for alcohol dependence using the World Health Organization risk drinking levels. Alcohol Clin Exp Res. 2017;41(1):179–86.
Hasin DS, Wall M, Witkiewitz K, Kranzler HR, Falk D, Litten R, et al. Change in non-abstinent WHO drinking risk levels and alcohol dependence: a 3 year follow-up study in the US general population. Lancet Psychiatry. 2017;4(6):469–76.
Cuttler C, Spradlin A. Measuring cannabis consumption: psychometric properties of the Daily Sessions, Frequency, Age of Onset, and Quantity of Cannabis Use Inventory (DFAQ-CU). PLoS One. 2017;12(5):e0178194.
Walden N, Earleywine M. How high: quantity as a predictor of cannabis-related problems. Harm Reduct J. 2008;5:1–8.
Norberg MM, Mackenzie J, Copeland J. Quantifying cannabis use with the Timeline Followback approach: a psychometric evaluation. Drug Alcohol Depend. 2012;121:247–52.
Tomko RL, Baker NL, McClure EA, Sonne SC, McRae-Clark AL, Sherman BJ, et al. Incremental validity of estimated cannabis grams as a predictor of problems and cannabinoid biomarkers: evidence from a clinical trial. Drug Alcohol Depend. 2018;182:1–7.
Hindocha C, Norberg MM, Tomko RL. Solving the problem of cannabis quantification. Lancet Psychiatry. 2018;5(4):e8.
Casajuana C, López-Pelayo H, Miquel L, Balcells-Oliveró MM, Colom J, Gual A. Quantitative criteria to screen for cannabis use disorder. Eur Addict Res. 2018;24(3):109–17.
Casajuana Kögel C, Balcells-Olivero MM, López-Pelayo H, Miquel L, Teixidó L, Colom J, et al. The standard joint unit. Drug Alcohol Depend. 2017;176:109–16.
Zeisser C, Thompson K, Stockwell T, Duff C, Chow C, Vallance K, et al. A ‘standard joint’? The role of quantity in predicting cannabis-related problems. Addict Res Theory. 2012;20(1):82–92.
Buu A, Hu YH, Pampati S, Arterberry BJ, Lin HC. Predictive validity of cannabis consumption measures: results from a national longitudinal study. Addict Behav. 2017;73:36–40.
Hser YI, Mooney LJ, Huang D, Zhu Y, Tomko RL, McClure E, et al. Reductions in cannabis use are associated with improvements in anxiety, depression, and sleep quality, but not quality of life. J Subst Abus Treat. 2017;81:53–8.
Brezing CA, Choi CJ, Pavlicova M, Brooks D, Mahony AL, Mariani JJ, et al. Abstinence and reduced frequency of use are associated with improvements in quality of life among treatment-seekers with cannabis use disorder. Am J Addict. 2018;27(2):101–7.
Mooney LJ, Zhu Y, Yoo C, Valdez J, Moino K, Liao JY, et al. Reduction in cannabis use and functional status in physical health, mental health, and cognition. J NeuroImmune Pharmacol. 2018;13(4):479–87.
Liao JY, Mooney LJ, Zhu Y, Valdez J, Yoo C, Hser YI. Relationships between marijuana use, severity of marijuana-related problems, and health-related quality of life. Psychiatry Res. 2019 ; 279: 237-243.
Jonas B, Tensil MD, Tossmann P, Strüber E. Effects of treatment length and chat-based counseling in a web-based intervention for cannabis users: randomized factorial trial. J Med Internet Res. 2018;20(5):e166.
Tossmann P, Jonas B, Tensil M, Lang P, Strüber E. A controlled trial of an internet-based intervention program for cannabis users. Cyberpsychol Behav Soc Netw. 2011;14(11):673–9.
McCambridge J, Strang J. The efficacy of single-session motivational interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: results from a multi-site cluster randomized trial. Addiction. 2004;99(1):39–52.
• Fitzmaurice GM, Lipsitz SR, Weiss RD. Statistical considerations in the choice of endpoint for drug use disorder trials. Drug Alcohol Depend. 2017;181:219–22 This manuscript illustrates statistical and power considerations when choosing an outcome measure in substance use disorder clinical trials.
Beckstead JW. On measurements and their quality: paper 2: random measurement error and the power of statistical tests. Int J Nurs Stud. 2013;50(10):1416–22.
Shiffman S. Ecological momentary assessment (EMA) in studies of substance use. Psychol Assess. 2009;21(4):486–97.
Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32.
Wilson TD, Dunn EW. Self-knowledge: its limits, value, and potential for improvement. Annu Rev Psychol. 2004;55:493–18.
Schwarz N, Oyserman D. Asking questions about behavior: cognition, communication, and questionnaire construction. Am J Eval. 2001;22(2):127–60.
Tversky A, Kahneman D. Judgment under uncertainty: heuristics and biases. Science. 1974;185(4157):1124–31.
Magura S, Kang SY. Validity of self-reported drug use in high risk populations: a meta-analytical review. Subst Use Misuse. 1996;31(9):1131–53.
Baker NL, Gray KM, Sherman BJ, Morella K, Sahlem GL, Wagner AM, et al. Biological correlates of self-reported new and continued abstinence in cannabis cessation treatment clinical trials. Drug Alcohol Depend. 2018;187:270–7.
Gray KM, Watson NL, Christie DK. Challenges in quantifying marijuana use. Am J Addict. 2009;18(2):178–9.
Hindocha C, Freeman TP, Curran HV. Anatomy of a joint: comparing self-reported and actual dose of cannabis and tobacco in a joint, and how these are influenced by controlled acute administration. Cannabis Cannabinoid Res. 2017:2217–23.
El Sohly MA, Mehmedic Z, Foster S, Gon C, Chandra S, Church JC. Changes in cannabis potency over the last 2 decades (1995–2014): analysis of current data in the United States. Biol Psychiatry. 2016;79:613–9.
Mariani JJ, Brooks D, Haney M, Levin FR. Quantification and comparison of marijuana smoking practices:blunts, joints, and pipes. Drug Alcohol Depend. 2011;113(2-3):249–51.
Donovan DM, Bigelow GE, Brigham GS, Carroll KM, Cohen AJ, Gardin JG, et al. Primary outcome indices in illicit drug dependence treatment research: systematic approach to selection and measurement of drug use end-points in clinical trials. Addiction. 2012;107(4):694–708.
•• Huestis MA, Smith ML. Cannabinoid markers in biological fluids and tissues: revealing intake. Trends Mol Med. 2018;24(2):156–72 This manuscript provides a recent review of biological matrices for assessing cannabis intake.
Huestis MA, Barnes A, Smith ML. Estimating the time of last cannabis use from plasma Δ9-tetrahydrocannabinol and 11-nor-9-carboxy- Δ9-tetrahydrocannabinol concentrations. Clin Chem. 2005;51:2289–95.
Swortwood MJ, Newmeyer MN, Andersson M, Abulseoud OA, Scheidweiler KB, Huestis MA. Cannabinoid disposition in oral fluid after controlled smoked, vaporized, and oral cannabis administration. Drug Test Anal. 2017;9(6):905–15.
Lee D, Schwope DM, Milman G, Barnes AJ, Gorelick DA, Huestis MA. Cannabinoid disposition in oral fluid after controlled smoked cannabis. Clin Chem. 2012;58:748–56.
Anizan S, Milman G, Desrosiers N, Barnes AJ, Gorelick DA, Huestis MA. Oral fluid cannabinoid concentrations following controlled smoked cannabis in chronic frequent and occasional smokers. Anal Bioanal Chem. 2013;405:8451–61.
Desrosiers NA, Milman G, Mendu DR, Lee D, Barnes AJ, Gorelick DA, et al. Cannabinoids in oral fluid by on-site immunoassay and by GC-MS using two different oral fluid collection devices. Anal Bioanal Chem. 2014;406(17):4117–28.
Lee D, Huestis MA. Current knowledge on cannabinoids in oral fluid. Drug Test Anal. 2014;6:88–111.
Niedbala RS, Kardos KW, Fritch DF, Kardos S, Fries T, Waga J, et al. Detection of marijuana use by oral fluid and urine analysis following single-dose administration of smoked and oral marijuana. J Anal Toxicol. 2001;25:289–303.
Toennes SW, Ramaekers JG, Theunissen EL, Moeller MR, Kauert GF. Pharmacokinetic properties of Δ9-tetrahydrocannabinol in oral fluid of occasional and chronic users. J Anal Toxicol. 2010;34:216–21.
Vandrey R, Herrmann ES, Mitchell JM, Bigelow GE, Flegel R, LoDico C, et al. Pharmacokinetic profile of oral cannabis in humans: blood and oral fluid disposition and relation to pharmacodynamic outcomes. J Anal Toxicol. 2017;41(2):83–99.
Lovestead TM, Bruno TJ. Determination of cannabinoid vapor pressures to aid in vapor phase detection of intoxication. Forensic Chem. 2017;5:79–85.
Himes SK, Scheidweiler KB, Beck O, Gorelick DA, Desrosiers NA, Huestis MA. Cannabinoids in exhaled breath following controlled administration of smoked cannabis. Clin Chem. 2013;59(12):1780–9.
Lynch KL, Luo YR, Hooshfar S, Yun C. Correlation of breath and blood Δ9-tetrahydrocannabinol concentrations and release kinetics following controlled administration of smoked cannabis. Clin Chem. 2019;65(9):1171–9.
Beckham JC, Adkisson KA, Hertzberg J, Kimbrel NA, Budney AJ, Stephens RS, et al. Mobile contingency management as an adjunctive treatment for co-morbid cannabis use disorder and cigarette smoking. Addict Behav. 2018;79:86–92.
Sherman BJ, Caruso MA, McRae-Clark AL. Exogenous progesterone for cannabis withdrawal in women: feasibility trial of a novel multimodal methodology. Pharmacol Biochem Behav. 2019;179:22–6.
Musshoff F, Madea B. Review of biologic matrices (urine, blood, hair) as indicators of recent or ongoing cannabis use. Ther Drug Monit. 2006;28:155–63.
D'Souza DC, Cortes-Briones J, Creatura G, Bluez G, Thurnauer H, Deaso E, et al. Efficacy and safety of a fatty acid amide hydrolase inhibitor (PF-04457845) in the treatment of cannabis withdrawal and dependence in men: a double-blind, placebo-controlled, parallel group, phase 2a single-site randomised controlled trial. Lancet Psychiatry. 2019;6(1):35–45.
Smith ML, Barnes AJ, Huestis MA. Identifying new cannabis use with urine creatinine-normalized THCCOOH concentrations and time intervals between specimen collections. J Anal Toxicol. 2009;33(4):185–9.
Schwilke EW, Gullberg RG, Darwin WD, Chiang N, Cadet JL, Gorelick DA, et al. Differentiating new cannabis use from residual urinary cannabinoid excretion in chronic, daily cannabis users. Addiction. 2011;106:499–506.
Huestis MA, Scheidweiler KB, Saito T, Fortner N, Abraham T, Gustafson RA, et al. Excretion of Δ9-tetrahydrocannabinol in sweat. Forensic Sci Int. 2008;174(2-3):173–7.
Taylor M, Lees R, Henderson G, Lingford-Hughes A, Macleod J, Sullivan J, et al. Comparison of cannabinoids in hair with self-reported cannabis consumption in heavy, light and non-cannabis users. Drug Alcohol Rev. 2017;36(2):220–6.
Funding
Effort was supported by National Institutes of Health grants from the National Institute of Drug Abuse (R01 DA042114), the Eunice Kennedy Shriver National Institute of Child Health and Human Development (K12 HD055885), and the National Institute on Alcohol Abuse and Alcoholism (K23 AA025399).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Marilyn A. Huestis provides consultation to Pinney & Associates, Inc., Canopy Health Innovations, Intelligent Fingerprinting, Cannabix, Evanostics, Inc., and the Center for Forensic Science Research and Education. Kevin M. Gray provides consultation to Pfizer, Inc.
Human and Animal Rights and Informed Consent
This article does not contain any original studies with human or animal subjects performed by any of the authors.
Additional information
Key points
1. Reduction in cannabis use is an alternative to abstinence in cannabis use disorder treatment
2. Reduction in cannabis use is challenging to assess and biologically confirm, and definitions vary across trials
3. Preliminary evidence suggests that reduced number of days of cannabis use is associated with improvements in functioning
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cannabis
Rights and permissions
About this article
Cite this article
Tomko, R.L., Gray, K.M., Huestis, M.A. et al. Measuring Within-Individual Cannabis Reduction in Clinical Trials: a Review of the Methodological Challenges. Curr Addict Rep 6, 429–436 (2019). https://doi.org/10.1007/s40429-019-00290-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-019-00290-y