Abstract
Introduction
In the mitral valve (MV), numerous pathological factors, especially those resulting from changes in external loading, have been shown to affect MV structure and composition. Such changes are driven by the MV interstitial cell (MVIC) population via protein synthesis and enzymatic degradation of extracellular matrix (ECM) components.
Methods
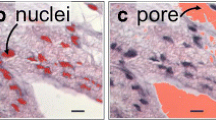
While cell phenotype, ECM composition and regulation, and tissue level changes in MVIC shape under stress have been studied, a detailed understanding of the three-dimensional (3D) microstructural mechanisms are lacking. As a first step in addressing this challenge, we applied focused ion beam scanning electron microscopy (FIB-SEM) to reveal novel details of the MV microenvironment in 3D.
Results
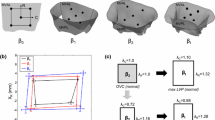
We demonstrated that collagen is organized into large fibers consisting of an average of 605 ± 113 fibrils, with a mean diameter of 61.2 ± 9.8 nm. In contrast, elastin was organized into two distinct structural subtypes: (1) sheet-like lamellar elastin, and (2) circumferentially oriented elastin struts, based on both the aspect ratio and transmural tilt. MVICs were observed to have a large cytoplasmic volume, as evidenced by the large mean surface area to volume ratio 3.68 ± 0.35, which increased under physiological loading conditions to 4.98 ± 1.17.
Conclusions
Our findings suggest that each MVIC mechanically interacted only with the nearest 3–4 collagen fibers. This key observation suggests that in developing multiscale MV models, each MVIC can be considered a mechanically integral part of the local fiber ensemble and is unlikely to be influenced by more distant structures.











Similar content being viewed by others
References
Ali, M. S., X. Wang, and C. M. Lacerda. A survey of membrane receptor regulation in valvular interstitial cells cultured under mechanical stresses. Exp. Cell Res. 351(2):150–156, 2017.
Ayoub, S., G. Ferrari, R. C. Gorman, J. H. Gorman, F. J. Schoen, and M. S. Sacks. Heart valve biomechanics and underlying mechanobiology. Compr. Physiol. 6(4):1743–1780, 2016.
Ayoub, S., C.-H. Lee, K. H. Driesbaugh, W. Anselmo, C. T. Hughes, G. Ferrari, R. C. Gorman, J. H. Gorman, and M. S. Sacks. Regulation of valve interstitial cell homeostasis by mechanical deformation: implications for heart valve disease and surgical repair. J. R. Soc. Interface 14(135):20170580, 2017.
Balachandran, K., P. W. Alford, J. Wylie-Sears, J. A. Goss, A. Grosberg, J. Bischoff, E. Aikawa, R. A. Levine, and K. K. Parker. Cyclic strain induces dual-mode endothelial-mesenchymal transformation of the cardiac valve. Proc. Natl. Acad. Sci. USA 108(50):19943–19948, 2011.
Balachandran, K., S. Konduri, P. Sucosky, H. Jo, and A. Yoganathan. An ex vivo study of the biological properties of porcine aortic valves in response to circumferential cyclic stretch. Ann. Biomed. Eng. 34(11):1655–1665, 2006.
Balachandran, K., P. Sucosky, H. Jo, and A. P. Yoganathan. Elevated cyclic stretch alters matrix remodeling in aortic valve cusps: implications for degenerative aortic valve disease. Am. J. Physiol. Heart Circ. Physiol. 296(3):H756–H764, 2009.
Bloodworth, C. H., E. L. Pierce, T. F. Easley, A. Drach, A. H. Khalighi, M. Toma, M. O. Jensen, M. S. Sacks, and A. P. Yoganathan. Ex vivo methods for informing computational models of the mitral valve. Ann. Biomed. Eng. 45(2):496–507, 2017.
Buchanan, R. M., and M. S. Sacks. Interlayer micromechanics of the aortic heart valve leaflet. Biomech. Model. Mechanobiol. 3(4):813–826, 2013.
Bushby, A. J., K. M. P’ng, R. D. Young, C. Pinali, C. Knupp, and A. J. Quantock. Imaging three-dimensional tissue architectures by focused ion beam scanning electron microscopy. Nat. Protoc. 6(6):845–858, 2011.
Carruthers, C. A., B. Good, A. D’Amore, J. Liao, R. Amini, S. C. Watkins, and M. S. Sacks. Alterations in the microstructure of the anterior mitral valve leaflet under physiological stress. In: ASME 2012 Summer Bioengineering Conference. American Society of Mechanical Engineers, Fajardo, Puerto Rico, 2012, pp. 227–228
Cole, W. G., D. Chan, A. J. Hickey, and D. E. Wilcken. Collagen composition of normal and myxomatous human mitral heart valves. Biochem. J. 219(2):451–460, 1984.
Dal-Bianco, J. P., E. Aikawa, J. Bischoff, J. L. Guerrero, M. D. Handschumacher, S. Sullivan, B. Johnson, J. S. Titus, Y. Iwamoto, J. Wylie-Sears, R. A. Levine, and A. Carpentier. Active adaptation of the tethered mitral valve: insights into a compensatory mechanism for functional mitral regurgitation. Circulation 120(4):334–342, 2009.
Dal-Bianco, J. P., E. Aikawa, J. Bischoff, J. L. Guerrero, J. Hjortnaes, J. Beaudoin, C. Szymanski, P. E. Bartko, M. M. Seybolt, M. D. Handschumacher, S. Sullivan, M. L. Garcia, A. Mauskapf, J. S. Titus, J. Wylie-Sears, W. S. Irvin, M. Chaput, E. Messas, A. A. Hagege, A. Carpentier, and R. A. Levine. Myocardial infarction alters adaptation of the tethered mitral valve. J. Am. Coll. Cardiol. 67(3):275–287, 2016.
De Winter, D. A., C. T. Schneijdenberg, M. N. Lebbink, B. Lich, A. J. Verkleij, M. R. Drury, and B. M. Humbel. Tomography of insulating biological and geological materials using focused ion beam (FIB) sectioning and low-kV BSE imaging. J. Microsc. 233(3):372–383, 2009.
Denk, W., and H. Horstmann. Serial block-face scanning electron microscopy to reconstruct three-dimensional tissue nanostructure. PLoS Biol. 2(11):e329, 2004.
Drach, A., A. H. Khalighi, and M. S. Sacks. A comprehensive pipeline for multi-resolution modeling of the mitral valve: Validation, computational efficiency, and predictive capability. Int. J. Numer. Method. Biomed. Eng. 34(2):e2921, 2018.
Dunkman, A. A., M. R. Buckley, M. J. Mienaltowski, S. M. Adams, S. J. Thomas, A. Kumar, D. P. Beason, R. V. Iozzo, D. E. Birk, and L. J. Soslowsky. The injury response of aged tendons in the absence of biglycan and decorin. Matrix Biol. 2013. https://doi.org/10.1016/j.matbio.2013.10.008.
Dunkman, A. A., M. R. Buckley, M. J. Mienaltowski, S. M. Adams, S. J. Thomas, L. Satchell, A. Kumar, L. Pathmanathan, D. P. Beason, and R. V. Iozzo. Decorin expression is important for age-related changes in tendon structure and mechanical properties. Matrix Biol. 32(1):3–13, 2013.
Giannuzzi, L. A., D. Phifer, N. J. Giannuzzi, and M. J. Capuano. Two-dimensional and 3-dimensional analysis of bone/dental implant interfaces with the use of focused ion beam and electron microscopy. J. Oral Maxillofac. Surg. 65(4):737–747, 2007.
Go, A. S., D. Mozaffarian, V. L. Roger, E. J. Benjamin, J. D. Berry, M. J. Blaha, S. Dai, E. S. Ford, C. S. Fox, S. Franco, H. J. Fullerton, C. Gillespie, S. M. Hailpern, J. A. Heit, V. J. Howard, M. D. Huffman, S. E. Judd, B. M. Kissela, S. J. Kittner, D. T. Lackland, J. H. Lichtman, L. D. Lisabeth, R. H. Mackey, D. J. Magid, G. M. Marcus, A. Marelli, D. B. Matchar, D. K. McGuire, E. R. Mohler, 3rd, C. S. Moy, M. E. Mussolino, R. W. Neumar, G. Nichol, D. K. Pandey, N. P. Paynter, M. J. Reeves, P. D. Sorlie, J. Stein, A. Towfighi, T. N. Turan, S. S. Virani, N. D. Wong, D. Woo, and M. B. Turner. Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation 129(3):e28–e292, 2014.
Grande-Allen, K. J., B. P. Griffin, N. B. Ratliff, D. M. Cosgrove, and I. Vesely. Glycosaminoglycan profiles of myxomatous mitral leaflets and chordae parallel the severity of mechanical alterations. J. Am. Coll. Cardiol. 42(2):271–277, 2003.
Grande-Allen, K. J., and J. Liao. The heterogeneous biomechanics and mechanobiology of the mitral valve: implications for tissue engineering. Curr. Cardiol. Rep. 13(2):113–120, 2011.
Gupta, V., H. Tseng, B. D. Lawrence, and K. J. Grande-Allen. Effect of cyclic mechanical strain on glycosaminoglycan and proteoglycan synthesis by heart valve cells. Acta Biomater. 5(2):531–540, 2009.
Hekking, L. H., M. N. Lebbink, D. A. De Winter, C. T. Schneijdenberg, C. M. Brand, B. M. Humbel, A. J. Verkleij, and J. A. Post. Focused ion beam-scanning electron microscope: exploring large volumes of atherosclerotic tissue. J. Microsc. 235(3):336–347, 2009.
Heymann, J. A., D. Shi, S. Kim, D. Bliss, J. L. Milne, and S. Subramaniam. 3D imaging of mammalian cells with ion-abrasion scanning electron microscopy. J. Struct. Biol. 166(1):1–7, 2009.
Huang, H. Y., J. Liao, and M. S. Sacks. In-situ deformation of the aortic valve interstitial cell nucleus under diastolic loading. J. Biomech. Eng. 129(6):880–889, 2007.
Khalighi, A. H., A. Drach, C. H. T. Bloodworth, E. L. Pierce, A. P. Yoganathan, R. C. Gorman, J. H. Gorman, 3rd, and M. S. Sacks. Mitral valve chordae tendineae: topological and geometrical characterization. Ann. Biomed Eng. 45(2):378–393, 2017.
Khalighi, A. H., A. Drach, R. C. Gorman, J. H. Gorman, and M. S. Sacks. Multi-resolution geometric modeling of the mitral heart valve leaflets. Biomech Model Mechanobiol 17(2):351–366, 2018.
Khalighi, A. H., A. Drach, F. M. ter Huurne, C.-H. Lee, C. Bloodworth, E. L. Pierce, M. O. Jensen, A. P. Yoganathan, and M. S. Sacks. A comprehensive framework for the characterization of the complete mitral valve geometry for the development of a population-averaged model. In: Functional Imaging and Modeling of the Heart: 8th International Conference, FIMH 2015, Maastricht, The Netherlands, June 25–27, edited by H. van Assen, P. Bovendeerd, T. Delhaas. Proceedings, Springer International Publishing, Cham, 2015, pp. 164–171.
Kizilyaprak, C., J. Daraspe, and B. M. Humbel. Focused ion beam scanning electron microscopy in biology. J. Microsc. 254(3):109–114, 2014.
Lamers, E., X. F. Walboomers, M. Domanski, G. McKerr, B. M. O’Hagan, C. A. Barnes, L. Peto, R. Luttge, L. A. Winnubst, H. J. Gardeniers, and J. A. Jansen. Cryo DualBeam focused ion beam-scanning electron microscopy to evaluate the interface between cells and nanopatterned scaffolds. Tissue Eng Part C 17(1):1–7, 2011.
Lanir, Y. Constitutive equations for fibrous connective tissues. J. Biomech. 16(1):1–12, 1983.
Lee, C. H., C. A. Carruthers, S. Ayoub, R. C. Gorman, J. H. Gorman, 3rd, and M. S. Sacks. Quantification and simulation of layer-specific mitral valve interstitial cells deformation under physiological loading. J. Theor. Biol. 373:26–39, 2015.
Lee, C.-H., and M. S. Sacks. Fibers to organs: how collagen fiber properties modulate the closing behavior of the mitral valve. In: Structure-Based Mechanics of Tissues and Organs, edited by G. S. Kassab, and M. S. Sacks. Boston: Springer, 2016, pp. 365–381.
Lee, C.-H., W. Zhang, K. Feaver, R. C. Gorman, J. H. Gorman, and M. S. Sacks. On the in vivo function of the mitral heart valve leaflet: insights into tissue–interstitial cell biomechanical coupling. Biomech. Model. Mechanobiol. 16(5):1613–1632, 2017.
Lee, C. H., W. Zhang, J. Liao, C. A. Carruthers, J. I. Sacks, and M. S. Sacks. On the presence of affine fibril and fiber kinematics in the mitral valve anterior leaflet. Biophys. J. 108(8):2074–2087, 2015.
Leser, V., M. Milani, F. Tatti, Z. P. Tkalec, J. Strus, and D. Drobne. Focused ion beam (FIB)/scanning electron microscopy (SEM) in tissue structural research. Protoplasma 246(1–4):41–48, 2010.
Levine, R. A., A. A. Hagege, D. P. Judge, M. Padala, J. P. Dal-Bianco, E. Aikawa, J. Beaudoin, J. Bischoff, N. Bouatia-Naji, P. Bruneval, J. T. Butcher, A. Carpentier, M. Chaput, A. H. Chester, C. Clusel, F. N. Delling, H. C. Dietz, C. Dina, R. Durst, L. Fernandez-Friera, M. D. Handschumacher, M. O. Jensen, X. P. Jeunemaitre, H. L. Marec, T. L. Tourneau, R. R. Markwald, J. Merot, E. Messas, D. P. Milan, T. Neri, R. A. Norris, D. Peal, M. Perrocheau, V. Probst, M. Puceat, N. Rosenthal, J. Solis, J. J. Schott, E. Schwammenthal, S. A. Slaugenhaupt, J. K. Song, and M. H. Yacoub. Mitral valve disease-morphology and mechanisms. Nat. Rev. Cardiol. 12(12):689–710, 2015.
Lidke, D. S., and K. A. Lidke. Advances in high-resolution imaging–techniques for three-dimensional imaging of cellular structures. J Cell Sci 125(11):2571–2580, 2012.
Medeiros, L. C., W. De Souza, C. Jiao, H. Barrabin, and K. Miranda. Visualizing the 3D architecture of multiple erythrocytes infected with Plasmodium at nanoscale by focused ion beam-scanning electron microscopy. PLoS ONE 7(3):e33445, 2012.
Merryman, W. D., H. D. Lukoff, R. A. Long, G. C. Engelmayr, Jr, R. A. Hopkins, and M. S. Sacks. Synergistic effects of cyclic tension and transforming growth factor-beta1 on the aortic valve myofibroblast. Cardiovasc. Pathol. 16(5):268–276, 2007.
Murphy, G. E., K. Narayan, B. C. Lowekamp, L. M. Hartnell, J. A. Heymann, J. Fu, and S. Subramaniam. Correlative 3D imaging of whole mammalian cells with light and electron microscopy. J. Struct. Biol. 176(3):268–278, 2011.
Nalla, R. K., A. E. Porter, C. Daraio, A. M. Minor, V. Radmilovic, E. A. Stach, A. P. Tomsia, and R. O. Ritchie. Ultrastructural examination of dentin using focused ion-beam cross-sectioning and transmission electron microscopy. Micron 36(7–8):672–680, 2005.
Narayan, K., and S. Subramaniam. Focused ion beams in biology. Nat Methods 12(11):1021, 2015.
O’Connell, M. K., S. Murthy, S. Phan, C. Xu, J. Buchanan, R. Spilker, and C. A. Taylor. The three-dimensional micro- and nanostructure of the aortic medial lamellar unit measured using 3D confocal and electron microscopy imaging. Matrix Biol. 27(3):171–181, 2008.
Peddie, C. J., and L. M. Collinson. Exploring the third dimension: volume electron microscopy comes of age. Micron 61:9–19, 2014.
Rabkin, E., M. Aikawa, J. R. Stone, Y. Fukumoto, P. Libby, and F. J. Schoen. Activated interstitial myofibroblasts express catabolic enzymes and mediate matrix remodeling in myxomatous heart valves. Circulation 104(21):2525–2532, 2001.
Rabkin-Aikawa, E., M. Farber, M. Aikawa, and F. J. Schoen. Dynamic and reversible changes of interstitial cell phenotype during remodeling of cardiac valves. J Heart Valve Dis 13(5):841–847, 2004.
Raspanti, M., M. Reguzzoni, M. Protasoni, and D. Martini. Evidence of a discrete axial structure in unimodal collagen fibrils. Biomacromolecules 12(12):4344–4347, 2011.
Rego, B. V., S. Ayoub, A. H. Khalighi, A. Drach, R. Gorman, J. Gorman, and M. S. Sacks. Alterations in mechanical properties and in vivo geometry of the mitral valve following myocardial infarction. In: Proceedings of the 2017 Summer Biomechanics, Bioengineering and Biotransport Conference, pp. SB3C2017-1, 2017.
Rego, B. V., A. H. Khalighi, A. Drach, E. K. Lai, A. M. Pouch, R. C. Gorman, J. H. Gorman, and M. S. Sacks. A non-invasive method for the determination of in vivo mitral valve leaflet strains. Int. J. Numer. Method. Biomed. Eng. (in press)
Rego, B. V., and M. S. Sacks. A functionally graded material model for the transmural stress distribution of the aortic valve leaflet. J. Biomech. 54:88–95, 2017.
Rego, B. V., S. M. Wells, C. H. Lee, and M. S. Sacks. Mitral valve leaflet remodelling during pregnancy: insights into cell-mediated recovery of tissue homeostasis. J. R. Soc. Interface 13(125):20160709, 2016.
Reznikov, N., R. Almany-Magal, R. Shahar, and S. Weiner. Three-dimensional imaging of collagen fibril organization in rat circumferential lamellar bone using a dual beam electron microscope reveals ordered and disordered sub-lamellar structures. Bone 52(2):676–683, 2013.
Robinson, P. S., K. A. Derwin, R. V. Iozzo, L. J. Soslowsky, T. W. Lin, and P. R. Reynolds. Strain-rate sensitive mechanical properties of tendon fascicles from mice with genetically engineered alterations in collagen and decorin. J. Biomech. Eng. 126(2):252–257, 2004.
Robinson, P. S., T.-F. Huang, E. Kazam, R. V. Iozzo, L. J. Soslowsky, and D. E. Birk. Influence of decorin and biglycan on mechanical properties of multiple tendons in knockout mice. J. Biomech. Eng. 127(1):181–185, 2005.
Ruggeri, A., F. Reale, and E. Benazzo. Collagen fibrils with straight and helicoidal microfibrils: a freeze-fracture and thin-section study. J. Ultrastruct. Res. 68(1):101–108, 1979.
Sacks, M. S., A. Khalighi, B. Rego, S. Ayoub, and A. Drach. On the need for multi-scale geometric modelling of the mitral heart valve. Healthc. Technol Lett 4(5):150, 2017.
Sacks, M. S., W. D. Merryman, and D. E. Schmidt. On the biomechanics of heart valve function. J. Biomech. 42(12):1804–1824, 2009.
Sacks, M. S., and A. P. Yoganathan. Heart valve function: a biomechanical perspective. Philos. Trans. R. Soc. Lond. B 363(1502):2481, 2008.
Schertel, A., N. Snaidero, H. M. Han, T. Ruhwedel, M. Laue, M. Grabenbauer, and W. Mobius. Cryo FIB-SEM: volume imaging of cellular ultrastructure in native frozen specimens. J. Struct. Biol. 184(2):355–360, 2013.
Schneider, P., M. Meier, R. Wepf, and R. Muller. Towards quantitative 3D imaging of the osteocyte lacuno-canalicular network. Bone 47(5):848–858, 2010.
Schneider, P., M. Meier, R. Wepf, and R. Muller. Serial FIB/SEM imaging for quantitative 3D assessment of the osteocyte lacuno-canalicular network. Bone 49(2):304–311, 2011.
Schoen, F. Aortic valve structure-function correlations: role of elastic fibers no longer a stretch of the imagination. J. Heart Valve Dis. 6:1–6, 1997.
Scott, M., and I. Vesely. Aortic valve cusp microstructure: the role of elastin. Ann. Thorac. Surg. 60:S391–S394, 1995.
Scott, M. J., and I. Vesely. Morphology of porcine aortic valve cusp elastin. J Heart Valve Dis. 5(5):464–471, 1996.
Starborg, T., N. S. Kalson, Y. Lu, A. Mironov, T. F. Cootes, D. F. Holmes, and K. E. Kadler. Using transmission electron microscopy and 3View to determine collagen fibril size and three-dimensional organization. Nat. Protoc. 8(7):1433–1448, 2013.
Stella, J. A., and M. S. Sacks. On the biaxial mechanical properties of the layers of the aortic valve leaflet. J. Biomech. Eng. 129(5):757–766, 2007.
Stephens, E., C. Durst, J. Swanson, K. J. Grande-Allen, N. Ingels, Jr, and D. C. Miller. Functional coupling of valvular interstitial cells and collagen via α2β1 integrins in the mitral leaflet. Cell. Mol. Bioeng. 3(4):428–437, 2010.
Taylor, P. M., P. Batten, N. J. Brand, P. S. Thomas, and M. H. Yacoub. The cardiac valve interstitial cell. Int. J. Biochem. Cell Biol. 35(2):113–118, 2003.
Thayer, P., K. Balachandran, S. Rathan, C. H. Yap, S. Arjunon, H. Jo, and A. P. Yoganathan. The effects of combined cyclic stretch and pressure on the aortic valve interstitial cell phenotype. Ann. Biomed. Eng. 39(6):1654–1667, 2011.
Timmermans, F. J., and C. Otto. Contributed review: Review of integrated correlative light and electron microscopy. Rev. Sci. Instrum. 86(1):011501, 2015.
Titze, B., and C. Genoud. Volume scanning electron microscopy for imaging biological ultrastructure. Biol. Cell 108(11):307–323, 2016.
Upton, M. L., J. Chen, F. Guilak, and L. A. Setton. Differential effects of static and dynamic compression on meniscal cell gene expression. J. Orthop. Res. 21(6):963–969, 2003.
Vesely, I. The role of elastin in aortic valve mechanics. J. Biomech. 31(2):115–123, 1998.
Weinberg, E. J., and M. R. K. Mofrad. A multiscale computational comparison of the bicuspid and tricuspid aortic valves in relation to calcific aortic stenosis. J. Biomech. 41(16):3482–3487, 2008.
Weinberg, E. J., D. Shahmirzadi, and M. R. K. Mofrad. On the multiscale modeling of heart valve biomechanics in health and disease. Biomech. Modeling Mechanobiol. 9(4):373–387, 2010.
Zaefferer, S., S. I. Wright, and D. Raabe. Three-dimensional orientation microscopy in a focused ion beam-scanning electron microscope: a new dimension of microstructure characterization. Metall. Mater. Trans. A 39(2):374–389, 2008.
Zhang, W., S. Ayoub, J. Liao, and M. S. Sacks. A meso-scale layer-specific structural constitutive model of the mitral heart valve leaflets. Acta Biomater. 32:238–255, 2015.
Acknowledgments
The authors would like to acknowledge Dr. Hua Gua (Rice University) and Dr. Dwight Romanovicz (UT Austin) for their assistance with the FIB-SEM and TEM instruments, as well as Sarah Poletti, Ethan Kwan, and Michelle Lu for their assistance with heart valve tissue isolation and preparation. This work was supported by the National Institutes of Health Grant [R01HL119297] to MSS and the American Heart Association Pre-Doctoral Fellowship [PRE33420135] to SA.
Conflict of interest
None of the authors of this work, Salma Ayoub, Karen C. Tsai, Amir H. Khalighi, and Michael S. Sacks, have a conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animal studies performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Michael R. King oversaw the review of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Video 1. Video of the 3D reconstruction of the mitral valve interstitial cell and its surrounding microenvironment showing the serial 2D FIB-SEM images (horizontal field width of 53.6 µm), followed by the 3D reconstruction of the nucleus, cytoplasm, collagen, and elastin. This video highlights the complexity of the interconnection between the valve interstitial cell and the surrounding extracellular matrix. Reconstruction of 77 serial sections (total thickness = 15.4 µm) with a slice thickness of 200 nm. Supplementary material 1 (MP4 102833 kb)
Video 2. Video of the 3D reconstruction of the mitral valve interstitial microenvironment showing the serial 2D FIB-SEM images (horizontal field width of 20.7 µm), followed by the 3D reconstruction of the collagen fibers and the elastin structures. Reconstruction of 30 serial sections (total thickness = 1.50 µm) with a slice thickness of 50 nm. Supplementary material 2 (MP4 94609 kb)
Rights and permissions
About this article
Cite this article
Ayoub, S., Tsai, K.C., Khalighi, A.H. et al. The Three-Dimensional Microenvironment of the Mitral Valve: Insights into the Effects of Physiological Loads. Cel. Mol. Bioeng. 11, 291–306 (2018). https://doi.org/10.1007/s12195-018-0529-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12195-018-0529-8