Abstract
This study focused on the development of novel coating formulations for stainless steel microneedles against influenza A virus. With in vitro studies, various viscosity enhancers and stabilizers were screened based on the hemagglutination activity of the vaccine, which was coated and dried onto a stainless steel chip at room temperature for 1 day. Following the long-term storage test, the hemagglutination activity and particle size of the vaccine, which was formulated with conventional or methylcellulose or hydroxyethyl cellulose and dried onto the microneedle, were monitored. Next, to evaluate the in vivo immunogenicity and protection effect of each dried vaccine formulation, mice were immunized by the antigen-coated microneedle, which had either the conventional or the proposed formulation. Two novel formulations were chosen in the preliminary screening, and in further evaluations, they exhibited a 20 % higher HA activity during storage for 3 months, and no aggregation was observed during storage after drying. In a mouse model, the microneedle with the novel formulation elicited a higher level of IgG and IgG2a was more prevalent in the IgG isotype profile. In addition, mice immunized with the HEC-coated microneedle survived with small weight loss (>90 %) against lethal challenge infection. Overall, the novel formulation hydroxyethyl cellulose preserved significantly higher HA activity during the production and storage of the microneedle as well as improved the in vivo immunogenicity of the vaccine.
Similar content being viewed by others
Introduction
In 1918–1919, humanity was confronted by the most devastating pandemic, the Spanish flu for the first time. Over 20 to 50 million cases of death caused by this pandemic were estimated around the world, for which the number of victims were threefold higher than the number of victims during World War I [1, 2]. To date, influenza is one of the major public health concerns unlike smallpox and poliomyelitis [3]. Every year, this disease has affected 5 to 15 % of the population in the world [4]. To deal with the disease, antiviral drugs and vaccines have been commercialized and researched to treat infected individuals as well as prevent infection [3]. However, vaccination is the most promising and economic strategy to reduce the damage of seasonal and pandemic influenza, regardless of the remarkable progress of antiviral agents [5–7].
All licensed inactivated influenza vaccines are liquid formulations stored at 2 to 8 °C to preserve their activity against environmental conditions, such as temperature [8]. In the case of temperature, the rate of inactivation for a vaccine is proportional to temperature. Therefore, the vaccine should be transported and stored at 2 to 8 °C using a “cold-chain,” which is an expensive and complicated process. On the other hand, the vaccine, which can be transported and stored at ambient temperature while maintaining its own stability, would reduce the cost caused by cold-chain maintenance and cope with an urgent vaccine distribution in a pandemic situation in western and developing countries [9].
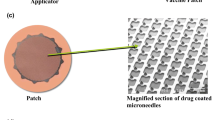
One of vaccine delivery methods which can preserve vaccine stability at ambient temperature is the coated microneedle (MN) due to the dried form of drug on the surface of MN. MNs provide a minimally invasive method to create micron-scale pathways that carry desired drugs into the skin, mainly into the epidermis and dermis [10]. The characteristic of MNs include reduced pain and fear, minimal need by health care personal, and accurate delivery of drugs into the target region. Four types of MNs, solid, hollow, dissolving and coated, have been investigated for drug delivery [11]. This study focused on coated MNs, which involves a solid MN coated with a vaccine formulation delivering the drug into the skin by insertion of the MN and dissolution of the coated antigen [12]. Coating formulations for MNs consist of several excipients, such as a viscosity enhancer sustaining the drug coated on the MN during drying, a surfactant changing the wettability of the MN surface, and a stabilizer preserving the drug from damage caused by drying and storage [11]. Furthermore, those excipients as well as stabilizers are known to effect the stability and activity of the drug [13–19].
Several studies which could improve the vaccine stability in the coating formulation have been introduced. Andrianov et al. showed that poly [di (carboxylatophenoxy) [phosphazene] could be a stabilizer and immunostimulating agent for MN vaccination [19]. Mistilis et al. used a similar stability evaluation method as in our study to find the optimal formulation in terms of the buffer, surfactant, and stabilizer and found that arginine and calcium heptagluconate were the best combination as a stabilizer with CMC in dissolving MNs in vitro [18]. In our previous studies, a coating formulation based on carboxymethylcellulose (CMC) as the viscosity enhancer, Lutrol® F-68 as the surfactant, and trehalose dihydrate as the stabilizer preserved 65 % of the hemagglutinin (HA) activity after the drying process. However, after 5 days, despite the trehalose, the above formulation could only preserve about 40 % of the HA activity at room temperature (RT) [13, 14].
Guided by previous works, in this study, another optimized formulation was found for inactivated influenza virus coated on stainless steel (SS) MNs to achieve stability in long-term storage at room temperature and improved immunogenicity in a mouse model. In the initial screening process, combinations of several viscosity enhancers and stabilizers were evaluated by measuring the HA activity. After the screening, the chosen formulations were further evaluated by measuring the HA activity and particle size during long-term storage at RT. To confirm the availability of the proposed formulations, the model vaccine was coated with either the conventional or the proposed formulations on the SS MNs. Finally, the immunogenicity and protection efficacy of vaccine coated with proposed formulation were investigated in vivo. The new formulation showed significant vaccine stability for 3 months at RT. Moreover, it elicited superior immune responses and protection effects compared with the conventional formulation in the mouse model.
Material and methods
Ethics statement
All animal procedures in this study were approved by the Institutional Animal Care and Use Committee of Konkuk University (permit number: KU16055).
Preparation of inactivated influenza virus
Inactivated influenza virus as a vaccine in this study was kindly provided by Prof. Fushi Quan (Department of Medical Zoology, Kyung Hee University School of Medicine, Seoul, Republic of Korea). Influenza A/PR/8/34 virus was grown in embryonated hen eggs (10 days old). After the growth period, the virus was purified from the allantoic fluid with a discontinuous sucrose gradient (15, 30 and 60 %). The virus was inactivated by formalin at a final concentration of 1:4000 (v/v). To confirm the inactivation of the virus, a plaque assay was done on a confluent monolayer of Madin-Darby canine kidney (MDCK) cells, and another assay was performed by inoculation of the virus into 10-day-old embryonated hen eggs.
Fabrication and coating of the MNs
SS MNs were fabricated by cutting needle structures from SS sheets (SS304, 75 μm thickness, Tech-Etch, Plymouth, MA) using an infrared laser previously described [13]. The length and width at the base of the MNs used in this study were 700 and 160 μm, respectively, and were aligned in a row of five needles per device. SS MNs were dipped into a modified coating device containing the coating formulations previously described [20] and dried at room temperature for 1 day and 1 week, respectively. MNs were dip-coated with several formulations, which were screened presented in Table 1.
Vaccine stability test and size distribution
To evaluate the stability of the inactivated influenza virus, the HA activity was measured to estimate the immunogenicity of the vaccine. Before measuring the HA activity, a mimicked MN coating system, previously suggested [13], was introduced to expose the vaccine to the same environment in which the MN was dried and stored. Briefly, 5 μl of a mixture, consisting of the vaccine and the proposed coating formulation in Table 1, was placed onto 3 mm × 3 mm chips clipped from the SS MNs, and it was dried at room temperature (RT) overnight.
After drying, the SS chips were incubated in PBS (Sigma, St. Louis, MO) for 4 h at 4 °C. Finally, to determine the HA of the inactivated virus coated on the SS chips, 50 μl of the incubated solution was placed in a 96-well plate and serially twofold-diluted. After dilution, 50 μl 0.5 % of chicken red blood cells (RBCs) were added to each well and incubated for 1 h at RT [13]. The endpoint dilutions inhibiting the precipitation of RBCs were used as the titers [21].
A long-term stability study was also done with the same methods described above. This study was conducted for the day points 1, 3, 7, 14, 42, and 84 days after vaccine coating. The results from the HA assay were determined with the same methods described above.
Particle size and size distribution were determined by dynamic light scattering (Zetasizer nano series, Malvern instruments limited, Malvern, USA) with the same one that was used in HA assay and then PBS was added up to 1 ml to adjust to the desired volume for the analysis.
Distribution in porcine skin using coated MNs
To quantitatively and visually check the distribution differences for the provided formulation candidates in the skin, we added fluorescence dye to each coating formulation. Sulforhodamine B (Sigma, St. Louis, MO) and porcine skin were chosen as the model drug and model skin in this experiment. In the case of quantitative analysis, the same mass of sulforhodamine B (1 μg) was coated onto the MN and these were inserted into the porcine skin. The MN was injected and removed after 5, 10, 30, 60, 90, 120, and 300 s. The tips of the MN were cut and incubated in 100 μl of PBS solution. After 1 h, the concentration of dissolved sulforhodamine B in each solution was measured by spectrofluorophotometer (RF-5301, Shimadzu, Kyoto, Japan).
In the case of visual analysis, the porcine skins, which treated with sulforhodamine B-coated MN for 60 s, were frozen in the optimal cutting temperature (OCT) compound (Tissue-Tek, Sakura, Torrance, CA), and cut to a microscale thickness (8–10 μm) using a Cryostat (Cryocut CM3050S, Leica, Bensheim, Germany). Then, the thin skins were collected and placed on slides, and viewed by fluorescence microscope (Leica DM2500, Leica, Bensheim, Germany) [22].
Animal experiments
Six-week female BALB/c mice (Orient Bio, Sungnam, Korea) were prepared and divided into 3 groups (n = 6). The mice in group 1 were immunized by a MN coated with the conventional formulation of CMC (Sigma, St. Louis, MO) 1 % (w/v), trehalose dihydrate (Sigma, St. Louis, MO) 15 % (w/v) and inactivated influenza virus. The mice in group 2 were immunized by a MN coated with the proposed formulation of hydroxyethylcellulose (HEC, Sigma, St. Louis, MO) 0.5 % (w/v), trehalose dihydrate 15 % (w/v) and inactivated influenza virus. Lastly, the mice in group 3 were not immunized (naïve group). The proposed formulation was selected based on in vitro vaccine stability study results. Before immunization, mice were anesthetized with Avertin (375 mg/kg) intraperitoneally. During anesthesia, the fur on the murine back was removed using a depilatory cream (Veet, Reckitt Benckiser, Berkshire, UK). After 5 min, the skin, which was treated with the depilatory cream, was washed by paper tissues with warm water and a soaked cotton ball with 70 % ethanol.
After the fur was removed, the coated MN was manually inserted into the treated site of each mouse in group 1 and 2. After waiting 10 min for complete dissolution of the coating on the MN, the MN was removed from the mice. The mice in the group 3 were not treated with any immunization tool.
After 5 weeks from immunization, all the mice were anesthetized by intraperitoneal injection of Avertin (375 mg/kg) and intranasally infected with a lethal dose of live A/PR/8/34 (H1N1) virus (10× LD50) in 90 μl for the challenge. The weight loss and survival rate of all the mice were recorded for 14 days after challenge. If the mice lost over 25 % of their weight, they were considered dead and humanely euthanized. In this study, the euthanasia was done by cervical dislocation under anesthetic condition. The anesthetic condition was the same as described above.
Serology
To measure the level of virus-specific antibodies in mouse sera, mouse sera collected from all mice at 2 and 4 weeks after immunization were also analyzed by enzyme-linked immunosorbent assay (ELISA). The inactivated antigen, which was the same antigen used in the immunization, was added to 96-well plates (50 μl/well) after dilution (2 μg/ml). The plates were incubated overnight at 4 °C. After the plates were washed with PBS-T (PBS containing 0.05 % Tween 20 (Sigma, St. Louis, MO)), blocking buffer (5 % skim milk powder (Sigma, St. Louis, MO) in PBS-T) was added to the plates (100 μl/well) and the plates were incubated at 37 °C for 1 h. After the plates were washed with PBS-T, the sera, which were twofold diluted to 2.5 % skim milk in PBS-T were added into the plates (50 μl/well), and the plates were incubated at 25 °C for 90 min. After washing with PBS-T, horseradish peroxidase-conjugated anti-mouse IgG, G1, or G2a antibody (Abcam, Cambridge, MA) was added to the plates (100 μl/well). Finally, the substrate, o-Phenylenediamine (Sigma, St. Louis, MO) in a phosphate-citrate buffer (pH 5.0, Sigma, St. Louis, MO) containing H2O2 (Sigma, St. Louis, MO) was added to the plates (100 μl/well) to develop the color. After incubating the plate at RT for 15 min, 1 N hydrochloride acid (100 μl/well) was added to stop the reaction. Lastly, the plates were read with an ELISA reader at 492 nm. End-point titers were defined as the optical density (OD) of the immunized mice sera at the highest dilution factor is greater than twofold the OD of the naïve control at the same dilution factor.
The hemagglutination inhibition (HI) assay was used to detect the presence of functional antibodies which inhibit the hemagglutinin glycoprotein from binding to erythrocytes [23]. The HI assay was done as previously described [24]. Briefly, immunized mouse sera collected at week 2 and 4 after vaccination were treated with a receptor-destroying enzyme (Denka Seiken, Tokyo, Japan). After that, samples were incubated overnight at 37 °C and then for 30 min at 56 °C. After incubation, the samples were serially diluted, and the 4 hemagglutination (HA) unit of the virus was added. And then, an equal volume of 0.5 % chicken red blood cells was added. After 30 min, at RT, the highest serum dilution point preventing HA was scored as the HI titer.
Viscosity of coating formulations
Viscosity of coating formulation was measured using cone and plate viscometer (DV2THB-CP, Brookfield Engineering Laboratories, Stoughton, MA) at 25 °C.
Statistical analysis
All tests done in this paper were measured using at least three replicated samples. The arithmetic mean and standard error of the mean were calculated from all data points and plotted on each graph. Student’s t test was conducted when comparing between two groups. Among multiple groups, a one-way analysis of variance (ANOVA; α = 0.05) was done. A p value less than 0.05 was considered to be significant.
Results
Formulation screening
In previous MN studies, especially on coated MNs, the viscosity enhancer, stabilizer, and surfactant in the coating formulation have been the focus for the dip-coating process, which is a type of coating process for loading desired materials onto solid MNs [20, 24, 25]. However, in some studies, a surfactant was not selected because a coating formulation without a surfactant was successfully dip-coated on a MN [24], or the surfactant had an effect on the virus activity [18]. To confirm whether the HA activity is affected by the surfactant in the proposed formulations, the HA activities were checked for the virus coated on the MNs with the proposed formulations with or without the surfactant Lutrol F68®. The results show that the surfactant had a deleterious effect on the HA activity in most combinations of viscosity enhancers and surfactant (data was not shown) similar to Mistilis et al. [18]. Therefore, all the coating formulations proposed in this study did not contain any surfactant.
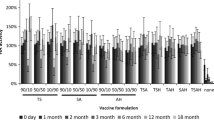
The screening results are shown in Fig. 1 and Table 1. Among the 46 proposed formulations, 30 formulations had a higher HA activity when compared with the conventional formulation (CMC 1 % and trehalose dihydrate 15 %) after storage for 24 h at RT. Among those formulations, two formulations had significantly superior vaccine stability (Student’s t test, p < 0.001): Methylcellulose (MC) 0.5 % with trehalose dihydrate 15 % (91.53 %) and Hydroxyethylcellulose (HEC) 0.5 % with trehalose dihydrate 15 % (91.53 %). In detail, they preserved over 90 % of the HA activity after the drying process, while the conventional formulation preserved only 67.8 % of the HA activity after the drying process. Therefore, these two formulations were used in following experiments.
Screening result of various formulations which was combined with several viscosity enhancers and stabilizer listed in Table 1 and dried on SS chips for 1 day at RT
Long-term stability on a SS chip
To compare the HA activity kinetics during long-term storage with different coating formulations, each combination of vaccine and coating formulation was placed on a SS chip, and stored at RT. As described above, the HA activity of the antigen was checked at 1, 3, 7, 14, 42, and 84 days after coating on the SS chip. As shown in Fig. 2a, the two proposed formulations (MC 88.6, 69.8, 56.3, 59.5, 62.1, and 63.4 HA %; HEC 89.2, 75.0, 58.2, 60.1, 60.8, and 63.4 HA %) preserved 20 to 25 % higher (Student’s t test, p < 0.001) HA activities at all the time points compared with the conventional formulation (64.7, 60.8, 44.6, 40.1, 39.4, and 43.3 HA %). Interestingly, the antigen lost the same amount of HA activity regardless of the formulation during storage at RT.
Stability kinetics of antigen in coatings for 3 months. The vaccine coated with conventional or proposed formulations were dried on SS chips at RT. After 1, 3, 7, 14, 42, and 84 days of storage, the vaccine coated on SS chips were collected. a HA activity and b hydrodynamic diameter changes were measured by HA assay and DLS
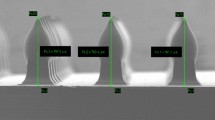
Previous studies have shown that protein aggregation is one of the main reasons for losing viral activity [26, 27]. It is also applicable to whole-inactivated virus [13]. Therefore, using a dynamic light scattering system, the size distribution of antigens that were dissolved from the vaccine-coated SS chip stored for 1, 3, 7, 14, 42, and 84 days post coating was determined. The hydrodynamic diameter was calculated based on the diameter of each particle, so it could be used as an indicator of size distribution. As shown in Fig. 2b, the hydrodynamic diameter ratio (compared with hydrodynamic diameter of control sample) of the antigen with the conventional formulation rapidly increased during first week, while only little change was observed from 1 week to 3 months post-coating. This result corresponds with the result of the HA activity changes. In contrast, the hydrodynamic diameter ratio of the antigen in two proposed formulations hardly increased during 3 months and the values were significantly lower (Student’s t test, p < 0.05) than those of the conventional formulation for all time points. The original size of the inactivated H1N1 virus is around 120 nm [28] and the hydrodynamic diameter ratio of antigen with the conventional formulation was measured around 1.5 after 1 month storage at RT [14]. We assume that higher value was obtained in the current study compared to previous study due to various reasons such as different antigen batch, different antigen concentration, and different storage environment (oxygen level, temperature, humidity, etc). At any rate, we found significant difference in antigen aggregation profile between conventional formulation and proposed formulation.
Coating and releasing experiments using different formulations
Before the in vivo trial, three experiments were done to determine the availability of the proposed coating formulations for practical application. Sulforhodamine B sodium salt was used as a model drug for these experiments. The same number of dip-coatings (9 times) was performed for each MN array using three different coating formulations (the conventional and two proposed formulations), and the mass of sulforhodamine B coated on the MN was measured. As shown in Fig. 3a, the formulation using HEC (2.4 μg) as a viscosity enhancer could load a significantly higher (Student’s t test, p < 0.001) amount of sulforhodamine B on the MN compared with the conventional formulation (1.6 μg). The formulation containing MC (0.3 μg) had a significantly lower (Student’s t test, p < 0.001) amount of sulforhodamine B coated on the MN even when compared with the conventional formulation.
Moreover, whether sulforhodamine B coated on the MN was well distributed in the porcine skin was determined. To compare the same conditions, MNs were prepared, which were coated with the same amount of sulforhodamine B regardless of the coating formulations. The MNs were inserted into the porcine skin and removed after 15, 30, 60, 120, and 300 s. According to the amount of sulforhodamine B remaining on the MN measured by a spectrofluorophotometer, the percentage of sulforhodamine B released into the porcine skin was calculated. As shown in Fig. 3b, the two proposed formulation showed faster releasing profiles up to 2 min than that of the conventional formulation. No sulforhodamine B remained on the MNs removed after 5 min regardless of the coating formulations.
For visual study, fluorescence dye distribution in porcine skin was imaged. For this experiment, each MN was 9 times dip-coated with a fluorescent dye and the conventional formulation, or proposed formulation and dried overnight at RT. After drying, the dye-coated MNs were inserted into the porcine skin for 1 min. As we expected based on the previous experiment, a strong fluorescence was observed from the groups using the formulations containing CMC or HEC. However, the group using the formulation containing MC showed a relatively weak fluorescence in both bright and fluorescent field compared with the other groups (Fig. 4a–f). It was because the MN with the formulation containing MC as a viscosity enhancer had a small amount of fluorescent dye. These results indicate that the formulation containing MC is difficult to use in the practical production of coated MN. Therefore, the formulation containing MC was not used in the following experiments.
Immune responses after vaccination using vaccine coated MNs with different formulations
In the previous in vitro experiments, the formulation containing HEC preserved significantly a higher HA activity during storage at RT. To confirm the correlation between in vitro and in vivo experiments, immune responses and the protection effect were observed in vivo. There were six mice in each group, and the three groups were divided according to the coating formulations (conventional or proposed). Each mouse was immunized with one MN coated with vaccine and the conventional or proposed formulation.
To check the immune response caused by the different formulations, the levels of virus-specific IgG and IgG subtypes level as well as HI activity were measured in the immunized sera collected at 2 and 4 weeks post-vaccination. In Fig. 5a, the proposed formulation induced a higher influenza H1N1 virus-specific IgG antibody response (14,080) than that of the conventional formulation (10,667) at week 4. The influenza virus-specific IgG subtypes could provide further details on the immune responses. The results for the IgG subtypes are shown in Fig. 5b–d. As seen in Fig. 5b, in the case of IgG1, the mice immunized by the MN coated with HEC (0.39) had a higher OD value in sera than the mice immunized by the MN coated with CMC (0.29) at week 4. In the case of IgG2a, the MN with HEC (0.70) also elicited a stronger IgG2a response compared with that coated with the conventional formulation (0.45) at week 4 in Fig. 5c. Using Fig. 5b, c, the IgG2a/IgG1 ratio was calculated and plotted in Fig. 5d. In detail, the IgG2a/IgG1 ratio indicated that the MN induced IgG2a dominant responses (IgG2a/IgG1 > 1). Moreover, the virus coated with HEC showed a strong IgG2a/IgG1 level (2.5) at week 4. A trend similar to the IgG level was observed in Fig. 5e; the MN containing HEC (26.8 and 70.4) elicited a higher HI titer than that containing CMC (7.0 and 40.0) at week 2 and 4, respectively. These results indicate that there is a direct correlation between the immune responses induced by the virus and the HA activity of virus which was coated with proposed formulation on the MN.
Protection against lethal influenza virus challenge after vaccination using MNs with different formulations
To confirm the protective efficiency against influenza virus, the mice immunized by MN with different storage periods and formulations were intranasally challenged against a lethal dose of influenza virus after 5 weeks post-vaccination (Fig. 6a-b). As shown in Fig. 6a, mice immunized by MN with HEC lost their body weight less than those with CMC group. Furthermore, in terms of maximum weight loss, the mice in the group that used CMC as a viscosity enhancer lost about 12 % of their weight (87.4 %) at day 6 after the post challenge dose. However, the mice in the HEC formulation group maintained their body weight by more than 90 % (90.5 %). These results indicate that the mice in the conventional and proposed formulations groups had a sufficient protective effect against lethal challenge. In addition, the HEC formulation group induced a stronger protection effect against the influenza virus compared with the CMC formulation group.
Furthermore, the protective efficiency is also explained based on survival rate described in Fig. 6b. As seen in Fig. 6b, even when a low antigen dose (0.15 μg) was used, all the vaccinated mice in the group with HEC survived against the challenge; however, one mouse in the group with CMC died. Overall, these results suggest that the protection ability in mice immunized by MN against influenza virus was successfully induced in all immunized groups. Moreover, it means that the proposed formulation could completely preserve the immunogenicity of the vaccine during the drying process and showed 100 % protection against lethal challenge compared with the conventional formulation. Taken together, HEC demonstrated promising results in in vivo as well as in vitro studies.
Discussion
These days, skin is an attractive region as an immunization alternative to muscle tissue because it contains many antigen-presenting cells, such as Langerhans cells and dermal dendritic cells [29]. Various types of vaccination tools have been developed aimed at this immune cell-rich organ, such as intradermal injection using traditional equipment, MN, jet injector, and epidermal powder immunization (EPI) [30, 31]. Among these intradermal vaccinations, we focused on MN because this vaccination method has the following advantages: no need for a cold-chain for storage, reduced pain, preference for self-vaccination, safe in terms of needle stick injuries, small volume for storage, no need for highly trained healthcare personnel in case of injection, and reduced adverse events [31–33]. Therefore, due to these characteristics, it could be an ideal vaccination method for seasonal and pandemic influenza [18]. However, few formulations have been reported for preserving the vaccine stability in coated MNs in ambient condition like at RT. Therefore, we tested various candidate formulations with combinations of viscosity enhancers and stabilizers to find the optimal formulation and to improve the stability of vaccine-coated MNs.
In our previous study, we reported that trehalose is the best stabilizer for influenza vaccine when the formulation included CMC as a viscosity enhancer due to its own chemical structure and characteristics [13]. However, Choi et al. showed that trehalose crystallization and phase separation generated in the virus-coated film could have an adverse effect on virus stability while the addition of CMC as a viscosity enhancer enhanced the virus stability during drying [15, 16]. In another paper, Mistilis et al. screened various kinds of materials to find an MN formulation with thermostability focusing on dissolving MNs. Therefore, we found several viscosity enhancers and stabilizer candidates from the above and additional papers [18, 34–42] and made a list for combinations of several viscosity enhancers and stabilizers. To increase the viscosity during the dip-coating process, cellulose (MC, HEC), a natural viscosity enhancer (pectin, carrageenan and gelatin), and a high molecular weight polymer (glycol chitosan and polyvinylpyrrolidone (PVP)) were chosen as candidates for the viscosity enhancer. Additionally, mono-, di-, and tri-saccharides and some amino acids (trehalose, maltose, raffinose, lactose, maltodextrin, dextran, mannose and arginine) were chosen as vaccine stabilizers.
First, we preliminarily screened each combination on the list by measuring the HA activity of the vaccine in each formulation dried on a SS chip at RT for 1 day previously described [13]. We choose the HA assay as the screening method because the HA assay is a simple and fast evaluation method for measuring the function of the influenza HA protein which is a major surface glycoprotein found in influenza for immunity and a target of infectivity-neutralizing antibodies [43–45]. Therefore, the HA activity was mainly used to evaluate the activity of the influenza vaccine in previous studies [13, 14].
Among 46 candidates, 30 formulations preserved a higher HA activity than that of the conventional formulation (CMC 1 % and trehalose 15 %) after drying (storage for 1 day at RT), shown in Fig. 1, in agreement with data obtained from Kim et al. [14]. Moreover, the best two formulations (F1: MC 0.5 % and trehalose 15 %; F2: HEC 0.5 % and trehalose 15 %) preserved more than 90 % of the HA activity after drying. For in-depth screening, particle size was added as another factor in the long-term stability test because aggregation is one of the main reasons for destabilization of proteins and associated with loss of HA activity [9, 14]. In the long-term stability experiments, the two proposed formulations preserved over 60 % of the HA activity during 3 months of storage, and this was a significantly improved (Student’s t test, p < 0.05) result compared with the conventional formulation. Moreover, from another aspect, to check the stability kinetics during production and long-term storage, we determined the hydrodynamic diameter by DLS as the size distribution of the antigen coated on the MN after 1, 3, 7, 14, 42, and 84 days of storage. As seen in the Fig. 2b, the hydrodynamic diameter ratio of the antigen in the coating with the conventional formulation was significantly increased while that of the antigen in the coating with the two proposed formulations was only slightly increased during production and maintained during storage at RT for 3 months. The correlation between aggregation and HA activity was not clearly demonstrated in Fig. 2; thus, particle size could be used as a criterion of vaccine stability; however, other factors such as denaturation, loss of HA conformation, hydrolysis, and oxidation could affect vaccine stability [9]. Taken together, these results indicate that the antigen in the coating with the novel formulations was significantly stable during production and storage at RT for 3 months.
To confirm the practicality of the proposed formulations in a practical coating process, we simulated those combinations with a dip-coating method using sulforhodamine B as a model drug. From the results (Fig. 3 and Fig. 4), the coating formulation containing MC was eliminated from the following experiments because the amount of the model drug in MC coated on MNs was much lower than those in the other two formulations coated on the MNs, and the distribution of the model drug with MC in porcine skin showed a weaker fluorescence signal compared with the other two groups. The other novel formulation containing HEC was chosen due to loading a significantly higher amount of sulforhodamine B on the MN compared with the conventional formulation and its similar drug distribution after insertion into porcine skin as the conventional one.
In Gill and Prausnitz, actual trials in the coating process with candidates on SS MN need to determine the proper materials for the dip-coating process. Some factors applied to the dip-coating process such as viscosity and surface tension of each viscosity enhancer could be explained [12]. In this trial, the thickness of the coating parts with MC observed in each dip-coating turn was thinner than the thickness of the coating parts with other formulations correlating with Fig. 3a. However, one of the factors, the viscosity of the formulation with MC and trehalose (9.64 cP), is higher than the viscosity of the formulation with CMC and trehalose (7.37 cP). Therefore, other factors such as surface tension or material characteristic could affect the dip-coating process. Taken together, HEC was chosen as the best viscosity enhancing excipient in the coating formulation for MN production using the dip-coating process.
To confirm the correlation between vaccine stability and immunogenicity, mice were immunized by vaccine-coated MNs with the conventional or proposed formulation. In the serological results, the HEC formulation group showed higher (Supplementary 1) immune responses in the HI titer, IgG, and IgG subtypes. Moreover, in protection efficacy, all the mice in the HEC formulation group survived and maintained their own body weight by more than 90 %; however, one of the vaccinated mice in the conventional formulation group died after challenge. Overall, these results indicate that the mice in all groups elicited sufficient immunogenic protection against a lethal virus; however, the HEC formulation group showed the best protection efficacy against the lethal influenza virus.
These results could be due to the material characteristic of HEC such as the viscosity. It has been reported that a higher viscosity in a coating formulation could preserve vaccine stability during the drying process [46]. In this paper, we changed CMC (5.49 and 7.37 cP with trehalose) to HEC (11.7 and 14.8 cP with trehalose) which is a higher viscous cellulose derivative than that of CMC and does not decrease the viral HA activity as described in this paper. Therefore, its material characteristics could affect the virus activity during the production and drying phase. However, as seen in Table 1, the chemical characteristic except for viscosity could also affect the virus activity.
Taken together, we suggest HEC as an alternative viscosity enhancer for the coating formulation in the production of coated MNs with the influenza vaccine. The antigen with HEC and trehalose protected 60 % of the HA activity during long-term storage and did not show further aggregation after the production process compared with the conventional formulation. Moreover, it is more practical in the dip-coating process compared with the other candidate. In addition, the vaccine coated and dried with HEC and trehalose on SS MNs exhibited a better immune response and protection efficacy than that with the conventional formulation. Overall, HEC is a suitable viscosity enhancer for coated microneedles fabricated by the dip-coating process, based on in vitro and in vivo trials and practicality tests. Further studies are needed for various vaccines or therapeutic proteins available for MNs as well as in vivo tests and additional screening for various types of materials.
Conclusion
Intradermal vaccination is one of the attractive delivery routes for vaccination which may provide a dose-sparing effect and better protective immunity [25, 47]. However, administration of traditional liquid form vaccines is unreliable and difficult [48]. Moreover, liquid vaccines should be stored and transported in a cold-chain to maintain their stability. Therefore, MNs could be one alternative for traditional vaccine delivery systems because vaccine-coated MNs can be stockpiled and carried without a cold-chain. In this study, HEC, as a viscosity enhancer, improved the stability of the vaccine-coated MN compared with the formulation using CMC. HEC was able to preserve the viral HA activity and inhibit aggregation during long-term storage. Moreover, the formulation with HEC was more suitable than the formulation with other candidate in dip-coating process in terms of practicality. In addition, mice immunized with the virus-coated MN with HEC showed improved immunogenicity and protective potential. Additional experiments are needed for optimizing the formulation, screening with more wide-ranging excipients, and determining the mechanistic basis for these stabilizing effects.
References
Trilla A, Trilla G, Daer C. The 1918 “Spanish flu” in Spain. Clin Infect Dis. 2008;47(5):668–73.
Holmes EC. 1918 and all that. Science. 2004;303:5665–1787.
Palese P. Influenza: old and new threats. Nat Med. 2004;10:S82–S7.
WHO: Influenza fact sheet No. 211, revised March 2003. See: www.who.int/mediacentre/factsheets/fs211/en/print.html (2003). Accessed 24 May 2005.
Osterholm MT, Kelley NS, Sommer A, Belongia EA. Efficacy and effectiveness of influenza vaccines: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(1):36–44.
Cox R, Brokstad K, Ogra P. Influenza virus: immunity and vaccination strategies. Comparison of the immune response to inactivated and live, attenuated influenza vaccines. Scand J Immunol. 2004;59(1):1–15.
Nichol KL, Lind A, Margolis KL, Murdoch M, McFadden R, Hauge M, et al. The effectiveness of vaccination against influenza in healthy, working adults. N Engl J Med. 1995;333(14):889–93.
Kristensen D. Summary of stability data for licensed vaccines. PATH: Seattle; 2012.
Amorij J, Huckriede A, Wilschut J, Frijlink H, Hinrichs W. Development of stable influenza vaccine powder formulations: challenges and possibilities. Pharm Res. 2008;25(6):1256–73.
Prausnitz MR. Microneedles for transdermal drug delivery. Adv Drug Del Rev. 2004;56(5):581–7.
Kim Y-C, Park J-H, Prausnitz MR. Microneedles for drug and vaccine delivery. Adv Drug Del Rev. 2012;64(14):1547–68.
Gill HS, Prausnitz MR. Coating formulations for microneedles. Pharm Res. 2007;24(7):1369–80.
Kim Y-C, Quan F-S, Compans RW, Kang S-M, Prausnitz MR. Formulation and coating of microneedles with inactivated influenza virus to improve vaccine stability and immunogenicity. J Control Release. 2010;142(2):187–95.
Kim Y-C, Quan F-S, Compans RW, Kang S-M, Prausnitz MR. Stability kinetics of influenza vaccine coated onto microneedles during drying and storage. Pharm Res. 2011;28(1):135–44.
Choi H-J, Yoo D-G, Bondy BJ, Quan F-S, Compans RW, Kang S-M, et al. Stability of influenza vaccine coated onto microneedles. Biomaterials. 2012;33(14):3756–69.
Choi H-J, Bondy BJ, Yoo D-G, Compans RW, Kang S-M, Prausnitz MR. Stability of whole inactivated influenza virus vaccine during coating onto metal microneedles. J Control Release. 2013;166(2):159–71.
Andrianov AK, Marin A, DeCollibus DP. Microneedles with intrinsic immunoadjuvant properties: microfabrication, protein stability, and modulated release. Pharm Res. 2011;28(1):58–65.
Mistilis MJ, Bommarius AS, Prausnitz MR. Development of a thermostable microneedle patch for influenza vaccination. J Pharm Sci. 2015;104(2):740–9.
Andrianov AK, Decollibus DP, Marin A, Webb A, Griffin Y, Webby RJ. PCPP-formulated H5N1 influenza vaccine displays improved stability and dose-sparing effect in lethal challenge studies. J Pharm Sci. 2011;100(4):1436–43.
Gill HS, Prausnitz MR. Coated microneedles for transdermal delivery. J Control Release. 2007;117(2):227–37.
Hierholzer JC, Suggs MT. Standardized viral hemagglutination and hemagglutination-inhibition tests. I. Standardization of erythrocyte suspensions. Appl Microbiol. 1969;18(5):816–23.
Lee JW, Park J-H, Prausnitz MR. Dissolving microneedles for transdermal drug delivery. Biomaterials. 2008;29(13):2113–24.
Klausberger M, Wilde M, Palmberger D, Hai R, Albrecht RA, Margine I, et al. One-shot vaccination with an insect cell-derived low-dose influenza A H7 virus-like particle preparation protects mice against H7N9 challenge. Vaccine. 2014;32(3):355–62.
Kim Y-C, Yoso D-G, Compans RW, Kang S-M, Prausnitz MR. Cross-protection by co-immunization with influenza hemagglutinin DNA and inactivated virus vaccine using coated microneedles. J Controlled Release. 2013;172(2):579–88
Shin J-H, Park J-K, Lee D-H, Quan F-S, Song C-S, Kim Y-C. Microneedle vaccination elicits superior protection and antibody response over intranasal vaccination against swine-origin influenza A (H1N1) in mice. PLoS One. 2015;10(6):e0130684.
Ghosh R, Sharma S, Chattopadhyay K. Effect of arginine on protein aggregation studied by fluorescence correlation spectroscopy and other biophysical methods†. Biochemistry. 2009;48(5):1135–43.
Jain NK, Roy I. Effect of trehalose on protein structure. Protein Sci. 2009;18(1):24–36.
Noda T, Sagara H, Yen A, Takada A, Kida H, Cheng RH, et al. Architecture of ribonucleoprotein complexes in influenza A virus particles. Nature. 2006;439(7075):490–2.
Skountzou I, Kang S-M. Transcutaneous immunization with influenza vaccines. Vaccines for pandemic influenza. Springer; 2009. p. 347–68.
Kim Y-C, Jarrahian C, Zehrung D, Mitragotri S, Prausnitz M. Delivery systems for intradermal vaccination. Intradermal immunization. Springer; 2011. p. 77–112.
Quan F-S, Kim Y-C, Yoo D-G, Compans RW, Prausnitz MR, Kang S-M. Stabilization of influenza vaccine enhances protection by microneedle delivery in the mouse skin. PLoS One. 2009;4(9):e7152.
Norman JJ, Arya JM, McClain MA, Frew PM, Meltzer MI, Prausnitz MR. Microneedle patches: usability and acceptability for self-vaccination against influenza. Vaccine. 2014;32(16):1856–62.
Arya J, Prausnitz MR. Microneedle patches for vaccination in developing countries. J Controlled Release. 2015. doi:10.1016/j.jconrel.2015.11.019.
Chen X, Prow TW, Crichton ML, Jenkins DW, Roberts MS, Frazer IH, et al. Dry-coated microprojection array patches for targeted delivery of immunotherapeutics to the skin. J Control Release. 2009;139(3):212–20.
Chen J, Qiu Y, Zhang S, Yang G, Gao Y. Controllable coating of microneedles for transdermal drug delivery. Drug Dev Ind Pharm. 2015;41(3):415–22.
Demir YK, Kerimoglu O. Novel use of pectin as a microneedle base. Chem Pharm Bull. 2015;63(4):300–4.
Ling M-H, Chen M-C. Dissolving polymer microneedle patches for rapid and efficient transdermal delivery of insulin to diabetic rats. Acta Biomater. 2013;9(11):8952–61.
Lee ES, Park K-H, Park IS, Na K. Glycol chitosan as a stabilizer for protein encapsulated into poly (lactide-co-glycolide) microparticle. Int J Pharm. 2007;338(1):310–6.
Kim YC, Quan FS, Yoo DG, Compans RW, Kang SM, Prausnitz MR. Enhanced memory responses to seasonal H1N1 influenza vaccination of the skin with the use of vaccine-coated microneedles. J Infect Dis. 2010;201(2):190–8. doi:10.1086/649228.
Mano J, Silva G, Azevedo HS, Malafaya P, Sousa R, Silva S, et al. Natural origin biodegradable systems in tissue engineering and regenerative medicine: present status and some moving trends. J R Soc Interface. 2007;4(17):999–1030.
Sasahara K, McPhie P, Minton AP. Effect of dextran on protein stability and conformation attributed to macromolecular crowding. J Mol Biol. 2003;326(4):1227–37.
Cheshire M. Origins and stability of soil polysaccharide. J Soil Sci. 1977;28(1):1–10.
Eisfeld AJ, Neumann G, Kawaoka Y. Influenza A virus isolation, culture and identification. Nat Protoc. 2014;9(11):2663–81.
Skehel JJ, Wiley DC. Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annu Rev Biochem. 2000;69(1):531–69.
DuBois RM, Aguilar-Yañez JM, Mendoza-Ochoa GI, Oropeza-Almazán Y, Schultz-Cherry S, Alvarez MM, et al. The receptor-binding domain of influenza virus hemagglutinin produced in Escherichia coli folds into its native, immunogenic structure. J Virol. 2011;85(2):865–72.
Choi H-J, Song J-M, Bondy BJ, Compans RW, Kang S-M, Prausnitz MR. Effect of osmotic pressure on the stability of whole inactivated influenza vaccine for coating on microneedles. PLoS One. 2015;10(7):e0134431.
Kim Y-C, Quan F-S, Yoo D-G, Compans RW, Kang S-M, Prausnitz MR. Improved influenza vaccination in the skin using vaccine coated microneedles. Vaccine. 2009;27(49):6932–8.
Lambert PH, Laurent PE. Intradermal vaccine delivery: will new delivery systems transform vaccine administration? Vaccine. 2008;26(26):3197–208.
Acknowledgments
This study was financially supported by grants of the Korean Health Technology R & D Project, the Ministry of Health & Welfare (Project number: HI13C0826), the KUSTAR-KAIST Institute at KAIST, Animal Disease Management Technology Development Program (Grant number: 313013-3), Ministry of Agriculture, Food and Rural Affairs, and the Ministry of Science, ICT, and Future Planning (Project number: NRF- 2014M3A9E4064580) in Republic of Korea. We appreciate Dr. Quan for providing PR8 influenza vaccine.
* All institutional and national guidelines for the care and use of laboratory animals were followed.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Seong-Jin Kim and Ju-Hyung Shin contributed equally to this work.
Electronic supplementary material
Supplementary 1
The results of serology in mice at week 2 and 4 using the microneedles after 1 week storage (DOC 44 kb)
Rights and permissions
About this article
Cite this article
Kim, SJ., Shin, JH., Noh, JY. et al. Development of the novel coating formulations for skin vaccination using stainless steel microneedle. Drug Deliv. and Transl. Res. 6, 486–497 (2016). https://doi.org/10.1007/s13346-016-0321-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-016-0321-z