Abstract
Purpose
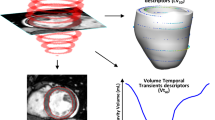
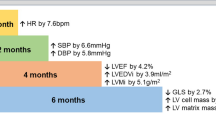
Patient-specific models of the heart can be used to improve the diagnosis of cardiac diseases, but practical application of these models can be impeded by the computational costs and numerical uncertainties of fitting mechanistic models to clinical measurements from individual patients. Reliable and efficient tuning of these models within clinically appropriate error bounds is a requirement for practical deployment in the time-constrained environment of the clinic.
Methods
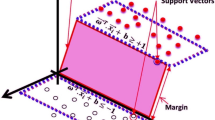
We developed an optimization framework to tune parameters of patient-specific mechanistic models using routinely-acquired non-invasive patient data more efficiently than manual methods. We employ a hybrid particle swarm and pattern search optimization algorithm, but the framework can be readily adapted to use other optimization algorithms.
Results
We apply the proposed framework to tune full-cycle lumped parameter circulatory models using clinical data. We show that our framework can be easily adapted to optimize cross-species models by tuning the parameters of the same circulation model to four canine subjects.
Conclusions
This work will facilitate the use of biomechanics and circulatory cardiac models in both clinical and research environments by ameliorating the tedious process of manually fitting the parameters.








Similar content being viewed by others
References
Aguado-Sierra J., A. Krishnamurthy, C. Villongco, J. Chuang, E. Howard, M. J. Gonzales, J. Omens, D. E. Krummen, S. Narayan, R. C. P. Kerckhoffs, and A. D. McCulloch. Patient-specific modeling of dyssynchronous heart failure: a case study. Prog. Biophys. Mol. Biol. 107(1):147–155, 2011.
Arts, T., T. Delhaas, P. Bovendeerd, X. Verbeek, and F. W. Prinzen. Adaptation to mechanical load determines shape and properties of heart and circulation: the CircAdapt model. Am. J. Physiol. 288:H1943–H1954, 2005.
Augustin, C. M., A. Crozier, A. Neic, Prassl AJ, Karabelas E, Ferreira da Silva T, Fernandes JF, Campos F, Kuehne T, and G. Plank. Patient-specific modeling of left ventricular electromechanics as a driver for haemodynamic analysis. Europace 18:iv121–iv129, 2016.
Baillargeon, B., N. Rebelo, D. D. Fox, R. L. Taylor, and E. Kuhl. The Living Heart Project: a robust and integrative simulator for human heart function. Eur. J. Mech. 48:38–47, 2014.
Balaban, G., M. S. Alnæs, J. Sundnes, and M. E. Rognes. Adjoint multi-start-based estimation of cardiac hyperelastic material parameters using shear data. Biomech. Model. Mechanobiol. 15(6), 1509–1521, 2016.
Bols, J., J. Degroote, B. Trachet, B. Verhegghe, P. Segers, and J. Vierendeels. A computational method to assess the in vivo stresses and unloaded configuration of patient-specific blood vessels. J. Comput. Appl. Math. 246:10–17, 2013.
Camara, O., T. Mansi, M. Pop, K. Rhode, M. Sermesant, and A. Young (eds). Statistical Atlases and Computational Models of the Heart: Imaging and Modelling Challenges. New York: Springer, 2014
Carapella, V., S. A. Niederer, P. Lamata, M. J. Bishop, J. E. Schneider, P. Kohl, and V. Grau. Images as drivers of progress in cardiac computational modelling. Prog. Biophys. Mol. Biol. 115:198–212, 2014.
Chabiniok, R., P. Moireau, P. F. Lesault, A. Rahmouni, J. F. Deux, and D. Chapelle. Estimation of tissue contractility from cardiac cine-MRI using a biomechanical heart model. Biomech. Model. Mechanobiol. 11(5), 609–630, 2012.
Chabiniok, R., V. Y. Wang, M. Hadjicharalambous, L. Asner, J. Lee, M. Sermesant, E. Kuhl, A. A. Young, P. Moireau, M. P. Nash, D. Chapelle, D. A. Nordsletten, and L. Mall. Multiphysics and multiscale modelling , data—model fusion and integration of organ physiology in the clinic : ventricular cardiac mechanics. Interface Focus, 2016. https://doi.org/10.1098/rsfs.2015.0083
Clay, S., K. Alfakih, A. Radjenovic, T. Jones, J. P. Ridgway, and M. U. Sinvananthan. Normal range of human left ventricular volumes and mass using steady state free precession MRI in the radial long axis orientation. Mag. Resonance Mater. Phys. Biol. Med. 19(1), 41–45, 2006.
CMRG. Continuity 6.4, 2015.
Ellwein, L. M., S. R. Pope, A. Xie, J. Batzel, C. T. Kelley, and M. S. Olufsen. Modeling cardiovascular and respiratory dynamics in congestive heart failure. Math. Biosci. 241:56–74, 2013.
Ennis, D. B. Assessment of Myocardial Structure and Function Using Magnetic Resonance Imaging. PhD thesis, Johns Hopkins University, 2004
Hadjicharalambous, M., L. Asner, R. Chabiniok, E. Sammut, J. Wong, D. Peressutti, E. Kerfoot, A. King, J. Lee, R. Razavi, N. Smith, G. Carr-White, and D. Nordsletten. Non-invasive model-based assessment of passive left-ventricular myocardial stiffness in healthy subjects and in patients with non-ischemic dilated cardiomyopathy. Ann. Biomed. Eng. 45(3): 605–618, 2017.
Heusinkveld, M., K. Reesink, T. Arts, W. Huberts, and T. Delhaas. Use of vascular adaptation in response to mechanical loading facilitates personalisation of a one-dimensional pulse wave propagation model. Artery Res. 20:79–80, 2009.
Holzapfel, G. A., and R. W. Ogden Constitutive modelling of passive myocardium: a structurally based framework for material characterization. Philos. Trans. R. Soc. Ser. A 367(1902):3445–3475, 2009.
Hooke, R., and T. A. Jeeves. “Direct search” solution of numerical and statistical problems. J. ACM 8(2):212–229, 1961.
Institute of Laboratory Animal Resources (ILAR). Guide for the Care and Use of Laboratory Animals. Washington, D.C.: National Academies Press, 1996
Kerckhoffs, R. C. P., J. Lumens, K. Vernooy, J. H. Omens, L. J. Mulligan, T. Delhaas, T. Arts, A. D. McCulloch, and F. W. Prinzen. Cardiac resynchronization: insight from experimental and computational models. Prog. Biophys. Mol. Biol. 97(2–3), 543–561, 2008.
Klotz, S., I. Hay, M. L. Dickstein, G. H. Yi, J. Wang, M. S. Maurer, D. A. Kass, and D. Burkhoff. Single-beat estimation of end-diastolic pressure-volume relationship: a novel method with potential for noninvasive application. Am. J. Physiol. 291(1):H403–H412, 2006.
Kovalova, S., J. Necas, and J. Vespalec. What is a “normal” right ventricle? Eur. J. Echocardiogr. 7(4):293–297, 2006.
Krishnamurthy, A., B. Coppola, J. Tangney, R. C. P. Kerckhoffs, J. H. Omens, and A. D. McCulloch. A microstructurally based multi-scale constitutive model of active myocardial mechanics. In: Structure-Based Mechanics of Tissues and Organs. New York: Springer, chap 3, pp. 439–460, 2016.
Krishnamurthy, A., C. Villingco, A. Beck, J. Omens, and A. McCulloch. Left ventricular diastolic and systolic material property estimation from image data: LV mechanics challenge. Stat. Atlases Comput. Model. Heart 8896:63–73, 2015.
Krishnamurthy, A., C. T. Villongco, J. Chuang, L. R. Frank, V. Nigam, E. Belezzuoli, P. Stark, D. E. Krummen, S. Narayan, J. H. Omens, A. D. McCulloch, R. C. P. Kerckhoffs. Patient-specific models of cardiac biomechanics. J. Comput. Phys. 244:4–21, 2013.
Lang, R. M., M. Bierig, R. B. Devereux, F. A. Flachskampf, E. Foster, P. A. Pellikka, M. H. Picard, M. J. Roman, J. Seward, J. Shanewise, S. Solomon, K. T. Spencer, M. St John Sutton, and W. Stewart. Recommendations for chamber quantification. Eur. J. Echocardiogr. 7(2):79–108, 2006.
Lim, E., S. Dokos, N. H. Lovell, S. L. Cloherty, R. F. Salamonsen, D. G. Mason, and J. A. Reizes. Parameter-optimized model of cardiovascular-rotary blood pump interactions. IEEE Trans. Biomed. Eng. 57(2):254–266, 2010.
Marchesseau, S., H. Delingette, M. Sermesant, and N. Ayache. Fast parameter calibration of a cardiac electromechanical model from medical images based on the unscented transform. Biomech. Model. Mechanobiol. 12(4), 815–831, 2013.
MathWorks. MATLAB R2017b, 2017
More, J. J., and S. M. Wild. Benchmarking derivative-free optimization algorithms. SIAM J. Optim. 39:2, 2009.
Nasopoulou, A., A. Shetty, J. Lee, D. Nordsletten, C. A. Rinaldi, P. Lamata, and S. Niederer. Improved identifiability of myocardial material parameters by an energy-based cost function. Biomech. Model. Mechanobiol. 16(3), 971–988, 2017.
Nauser, T. D., and S. W. Stites. Diagnosis and treatment of pulmonary hypertension. Am. Family Phys. 63(9):1789–1798, 2001.
Neal, M. L., and J. B. Bassingthwaighte. Subject-specific model estimation of cardiac output and blood volume during hemorrhage. Cardiovasc. Eng. 7(3):97–120, 2007.
Niederer, S. A., M. Fink, D. Noble, and N. P. Smith. A meta-analysis of cardiac electrophysiology computational models. Exp. Physiol. 94(5):486–495, 2009.
Piper, M. A., C. V. Evans, B. U. Burda, K. L. Margolis, E. O’Connor, and E. P. Whitlock. Diagnostic and predictive accuracy of blood pressure screening methods with consideration of rescreening intervals: a systematic review for the U.S. Preventive Services Task Force. Ann. Int. Med. 162(3):192–204, 2015.
Raamat, R., J. Talts, K. Jagomägi, and J. Kivastik. Accuracy of some algorithms to determine the oscillometric mean arterial pressure: a theoretical study. Blood Press. Monit. 18:50–56, 2013.
Sellier, M. An iterative method for the inverse elasto-static problem. J. Fluid. Struct. 27(8):1461–1470, 2011.
Shi, Y., and R. Eberhart. A modified particle swarm optimizer. In: IEEE International Conference on Evolutionary Computation, pp. 69–73, 1998.
Shortliffe, E. H., B. G. Buchanan, and E. A. Feigenbaum. Knowledge engineering for medical decision making: a review of computer-based clinical decision aids. Tech. Rep., Stanford University Computer Science Department, 1979.
Tange, O. GNU parallel---the command-line power tool. login USENIX Mag. 36(1):42–47, 2011
Vaz, A. I. F., and L. N. Vicente. A particle swarm pattern search method for bound constrained global optimization. J. Glob. Optim. 39(2):197–219, 2007.
Wang, V. Y., H. I. Lam, D. B. Ennis, B. R. Cowan, A. A. Young, and M. P. Nash. Modelling passive diastolic mechanics with quantitative MRI of cardiac structure and function. Med. Image Anal. 13(5):773–784, 2009.
Wang, V. Y., P. M. F. Nielsen, and M. P. Nash. Image-based predictive modeling of heart mechanics. Ann. Rev. Biomed. Eng. 17:351–383, 2015.
Xi, J., P. Lamata, S. Niederer, S. Land, W. Shi, X. Zhuang, S. Ourselin, S. G. Duckett, A. K. Shetty, C. A. Rinaldi, D. Rueckert, R. Razavi, and N. P. Smith. The estimation of patient-specific cardiac diastolic functions from clinical measurements. Med. Image Anal. 17(2):133–146, 2013.
Yoshimura, M., H. Yasue, K. Okumura, H. Ogawa, M. Jougasaki, M. Mukoyama, K. Nakao, and H. Imura. Different secretion patterns of atrial natriuretic peptide and brain natriuretic peptide in patients with congestive heart failure. Circulation 87(2):464–469, 1993.
Zoghbi, W. A. Quantifying valvular regurgitation. In: ACC Middle East Conference, 2016.
Funding
This research was supported in part by the National Biomedical Computation Resource, NIH Grant 8 P41 GM103426-21 (Amaro and McCulloch), by the UC Center for Accelerated Innovation under NIH Grant 4 U54 HL11-9893, NIH Grant 1 R01 HL131753 (Segars, Krishnamurthy, McCulloch), by NSF Grant 1750865 (Krishnamurthy), and by the Joseph C. and Elizabeth A. Anderlik Professorship at Iowa State University (Mineroff). We would also like to show our gratitude to Dr. Judy Vance at Iowa State University for her extraordinary support.
Conflict of interest
Andrew D. McCulloch is a co-founder, equity holders and scientific advisory board member of Insilicomed Inc. and Vektor Medical, licensees of UCSD software used in this research. This relationship has been disclosed to the University of California San Diego and is overseen by an independent conflict of interest management subcommittee appointed by the university. Joshua Mineroff, David Krummen, Baskar Ganapathysubramanian, and Adarsh Krishnamurthy have declared that no competing interests exist.
Ethical Approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Alison Marsden and Ajit P. Yoganathan oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mineroff, J., McCulloch, A.D., Krummen, D. et al. Optimization Framework for Patient-Specific Cardiac Modeling. Cardiovasc Eng Tech 10, 553–567 (2019). https://doi.org/10.1007/s13239-019-00428-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-019-00428-z