Abstract
The care of the individual with spina bifida has changed substantially in recent years. Major advances and shifts in the prenatal and neonatal management of patients with myelomeningocele has led to improved survivability and outcomes. Most notable of these is the option for fetal repair of the spina bifida lesion. As more and more children with spina bifida are aging into adulthood, there is a growing recognition of the issues faced by adults with spina bifida, including the difficult transition to adult-based health care. Physiatrists should be aware of recent trends and advancements to help optimize outcomes for individuals across the lifespan. This article will review prenatal and neonatal advances and controversies, and will then shift gears to address issues facing adults with spina bifida.
Similar content being viewed by others
Introduction
Spina bifida is a complex congenital condition with an estimated prevalence of between 3.06 and 3.13 cases per 10,000 live births, not including cases of spina bifida occulta [1, 2•]. The introduction of mandatory folic acid supplementation and early prenatal diagnosis accompanied by the subsequent termination of affected fetuses has lead to a decrease in the incidence of spina bifida [3–5]. Hispanic children and girls experience spina bifida at higher rates than non-Hispanics and boys [6•].
The term spina bifida simply refers to splitting of the vertebral arches. This splitting can be isolated (spina bifida occulta), or it may include the meningeal sac (meningocele) or the meningeal sac plus portions of the spinal cord and/or spinal nerves (myelomeningocele) [7]. When excess lipomatous tissue is involved, the condition is referred to as lipomeningocele or lipomyelomeningocele, depending on the involvement of the nervous tissue [1]. Associated conditions that do not necessarily involve splitting of the vertebral arches, but often do, include diastematomyelia (split cord), diplomyelia (duplicated cord), myeloschisis (flatten malformed cord), and fatty filum (lipomatous tissue surrounding the filum terminale). Practitioners frequently use the term spina bifida when discussing clinical scenarios in which the individual’s nervous tissue is compromised. In this article, we will adopt this terminology, but we will be more specific when appropriate.
Over the past several decades, advances in care have led to the improved survivability of infants born with spina bifida [8, 9]. This article will address current concepts in prenatal and neonatal care, and then shift to medical issues facing the growing population of adults with spina bifida and the transition from the pediatric model of care (regional multidisciplinary clinics) to adult clinical settings.
Operative management issues for the fetus and the infant with myelomeningocele
Recent advances in prenatal diagnosis and management
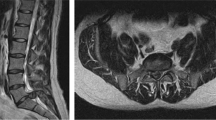
The presence of spina bifida is frequently identified before birth. The diagnosis is suspected with elevated alpha-fetoprotein (AFP) levels on triple [AFP, human chorionic gonadotropin (hCG) and estriol] or quadruple screen (triple screen + inhibin A). Using ultrasound to measure biparietal diameter on ultrasound at 11–13 weeks improves the accuracy of early detection [10]. On the routine 20-week ultrasound, fetuses with spina bifida can demonstrate a concave shape to the calvarium, a convexity of the cerebellum, and widening of the spinal column. Some centers offer fetal MRI to further delineate abnormal findings on ultrasound [11]. The formal diagnosis, including the specific subtype, is made after birth or in the operating room in the case of fetal repair. Improved prenatal detection has led to the more widespread planning for the prenatal clinical course, delivery, and after birth care of the infant with spina bifida.
Perhaps the most important advance in the management of myelomeningocele is the introduction of fetal repair. In the late 1990s, fetal repair was attempted on fetuses at various gestational ages with variable but promising success [12–15]. Due to the substantial risks to the maternal fetal dyad, experts in the field agreed that a randomized controlled trial to prove that the benefits outweighed the risks was necessary. In 2003, the Management of Myelomeningocele Study (MOMS) was started to determine the safety and efficacy of fetal surgery for spina bifida [16••]. MOMS was conducted at 3 centers with extensive expertise in fetal surgery—the Children’s Hospital of Philadelphia (CHOP), the University of California San Francisco (UCSF), and Vanderbilt University, in conjunction with George Washington University which served as the data coordinating center. Maternal fetal dyads were enrolled between 19.0 and 25.9 weeks gestation with surgical intervention occurring by 26 weeks gestation. The primary outcome of interest at 12 months was a composite measure of fetal/neonatal death plus the need for a cerebrospinal fluid shunt. The primary outcome at 30 months was a composite score of the Mental Development Index on the Bayley Scales of Infant Development II plus motor function adjusted for level [16••]. The sample was randomized into standard postnatal repair versus fetal repair by laparotomy before 26 weeks gestation. In December 2010, the data and safety monitoring committee recommended stopping the trial for efficacy after 183 of the 200 anticipated maternal fetal dyads were enrolled. Compared to the standard postnatal repair group, those who underwent fetal repair less commonly required cerebrospinal fluid shunting at 12 months and had less severe hindbrain herniation [16••]. In addition, the prenatally repaired subjects had better than expected motor functioning based on anatomic level [16••]. As MOMS concluded, MOMS2, a follow-up study to determine if the benefits of fetal repair extended past the early childhood period, was initiated. This study will conclude in 2016 and will provide neuropsychological, functional, urological, and radiographic outcomes for the former fetal subjects at school age from MOMS, as well as additional maternal outcome data. Of note, the data collected on subjects repaired prior to the initiation of MOMS showed improved neurobehavioral and functional outcomes for children status postfetal repair when compared to postnatally repaired historical controls [17, 18].
After the conclusion of MOMS, other centers began offering fetal repair for spina bifida. Whether the benefit found in the MOMS trial, which was conducted under strict protocols with highly experienced practitioners, will be replicated by other centers is yet to be determined [19]. This issue warrants careful attention as the risks of fetal repair include a higher likelihood of symptomatic tethered cord in the prenatally repaired child which can complicate the child’s clinical course [16, 20]. Additionally, for the maternal–fetus dyad, the risks include fetal demise, premature rupture of membranes, oligohydramnios, preterm labor, and preterm birth, with potential complications in subsequent pregnancies for the mother [16, 21]. Many experts in the field, including the Committee on Obstetric Practice of the American College of Obstetricians and Gynecologists, recommend regional concentration of fetal repair to highly skilled centers with the expertise and team-based support systems to provide the highest quality of care for maternal fetal dyads undergoing fetal repair for myelomeningocele [21–23]. For providers who may counsel pregnant women regarding prenatal treatment options, it is important to recognize that the optimal place of care may be at a center relatively far from home. Ethically, it is imperative to provide pregnant women with the information necessary to make an informed decision regarding the option of prenatal repair and the centers that have the best track record with the procedure. This can be politically complicated, as many sites are attempting to build their maternal–fetal medicine programs, and practitioners may feel pressure to refer to a fledging center within their own network.
Another area of controversy is endoscopic patching of myelomeningocele early in pregnancy. The first reported endoscopic repair was conducted in 1997. Endoscopic patch placement is associated with high morbidity and mortality [21, 24, 25]. Since MOMS, and in other countries, there have been attempts to revisit this method [26, 27]. There is no consensus as to when the fetoscopic patch should be placed; the timing may overlap with the timing of open fetal repair. Additionally, patching is not a complete neurosurgical closure. At the time of this writing, endoscopic repair is not recommended until the technique has been perfected in animal models and the procedure can be performed safely [21, 25, 28]. The technique does have promise though. The rationale for in utero intervention is the ‘two-hit hypothesis’ which proposes that the primary lesion is complicated by nervous tissue being exposed to amniotic fluid, trauma, and abnormal hydrodynamic pressure [29, 30]. Earlier repair should help mitigate these secondary complications [31]. Additionally, research in the use of neural stem cells as part of the repair technique is being conducted in animal models with the hope of translating the intervention to humans [32–34]. These interventions represent the next frontier of myelomeningocele care and have the possibility of substantially altering the clinical course for infants born with the condition [32].
Controversies in the neurosurgical management of the infant with spina bifida
There is a fair amount of controversy regarding shunting of cerebral spinal fluid for the infant with myelomeningocele. It has long been reported that 90 % of patients with myelomeningocele develop ventriculomegaly, and 50–85 % of children develop hydrocephalus requiring surgical intervention [8, 35–37]. While shunting has been part of the treatment for hydrocephalus in infants and children with myelomeningocele since the 1950s, there have been considerable shifts in care over the past several decades [38•]. Historically, some centers shunted all babies with myelomeningocele, while, more recently, some centers have opted to shunt in only the most severe cases of hydrocephalus. Hydrocephalus is damaging to the developing brain: it disturbs brain development and delays myelination [39]. Some of the damage may be reversed after shunting, but it is difficult to distinguish clinically or in experimental models which individuals benefit from shunting and when [39]. Unfortunately, infants and children with shunted hydrocephalus experience shunt infections and malfunctions relatively frequently [40]. In the pediatric population, shunt malfunction was the number one reason for hospital admission after 1 year of age [41].
Many centers have attempted to decrease their shunt infection and complication rate by reducing the rate of shunts placed [36, 42, 43•]. Unfortunately, there are no accepted criteria for determining clinically significant hydrocephalus, nor are there adequate clinical prediction rules [39, 44, 45]. At least one center has adopted very rigorous standards for shunt placement, such that shunts are inserted only when the hydrocephalus is severe enough to cause the clinical features of elevated intracranial pressure [46]. Long-term neurocognitive outcome data are not available on their subjects/patients with unshunted hydrocephalus. Given the deleterious consequences of hydrocephalus, even when considered arrested [47, 48], one could hypothesize that these unshunted children will have worse neurocognitive outcomes than their shunted peers, after adjustment for severity and shunt complications in the shunted group. In addition, numerous clinicians and researchers point to the negative neurocognitive profile of children with spina bifida and shunted hydrocephalus as a reason to decrease shunting [38, 44]. However, this logic is flawed because shunting helps ameliorate the effects of hydrocephalus [38, 39], and distinguishing the neurocognitive effects of hydrocephalus itself from the effects of shunt complications is challenging, because studies often consider the presence of a shunt as the indication of hydrocephalus and do not also study individuals with unshunted hydrocephalus [38].
As the field advances, attempts should be made to develop consensus on what represents clinically relevant hydrocephalus, as the consequences of shunt failure or infection can be severe [42, 44]. Similarly, advances in the technique and technology of shunts should be sought to improve outcomes [45]. Instead of creating a goal to decrease shunting rates, the field should seek the data necessary to accurately predict which children would benefit from shunting [45]. Data from MOMS2 may be helpful in determining clinical algorithms. The primary outcome in MOMS included the need for a shunt, and an expert panel was convened prior to MOMS to develop shunting criteria. The criteria used in the MOMS trial were: the presence of marked syringomyelia with ventriculomegaly; or ventriculomegaly with symptoms of Chiari malformation; or persistent cerebral spinal fluid leak or bulging at the repair site; or at least two of the following: crossing centiles without plateauing on head circumference, a bulging fontanelle or split sutures or sunsetting eyes, increased hydrocephalus determined by an increased biventricular to biparietal diameter ratio on consecutive imaging, and/or head circumference >95 % ile for gestational age [16••]. Among the MOMS subjects, these criteria were not routinely applied in the clinical setting. In the postnatally repaired subjects, 92 % met shunting criteria but only 82 % were shunted, while in the prenatally repaired group, 65 % met shunting criteria, but only 40 % were shunted [16••]. This means that subjects with hydrocephalus who were shunted can be compared to subjects with hydrocephalus who were not shunted, and both these subgroups can be compared to those without hydrocephalus.
In addition to the controversy surrounding shunting in general, there remains disagreement about how to stage the primary closure of the lesion with ventriculoperitoneal shunt placement. Simultaneously closing the myelomeningocele lesion and placing a ventriculoperitoneal shunt fell out of favor due to the high rate of shunt infections [49, 50], but offers other benefits such as shorter length of hospital stay and better wound healing at the spina bifida repair site [51]. Recently, centers are returning to this option in a subset of patients to decrease the health care burden of doing sequential procedures [44]. This technique warrants further investigation, as improvements have been made in the mitigation of postoperative infection rates. There is also controversy regarding the use of endoscopic third ventriculostomy as a method to manage hydrocephalus. This technique has fallen in and out of favor over the years [52]. Currently, third ventriculostomy coupled with choroid plexus ablation/coagulation is frequently used in less developed countries where access to neurosurgical care in the face of a shunt malfunction is limited [53]. In the United States, endoscopic third ventriculostomy has much higher failure rate than shunting [54], making it a less than ideal option for managing hydrocephalus. Nonetheless, some studies have shown similar outcomes when compared to standard ventriculoperitoneal shunting [43]. This technique may be offered more frequently if the data support its use.
Management of the adult with myelomeningocele
Medical problems that “fall through the cracks”
Individuals with spina bifida have many health issues that can easily become problematic if there is not a systematic approach to care [9]. Conditions related to aging and inactivity are often underdiagnosed and undertreated, but can lead to serious medical and functional decline. [55] Repetitive strain injuries such as rotator cuff syndrome, osteoporosis [56], obesity, and low levels of physical activity levels are just a few examples [55]. Individuals with spina bifida who are not physically active are more likely to have dyslipidemia and hypertension, be smokers, and be at risk for cardiovascular disease [57]. Obesity in ambulators with spina bifida is also a predictor of future wheelchair use [58].
High blood pressure may affect a significantly higher percentage of young adults with spina bifida than similar age groups in the general population [59]. In a single cohort study, high blood pressure was more prevalent in those with spina bifida who also had a history of diabetes, a history of procedures to treat neurogenic bladder, and renal dysfunction. If sub-optimally treated, high blood pressure can lead to serious events, like stroke. Stroke is responsible for about 3 % of hospital admission of those with spina bifida who are 65+ years old and about 6.5 % of deaths during those hospitalizations [60•]. Another under-addressed cardiovascular issue is lymphedema. We have published a single-site cohort study [61] that evaluated the occurrence rates of lymphedema in our own adult spina bifida population which was over 9 %, 100 times the rate found in general population. Having a clinical diagnosis of lymphedema was found to be significantly associated with a prior history of trauma, cellulitis, cancer, obesity, wounds, high blood pressure, higher lesion level, and wheelchair use.
Healthcare utilization, mortality, cost, and preventable conditions
While prior literature once suggested that the reason for death of adults with spina bifida in many cases was from renal, cardiac, or respiratory complications [62], with improvements in urological management, we have seen a shift in diagnoses responsible for mortality. The mortality rate from unexpected causes for adults with spina bifida is markedly higher than that of adults in the general population [63•]. However, most in-hospital deaths are now thought to be due to potentially preventable conditions [60]. Kinsman et al. [64] published results from a chart review study in 1996 from one US acute care hospital. Individuals with spina bifida were admitted an average of 3.6 times per year, with an average length of stay of 11.2 days. A total of 47 % of those admissions were thought to be due to potentially preventable secondary conditions like urinary tract infection, (UTI), skin breakdown, and osteomyelitis. More current research suggests that skin- and bladder-related infections are the most prominent potentially preventable conditions that are responsible for hospitalizations of adults with spina bifida [60]. Overall, potentially preventable conditions account for about 1/3 of the total hospitalizations of this group. The average number of hospitalizations and 30-day re-admission rates are significantly higher for those with spina bifida than the general population [65]. Another study [66] performed between 2001 and 2003 on a US claims database, which evaluated paid medical and prescription drug claims for individuals with spina bifida with employer-sponsored insurance, showed that medical expenses were found to be 3–6 times higher than the general population [67]. In the US, potentially preventable conditions resulting in hospitalization of those with spina bifida are most common in adults less than 51 years of age and in those treated at rural or urban nonteaching hospital settings [60, 65]. In Canada, where few adults with spina bifida are treated in a medical home model, the statistics are similar [68].
Interventions to improve outcomes of adults
While the multidisciplinary clinic is held as the gold standard of care for individuals with spina bifida, and the way that the majority of children receive care in the US, research to compare different models of care in terms of outcomes in adults is, in fact, lacking. For those who do continue to receive care in pediatric multidisciplinary settings after reaching adulthood, many continue to be treated by pediatric specialists, who may not always be able to care for issues related to aging. In the US, however, the majority of adults with spina bifida are not treated in multidisciplinary settings at all. Many are discharged from pediatric clinics once they reach age 18 or 21 and lose access to all care providers who have expertise in spina bifida care, because most specialists with expertise in this area are affiliated with spina bifida clinics and not providing care independently in the adult provider community. Thus, many adults struggle with trying to piece together specialists who will assume responsibility for parts of their medical care. While a few clinics exclusively for adults do exist, these are rare [69]. Financial, programmatic, and staffing issues challenge survival of the clinics for adults that do exist [70]. These issues of care access may in part explain why so many issues fall through the cracks.
The alarming health care utilization and mortality rates that result from conditions that we should theoretically be able to manage better in an outpatient setting highlight opportunities for interventions that could improve outcomes. The first potential way to intervene is to provide care coordination services [71]. While the evidence is still, in part, qualitative in nature, most caregivers and clinicians believe that, due to the complex medical issues that require a careful and systematic approach to care [72–75], care coordination is an essential for improved outcomes both in the adult and pediatric setting [76–78]. This implies that an adult provider must assume responsibility for being a medical home, or hub of care, that ensures all specialists treating the patient are communicating and that there are no gaps in care. In many cases, a physiatrist may be a suitable provider to coordinate this approach since physiatrists are trained to lead teams involving other disciplines and are alsotrained to deliver care for secondary conditions common in the spina bifida population. Specifically, physiatrists tend to be skilled at managing skin integrity, neurogenic bladder and impairments from secondary conditions of aging. Thus, a physiatrist, especially one who is trained in a pediatric rehabilitation or spinal cord injury fellowship, may be one specialist particularly suited to coordinate a patient’s care [79]. Even in this model, however, other surgical specialists such as urologists, neurosurgeons, and orthopedists who are trained to manage spina bifida related issues are as essential as the primary care physician [73].
Second, a plan for transition of care from a pediatric setting to an adult provider is also crucial [80]. In most cases in the US, the receiving provider would be a primary care physician with limited training in the care of an adult with spina bifida [9, 81]. Therefore, large-scale educational efforts should be made to ensure that providers receive the necessary information about the medical issues typically faced by transitioning young adults with spina bifida and each patient’s individual medical complexities [82]. Resources to aid this transition process were developed by the Spina Bifida Association (SBA).
A third possible intervention is to develop wellness programs that provide care above and beyond what is delivered in the clinics. A pilot program developed at the SBA of Western Pennsylvania (SBAWP) utilized two wellness coordinators (WCs) who were registered nurses who supervised the care of 35 individuals with spina bifida and complex medical needs [83]. The WC designed an individualized plan of care for each person by incorporating the patient’s own goals for wellness and gaps identified in their overall medical care. The WCs promoted patients’ independence in managing skills like scheduling medical appointments, filling prescriptions, and conducting daily self-care activities like catheterization and skin checks for wound. The WCs also conducted home visits, activated community resources, and ensured that all health care providers seeing the patients communicated with each other. The program resulted in shorter lengths of hospital stays, lower admission rates, and lower rates of skin breakdown and UTIs compared to those in the local and national adult spina bifida clinic population, and those served by SBAWP but not in the Wellness Program. Because of the success of the pilot program, a larger version of this program was established at the UPMC Adult Spina Bifida Clinic in conjunction with UPMC Health Plan. This program, directed by a physiatrist, is a specialty home model serving both individuals with spina bifida and also spinal cord injury, and whose outcomes are now being studied in a clinical trial.
In-person Wellness Programs and models of care coordination, however, are challenged by obstacles of patients spread over large geographical distances. Hence, a fourth intervention is to use technological approaches. Many individuals with spina bifida experience problems with executive function and require assistive technology to assist with not only mobility but also self-management and independent living. Mobile health (mHealth) and telerehabilitation approaches can be used to deliver care to underserved patients. We have developed an mHealth system, iMHere (interactive Mobile Health and Rehabilitation) [84]. In this system, patients use smartphone apps geared toward managing common spina bifida-related medical issues. The apps provide reminders to conduct daily self-care activities, and data on problems encountered are transmitted to a secure, web-based portal managed by a clinician. The portal provides a dashboard that allows the clinician to quickly triage patients with urgent needs. The iMHere system allow allows secure, two-way communication between the patients and clinician. In usability testing trials [84, 85], the system was found to be feasible and accessible, and user satisfaction was high. The system is now being studied and enhanced in further clinical and development trials.
The National Spina Bifida Patient Registry
The National Spina Bifida Patient Registry [86•] is a partner program between the Centers for Disease Control (CDC), the SBA, and individual spina bifida clinics in the US. Through planned longitudinal data collection of key outcome variables, and an integrated electronic medical record, the data generated by the registry have become robust, and over time will allow for research to be conducted on larger groups of individuals with spina bifida. This is especially needed to advance research in the care of adults, to determine which medical, surgical, and rehabilitation interventions produce the best outcomes, to compare models of care, and to quickly disseminate research findings into the clinical care of all individuals with spina bifida.
Conclusions
The care of individuals with spina bifida is rapidly advancing. Prenatal and neonatal interventions have the possibility of markedly altering the landscape of myelomeningocele. As treatment options improve prenatally and antenatally, the life expectancy and quality of life for individuals should also improve. As individuals with spina bifida continue to age into adulthood, it is imperative to attend to the medical, functional, and social issues faced by this growing population. The information presented in this manuscript is not intended to function as a review of all of the medical issues and advances in the care of the individual with spina bifida. Instead, our intention is to provide detailed information on a subset of advances, issues, and new knowledge.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Agopian AJ, Canfield MA, Olney RS, et al. Spina bifida subtypes and sub-phenotypes by maternal race/ethnicity in the National Birth Defects Prevention Study. Am J Med Genet Part A. 2012;158A(1):109–15.
• Kim K, Wang Y, Kirby RS, Druschel CM. Prevalence and trends of selected congenital malformations in New York State, 1983 to 2007. Birth Defects Res A Clin Mol Teratol. 2013;97(10):619–627. This paper discusses trends in the birth of children with spina bifida. Racial differences are identified.
Boulet SL, Yang Q, Mai C, et al. Trends in the postfortification prevalence of spina bifida and anencephaly in the United States. Birth Defects Res A. 2008;82(7):527–32.
Forrester MB, Merz RD, Yoon PW. Impact of prenatal diagnosis and elective termination on the prevalence of selected birth defects in Hawaii. Am J Epidemiol. 1998;148(12):1206–11.
Williams LJ, Rasmussen SA, Flores A, Kirby RS, Edmonds LD. Decline in the prevalence of spina bifida and anencephaly by race/ethnicity: 1995–2002. Pediatrics. 2005;116(3):580–6.
• Shin M, Besser LM, Siffel C, et al. Prevalence of Spina bifida among children and adolescents in 10 regions in the United States. Pediatrics. 2010;126(2):274–279. This paper discusses trends in spina bifida in 10 different areas of the country.
Northrup H, Volcik KA. Spina bifida and other neural tube defects. Curr Probl Pediatr. 2000;30(10):313–32.
Davis BE, Daley CM, Shurtleff DB, et al. Long-term survival of individuals with myelomeningocele. Pediatr Neurosurg. 2005;41(4):186–91.
Liptak GS, Garver K, Dosa NP. Spina bifida grown up. J Dev Behav Pediatr. 2013;34(3):206–15.
Bernard JP, Cuckle HS, Bernard MA, Brochet C, Salomon LJ, Ville Y. Combined screening for open spina bifida at 11–13 weeks using fetal biparietal diameter and maternal serum markers. Am J Obstet Gynecol. 2013;209(3):e221–5.
Chao TT, Dashe JS, Adams RC, Keefover-Hicks A, McIntire DD, Twickler DM. Fetal spine findings on MRI and associated outcomes in children with open neural tube defects. Am J Roentgenol. 2011;197(5):W956–61.
Bruner JP, Tulipan N, Paschall RL, et al. Fetal surgery for myelomeningocele and the incidence of shunt-dependent hydrocephalus. JAMA. 1999;282(19):1819–25.
Sutton LN, Adzick NS, Bilaniuk LT, Johnson MP, Crombleholme TM, Flake AW. Improvement in hindbrain herniation demonstrated by serial fetal magnetic resonance imaging following fetal surgery for myelomeningocele. JAMA. 1999;282(19):1826–31.
Hirose S, Farmer DL. Fetal surgery for myelomeningocele. Clin Perinatol. 2009;36(2):431–8.
Farmer DL, von Koch CS, Peacock WJ, et al. In utero repair of myelomeningocele: experimental pathophysiology, initial clinical experience, and outcomes. Arch Surg. 2003;138(8):872–8.
•• Adzick NS, Thom EA, Spong CY, et al. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med. 2011;364(11):993–1004. This manuscript presents the results on the multicentered randomized controlled trial that studied fetal repair for spina bifida versus standard postnatal repair. This study found that fetal surgery was beneficial for reducing the need for shunting.
Danzer E, Gerdes M, Bebbington MW, Koh J, Adzick NS, Johnson MP. Preschool neurobehavioral outcome following fetal myelomeningocele surgery. Fetal Diagn Ther. 2011;30(3):174–9.
Danzer E, Gerdes M, Bebbington MW, Koh J, Adzick SN, Johnson MP. Fetal myelomeningocele surgery: preschool functional status using the Functional Independence Measure for children (WeeFIM). Childs Nerv Syst. 2011;27(7):1083–8.
Simpson JL, Greene MF. Fetal surgery for myelomeningocele? N Engl J Med. 2011;364(11):1076–7.
Hayashi T, Takemoto J, Ochiai T, et al. Surgical indication and outcome in patients with postoperative retethered cord syndrome. J Neurosurg Pediatr. 2013;11(2):133–9.
Meuli M, Moehrlen U. Fetal surgery for myelomeningocele: a critical appraisal. Eur J Pediatr Surg. 2013;23(2):103–9.
van Lith JM, Johnson MP, Wilson RD. Current controversies in prenatal diagnosis 3: fetal surgery after MOMS: is fetal therapy better than neonatal? Prenat Diagn. 2013;33(1):13–6.
American College of O, Gynecologists. ACOG Committee opinion no. 550: maternal-fetal surgery for myelomeningocele. Obstetrics and gynecology. 2013;121(1):218–219.
Kohl T, Hering R, Heep A, et al. Percutaneous fetoscopic patch coverage of spina bifida aperta in the human–early clinical experience and potential. Fetal Diagn Ther. 2006;21(2):185–93.
Shurtleff D. Fetal endoscopic myelomeningocele repair. Dev Med Child Neurol. 2012;54(1):4–5.
Verbeek RJ, Heep A, Maurits NM, et al. Fetal endoscopic myelomeningocele closure preserves segmental neurological function. Dev Med Child Neurol. 2012;54(1):15–22.
Pedreira DA. Keeping it simple: a “two-step” approach for the fetoscopic correction of spina bifida. Surg Endosc. 2010;24(10):2642–3.
Bruner JP, Tulipan NB, Richards WO, Walsh WF, Boehm FH, Vrabcak EK. In utero repair of myelomeningocele: a comparison of endoscopy and hysterotomy. Fetal Diagn Ther. 2000;15(2):83–8.
Heffez DS, Aryanpur J, Hutchins GM, Freeman JM. The paralysis associated with myelomeningocele: clinical and experimental data implicating a preventable spinal cord injury. Neurosurgery. 1990;26(6):987–92.
McLone DG, Knepper PA. The cause of Chiari II malformation: a unified theory. Pediatric Neurosci. 1989;15(1):1–12.
Adzick NS. Fetal surgery for spina bifida: past, present, future. Semin Pediatr Surg. 2013;22(1):10–7.
Dhaulakhandi DB, Rohilla S, Rattan KN. Neural tube defects: review of experimental evidence on stem cell therapy and newer treatment options. Fetal Diagn Ther. 2010;28(2):72–8.
Saadai P, Wang A, Nout YS, et al. Human induced pluripotent stem cell-derived neural crest stem cells integrate into the injured spinal cord in the fetal lamb model of myelomeningocele. J Pediatr Surg. 2013;48(1):158–63.
Saadai P, Farmer DL. Fetal surgery for myelomeningocele. Clin Perinatol. 2012;39(2):279–88.
Dias MS, McLone DG. Hydrocephalus in the child with dysraphism. Neurosurg Clin N Am. 1993;4(4):715–26.
Chakraborty A, Crimmins D, Hayward R, Thompson D. Toward reducing shunt placement rates in patients with myelomeningocele. J Neurosurg Pediatr. 2008;1(5):361–5.
Talamonti G, D’Aliberti G, Collice M. Myelomeningocele: long-term neurosurgical treatment and follow-up in 202 patients. J Neurosurg. 2007;107(5 Suppl):368–86.
• Hampton LE, Fletcher JM, Cirino PT, et al. Hydrocephalus status in spina bifida: an evaluation of variations in neuropsychological outcomes. J Neurosurg Pediatr. 2011;8(3):289–298. This article discusses the impacts of hydrocephalus for children with spina bifida.
Del Bigio MR. Neuropathology and structural changes in hydrocephalus. Dev Disabil Res Rev. 2010;16(1):16–22.
Wu Y, Green NL, Wrensch MR, Zhao S, Gupta N. Ventriculoperitoneal shunt complications in California: 1990 to 2000. Neurosurgery. 2007;61(3):557–62 discussion 562-553.
Houtrow AJ, Maselli JH, Okumura MJ. Inpatient care for children, ages 1–20 years, with spina bifida in the United States. J Pediatr Rehabil Med. 2013;6(2):95–101.
Vinchon M, Dhellemmes P. Cerebrospinal fluid shunt infection: risk factors and long-term follow-up. Childs Nerv Syst. 2006;22(7):692–7.
• Tamburrini G, Frassanito P, Iakovaki K, et al. Myelomeningocele: the management of the associated hydrocephalus. Childs Nerv Syst. 2013;29(9):1569–1579. This paper addresses current issues around shunting for hydrocephalus. There are a lot of opinions about this topic, some of which are presented here.
Wakhlu A, Ansari NA. The prediction of postoperative hydrocephalus in patients with spina bifida. Childs Nerv Syst. 2004;20(2):104–6.
Bowman RM, McLone DG. Neurosurgical management of spina bifida: research issues. Dev Disabil Res Rev. 2010;16(1):82–7.
Sankhla S, Khan GM. Reducing CSF shunt placement in patients with spinal myelomeningocele. J Pediatric Neurosci. 2009;4(1):2–9.
Mataro M, Poca MA, Sahuquillo J, et al. Cognitive changes after cerebrospinal fluid shunting in young adults with spina bifida and assumed arrested hydrocephalus. J Neurol Neurosurg Psychiatry. 2000;68(5):615–21.
Edwards RJ, Pople IK. Long-term outcome of “arrested” hydrocephalus. Eur J Pediatr Surg. 2003;13(Suppl 1):S39–40.
Margaron FC, Poenaru D, Bransford R, Albright AL. Timing of ventriculoperitoneal shunt insertion following spina bifida closure in Kenya. Childs Nerv Syst. 2010;26(11):1523–8.
Arslan M, Eseoglu M, Gudu BO, et al. Comparison of simultaneous shunting to delayed shunting in infants with myelomeningocele in terms of shunt infection rate. Turk Neurosurg. 2011;21(3):397–402.
Miller PD, Pollack IF, Pang D, Albright AL. Comparison of simultaneous versus delayed ventriculoperitoneal shunt insertion in children undergoing myelomeningocele repair. J Child Neurol. 1996;11(5):370–2.
Marlin AE. Management of hydrocephalus in the patient with myelomeningocele: an argument against third ventriculostomy. Neurosurg Focus. 2004;16(2):E4.
Warf BC. Hydrocephalus associated with neural tube defects: characteristics, management, and outcome in sub-Saharan Africa. Childs Nerv Syst. 2011;27(10):1589–94.
Jernigan SC, Berry JG, Graham DA, Goumnerova L. The comparative effectiveness of ventricular shunt placement versus endoscopic third ventriculostomy for initial treatment of hydrocephalus in infants. J Neurosurg Pediatr. 2014.
Klingbeil H, Baer HR, Wilson PE. Aging with a disability. Arch Phys Med Rehabil. 2004;85(7 Suppl 3):S68–73.
Valtonen KM, Goksor LA, Jonsson O, Mellstrom D, Alaranta HT, Viikari-Juntura ER. Osteoporosis in adults with meningomyelocele: an unrecognized problem at rehabilitation clinics. Arch Phys Med Rehabil. 2006;87(3):376–82.
Buffart LM, van den Berg-Emons RJ, Burdorf A, Janssen WG, Stam HJ, Roebroeck ME. Cardiovascular disease risk factors and the relationships with physical activity, aerobic fitness, and body fat in adolescents and young adults with myelomeningocele. Arch Phys Med Rehabil. 2008;89(11):2167–73.
Findley TW, Agre JC, Habeck RV, Schmalz R, Birkebak RR, McNally MC. Ambulation in the adolescent with myelomeningocele. I: early childhood predictors. Arch Phys Med Rehabil. 1987;68(8):518–22.
Stepanczuk BC, Dicianno BE, Webb TS. Young adults with spina bifida may have higher occurrence of prehypertension and hypertension. Am J Physical Med Rehabil Assoc Acad Physiatr. 2013.
• Dicianno BE, Wilson R. Hospitalizations of adults with spina bifida and congenital spinal cord anomalies. Arch Phys Med Rehabil. 2010;91(4):529–535. This paper presents data about the reasons for hospitalization for adults with spina bifida.
Garcia AM, Dicianno BE. The frequency of lymphedema in an adult spina bifida population. Am J Phys Med Rehabil. 2011;90(2):89–96.
Singhal B, Mathew K. Factors affecting mortality and morbidity in adult spina bifida. Eur J Pediatr Surg. 1999;9(S 1):31–2.
• Oakeshott P, Hunt GM, Poulton A, Reid F. Expectation of life and unexpected death in open spina bifida: a 40-year complete, non-selective, longitudinal cohort study. Dev Med Child Neurol. 2010;52(8):749–753. This study looked at life expectancy and dealth among a group of individuals with spina bifida.
Kinsman SL, Doehring MC. The cost of preventable conditions in adults with spina bifida. Eur J Pediatr Surg. 1996;6(S 1):17–20.
Wilson R, Lewis SA, Dicianno BE. Targeted preventive care may be needed for adults with congenital spine anomalies. PMR. 2011;3(8):730–8.
Ouyang L, Grosse SD, Armour BS, Waitzman NJ. Health care expenditures of children and adults with spina bifida in a privately insured US population. Birth Defects Res A. 2007;79(7):552–8.
Ouyang L, Grosse SD, Armour BS, Waitzman NJ. Health care expenditures of children and adults with spina bifida in a privately insured US population. Birth Defects Res A. 2007;79(7):552–8.
Young NL, Anselmo LA, Burke TA, McCormick A, Mukherjee S. Youth and young adults with spina bifida: their utilization of physician and hospital services. Arch Phys Med Rehabil. 2013;95(3):466–71.
http://www.spinabifidaassociation.org/site/c.evKRI7OXIoJ8H/b.8029583/k.C4E9/Clinics.htm. Accessed 1 Dec 2013.
Brei TJ. The future of the multidisciplinary clinic. Sci World J. 2007;7:1752–6.
Kaufman B, Terbrock A, Winters N, Ito J, Klosterman A, Park T. Disbanding a multidisciplinary clinic: effects on the health care of myelomeningocele patients. Pediatr Neurosurg. 1994;21(1):36–44.
Dicianno BE, Kurowski BG, Yang JMJ, et al. Rehabilitation and medical management of the adult with spina bifida. Am J Phys Med Rehabil. 2008;87(12):1027–50.
Walker J, William O. Primary care providers and medical homes for individuals with spina bifida. J Pediatric Rehabil Med. 2008;1(4):337–44.
Webb TS. Medical care of adults with spina bifida. J Pediatric Rehabil Med. 2009;2(1):3–11.
Webb TS. Optimizing health care for adults with spina bifida. Dev Disabil Res Rev. 2010;16(1):76–81.
Brustrom J, Thibadeau J, John L, Liesmann J, Rose S. Care coordination in the spina bifida clinic setting: current practice and future directions. J Pediatric Health Care. 2012;26(1):16–26.
Burke R, Liptak GS. Providing a primary care medical home for children and youth with spina bifida. Pediatrics. 2011;128(6):e1645–57.
Liptak GS, El Samra A. Optimizing health care for children with spina bifida. Dev Disabil Res Rev. 2010;16(1):66–75.
Dicianno BE. 21st Century challenges to the provision of health care to adults with spina bifida: a rehabilitation approach. Arch PMR. In press. 2014.
Binks JA, Barden WS, Burke TA, Young NL. What do we really know about the transition to adult-centered health care? A focus on cerebral palsy and spina bifida. Arch Phys Med Rehabil. 2007;88(8):1064–73.
Sawyer SM, Macnee S. Transition to adult health care for adolescents with spina bifida: research issues. Dev Disabil Res Rev. 2010;16(1):60–5.
Patel MS, O’Hare K. Residency training in transition of youth with childhood-onset chronic disease. Pediatrics. 2010;126(Suppl 3):S190–3.
Dicianno BE PP, Lovelace J, Fairman A, Smyers D, Halgas M, Burkholder K, Boninger ML. Specialty medical homes and wellness services in congenital and acquired spinal cord injury. American Medical Group Association Compendium of Chronic Care Practices. 2013. http://www.amga.org/PI/Collabs/MPMCC/Compendiums/UniversityofPittsburgh.pdf. Accessed 1 Dec 2014.
Parmanto B, Pramana G, Yu DX, Fairman AD, Dicianno BE, McCue MP. iMHere: a novel mhealth system for supporting self-care in management of complex and chronic conditions. J Med Internet Res. 2012;15:277.
Fairman AD, Dicianno BE, Datt N, Garver A, Parmanto B, McCue M. Outcomes of clinicians, caregivers, family members and adults with spina bifida regarding receptivity to use of the iMHere mHealth solution to promote wellness. Int J Telerehabil. 2013.
• Thibadeau JK, Ward EA, Soe MM, et al. Testing the feasibility of a National Spina Bifida Patient Registry. Birth Defects Res A. 2013;97(1):36–41. This paper discusses the feasibility and the creation of the registry funded by the CDC.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Houtrow, A., Dicianno, B.E. Advances in spina bifida care: from the womb to adulthood. Curr Phys Med Rehabil Rep 2, 71–78 (2014). https://doi.org/10.1007/s40141-014-0046-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40141-014-0046-1