Abstract
Background
Cholinesterase inhibitors (ChEIs) are one of only two drug therapies available to manage cognitive decline in dementia. Given sex-specific differences in medication access and effects, it is important to understand how ChEIs are used by women and men.
Objective
The objective of this study was to provide contemporary sex-stratified evidence on patterns of ChEI use by community-dwelling older adults with dementia to inform opportunities to optimize drug prescribing.
Methods
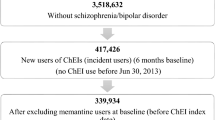
We conducted a population-based cross-sectional study examining ChEI use in older adults with dementia in Ontario, Canada. We identified all community-dwelling individuals aged 66 years and older with a pre-existing diagnosis of dementia as of 1 April, 2016. We examined the prevalence of ChEI use among women and men separately, and explored the association between ChEI use and age, sex, income status, geographic location of residence, use of palliative care services, comorbidity, and polypharmacy. Concurrent use of drugs known to impair cognition (including antipsychotics, benzodiazepines, and medications with strong anticholinergic properties) was separately assessed among women and men using multivariable analyses and prevalence risk ratios.
Results
Of 74,799 women and 52,231 men living with dementia in the community, nearly 30% currently were using a ChEI (29.3% women, 28.6% men). Close to 70% of users were receiving the target therapeutic dose. Compared to men, women were less often taking the target therapeutic dose (67.8% women vs. 71.6% men, p < 0.001). Over 20% of users also were using drugs known to impair cognition, while being treated for cognitive decline using ChEIs. Compared to men, women were more often concurrently using drugs known to impair cognition (23.9% women vs. 21.8% men, p < 0.001).
Conclusions
This is one of the first studies of ChEI use to account for important sex differences. The results remind clinicians and researchers that patterns of ChEI therapy use differ by sex, as women were less likely to receive target therapeutic doses and more vulnerable to potentially problematic polypharmacy than men.


Similar content being viewed by others
References
Kaduszkiewicz H, Zimmermann T, Beck-Bornholdt HP, van den Bussche H. Cholinesterase inhibitors for patients with Alzheimer’s disease: systematic review of randomised clinical trials. BMJ. 2005;331(7512):321–7. https://doi.org/10.1136/bmj.331.7512.321.
Small G, Bullock R. Defining optimal treatment with cholinesterase inhibitors in Alzheimer’s disease. Alzheimers Dement. 2011;7(2):177–84. https://doi.org/10.1016/j.jalz.2010.03.016.
Koller D, Hua T, Bynum JP. Treatment patterns with antidementia drugs in the United States: medicare cohort study. J Am Geriatr Soc. 2016;64(8):1540–8. https://doi.org/10.1111/jgs.14226.
Ngo J, Holroyd-Leduc JM. Systematic review of recent dementia practice guidelines. Age Ageing. 2015;44(1):25–33. https://doi.org/10.1093/ageing/afu143.
Ali TB, Schleret TR, Reilly BM, Chen WY, Abagyan R. Adverse effects of cholinesterase inhibitors in dementia, according to the pharmacovigilance databases of the United-States and Canada. PLoS One. 2015;10(12):e0144337. https://doi.org/10.1371/journal.pone.0144337.
Birks J. Cholinesterase inhibitors for Alzheimer’s disease. Cochrane Database Syst Rev. 2006;1:CD005593. https://doi.org/10.1002/14651858.cd005593.
Kavirajan H, Schneider LS. Efficacy and adverse effects of cholinesterase inhibitors and memantine in vascular dementia: a meta-analysis of randomised controlled trials. Lancet Neurol. 2007;6(9):782–92. https://doi.org/10.1016/S1474-4422(07)70195-3.
Rochon PA, Gruneir A, Gill SS, Wu W, Zhu L, Herrmann N, et al. Initial cholinesterase inhibitor therapy dose and serious events in older women and men. J Am Geriatr Soc. 2018;66(9):1692–9. https://doi.org/10.1111/jgs.15442.
Gruber-Baldini AL, Stuart B, Zuckerman IH, Simoni-Wastila L, Miller R. Treatment of dementia in community-dwelling and institutionalized medicare beneficiaries. J Am Geriatr Soc. 2007;55(10):1508–16. https://doi.org/10.1111/j.1532-5415.2007.01387.x.
Clague F, Mercer SW, McLean G, Reynish E, Guthrie B. Comorbidity and polypharmacy in people with dementia: insights from a large, population-based cross-sectional analysis of primary care data. Age Ageing. 2017;46(1):33–9. https://doi.org/10.1093/ageing/afw176.
Reppas-Rindlisbacher CE, Fischer HD, Fung K, Gill SS, Seitz D, Tannenbaum C, et al. Anticholinergic drug burden in persons with dementia taking a cholinesterase inhibitor: the effect of multiple physicians. J Am Geriatr Soc. 2016;64(3):492–500. https://doi.org/10.1111/jgs.14034.
Huey ED, Taylor JL, Luu P, Oehlert J, Tinklenberg JR. Factors associated with use of medications with potential to impair cognition or cholinesterase inhibitors among Alzheimer’s disease patients. Alzheimers Dement. 2006;2(4):314–21. https://doi.org/10.1016/j.jalz.2006.08.003.
American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63(11):2227–46. https://doi.org/10.1111/jgs.13702.
Wu YT, Beiser AS, Breteler MMB, Fratiglioni L, Helmer C, Hendrie HC, et al. The changing prevalence and incidence of dementia over time: current evidence. Nat Rev Neurol. 2017;13(6):327–39. https://doi.org/10.1038/nrneurol.2017.63.
Mazure CM, Swendsen J. Sex differences in Alzheimer’s disease and other dementias. Lancet Neurol. 2016;15(5):451–2. https://doi.org/10.1016/S1474-4422(16)00067-3.
Tam-Tham H, Nettel-Aguirre A, Silvius J, Dalziel W, Garcia L, Molnar F, et al. Provision of dementia-related services in Canada: a comparative study. BMC Health Serv Res. 2016;16:184. https://doi.org/10.1186/s12913-016-1435-1.
Canevelli M, Quarata F, Remiddi F, Lucchini F, Lacorte E, Vanacore N, et al. Sex and gender differences in the treatment of Alzheimer’s disease: a systematic review of randomized controlled trials. Pharmacol Res. 2017;115:218–23. https://doi.org/10.1016/j.phrs.2016.11.035.
Mehta N, Rodrigues C, Lamba M, Wu W, Bronskill SE, Herrmann N, et al. Systematic review of sex-specific reporting of data: cholinesterase inhibitor example. J Am Geriatr Soc. 2017;65(10):2213–9. https://doi.org/10.1111/jgs.15020.
Legato MJ, Johnson PA, Manson JE. Consideration of sex differences in medicine to improve health care and patient outcomes. JAMA. 2016;316(18):1865–6. https://doi.org/10.1001/jama.2016.13995.
Ontario Ministry of Finance. Ontario population projections update, 2017–2041. https://www.fin.gov.on.ca/en/economy/demographics/projections. Accessed 1 Oct 2018.
Jaakkimainen RL, Bronskill SE, Tierney MC, Herrmann N, Green D, Young J, et al. Identification of physician-diagnosed Alzheimer’s disease and related dementias in population-based administrative data: a validation study using family physicians’ electronic medical records. J Alzheimers Dis. 2016;54(1):337–49. https://doi.org/10.3233/JAD-160105.
Alzheimer’s Society UK. Drug treatments for Alzheimer’s disease. https://www.alzheimers.org.uk/info/20162/drugs/105/drug_treatments_for_alzheimers_disease/7. Accessed 19 Jun 2017.
The National Institute on Aging’s Alzheimer’s Disease Education and Referral (ADEAR) Center. Alzheimer’s disease medications. https://www.nia.nih.gov/sites/default/files/alzheimers-disease-medications-fact-sheet_1.pdf. Accessed 21 Jul 2017.
Schwartz LM, Woloshin S. How the FDA forgot the evidence: the case of donepezil 23 mg. BMJ. 2012;344:e1086. https://doi.org/10.1136/bmj.e1086.
Hogan DB, Bailey P, Black S, Carswell A, Chertkow H, Clarke B, et al. Diagnosis and treatment of dementia: 5. Nonpharmacologic and pharmacologic therapy for mild to moderate dementia. CMAJ. 2008;179(10):1019–26. https://doi.org/10.1503/cmaj.081103.
Rudolph JL, Salow MJ, Angelini MC, McGlinchey RE. The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch Intern Med. 2008;168(5):508–13. https://doi.org/10.1001/archinternmed.2007.106.
Ontario Ministry of Health and Long-Term Care. New eligibility requirements for the low-income Seniors Co-Payment Drug Program. http://www.health.gov.on.ca/en/public/programs/drugs/programs/copayment/copayment.aspx. Accessed 30 Jun 2019.
Johns Hopkins University. Johns Hopkins ACG case-mix adjustment system. https://www.hopkinsacg.org. Modified 2018. Accessed 17 Sep 2017.
Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1):230. https://doi.org/10.1186/s12877-017-0621-2.
Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. 2009;38(6):1228–34.
Austin PC. Absolute risk reductions, relative risks, relative risk reductions, and numbers needed to treat can be obtained from a logistic regression model. J Clin Epidemiol. 2010;63(1):2–6. https://doi.org/10.1016/j.jclinepi.2008.11.004.
Pariente A, Helmer C, Merliere Y, Moore N, Fourrier-Reglat A, Dartigues JF. Prevalence of cholinesterase inhibitors in subjects with dementia in Europe. Pharmacoepidemiol Drug Saf. 2008;17(7):655–60. https://doi.org/10.1002/pds.1613.
Rattinger GB, Burcu M, Dutcher SK, Chhabra PT, Rosenberg PB, Simoni-Wastila L, et al. Pharmacotherapeutic management of dementia across settings of care. J Am Geriatr Soc. 2013;61(5):723–33. https://doi.org/10.1111/jgs.12210.
Herrmann N, Gill SS, Bell CM, Anderson GM, Bronskill SE, Shulman KI, et al. A population-based study of cholinesterase inhibitor use for dementia. J Am Geriatr Soc. 2007;55(10):1517–23. https://doi.org/10.1111/j.1532-5415.2007.01377.x.
Pfizer. Product monograph: Aricept (donepezil hydrochloride) tablets 5 and 10 mg. https://www.pfizer.ca/sites/g/files/g10037206/f/201612/ARICEPT_PM_E_177353_18Dec2014_R.pdf. Revised December 18, 2014. Accessed 15 Jul 2018.
Gill SS, Bronskill SE, Normand SL, Anderson GM, Sykora K, Lam K, et al. Antipsychotic drug use and mortality in older adults with dementia. Ann Intern Med. 2007;146(11):775–86.
Douglas IJ, Smeeth L. Exposure to antipsychotics and risk of stroke: self controlled case series study. BMJ. 2008;337:a1227. https://doi.org/10.1136/bmj.a1227.
Kales HC, Gitlin LN, Lyketsos CG. Assessment and management of behavioral and psychological symptoms of dementia. BMJ. 2015;350:h369. https://doi.org/10.1136/bmj.h369.
Hogan DB, Bailey P, Black S, Carswell A, Chertkow H, Clarke B, et al. Diagnosis and treatment of dementia: 4. Approach to management of mild to moderate dementia. CMAJ. 2008;179(8):787–93. https://doi.org/10.1503/cmaj.070803.
Fereshtehnejad SM, Johnell K, Eriksdotter M. Anti-dementia drugs and co-medication among patients with Alzheimer’s disease : investigating real-world drug use in clinical practice using the Swedish Dementia Quality Registry (SveDem). Drugs Aging. 2014;31(3):215–24. https://doi.org/10.1007/s40266-014-0154-8.
Morgan SG, Weymann D, Pratt B, Smolina K, Gladstone EJ, Raymond C, et al. Sex differences in the risk of receiving potentially inappropriate prescriptions among older adults. Age Ageing. 2016;45(4):535–42. https://doi.org/10.1093/ageing/afw074.
Acknowledgements
We thank IMS Brogan Inc. for use of their Drug Information Database. They had no role in the design, conduct, or reporting of the study, or in the decision to submit the manuscript for publication. Parts of this material are based on data and/or information compiled and provided by the Canadian Institute for Health Information. However, the analyses, conclusions, opinions, and statements expressed in the material are those of the authors, and not necessarily those of the Canadian Institute for Health Information.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by a grant from Physicians Services Incorporated (PSI 2015-16).The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding sources. This study also was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. Paula A. Rochon is supported by the Retired Teachers of Ontario/ERO Chair in Geriatric Medicine at the University of Toronto. Peter C. Austin was supported by a Mid-Career Investigator Award from the Heart and Stroke Foundation.
Conflict of Interest
Lynn Zhu, Paula A. Rochon, Andrea Gruneir, Wei Wu, Vasily Giannakeas, Peter C. Austin, Nathan M. Stall, Lisa McCarthy, Amanda Alberga, Nathan Herrmann, Sudeep S. Gill, and Susan E. Bronskill have no conflicts of interest that are directly relevant to the contents of this article.
Ethics Approval
ICES is a prescribed entity under section 45 of Ontario’s Personal Health Information Protection Act. Section 45 authorizes ICES to collect personal health information, without consent, for the purpose of analysis or compiling statistical information with respect to the management of, evaluation or monitoring of, the allocation of resources to or planning for all or part of the health system. Projects conducted under section 45, by definition, do not require review by a research ethics board. This project was conducted under section 45, and approved by the ICES’ Privacy and Legal Office.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhu, L., Rochon, P.A., Gruneir, A. et al. Sex Differences in the Prevalent Use of Oral Formulations of Cholinesterase Inhibitors in Older Adults with Dementia. Drugs Aging 36, 875–884 (2019). https://doi.org/10.1007/s40266-019-00690-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-019-00690-9