Abstract
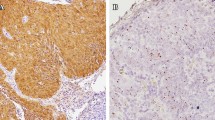
The lungs are a common site of metastasis of head and neck (H&N) squamous cell carcinomas (SCC). This study attempts to define p16 immunoexpression and presence of HPV in primary SCC of the lung and determine their usefulness in discriminating between primary lung SCC and metastasis from HPV-associated oropharyngeal primary. Pathology archives were searched for patients with SCC of the lung without SCC elsewhere. Tissue microarray was constructed and immunohistochemistry performed using anti-p40 and anti-p16 antibodies. All cases were tested for HPV viral proteins E6/E7 by RNA in situ hybridization (ISH) and available positive cases for HPV DNA by polymerase chain reaction (PCR). Eight of 25 (32%) showed cytoplasmic and nuclear expression of p16: 2 (8%) strong and 2 (8%) moderate in > 70% of tumor cells; 1 (4%) strong, 1 (4%) moderate, and 1 (4%) weak in 50–70% of tumor cells; 1 (4%) weak in < 50% of tumor cells. E6/E7 mRNA ISH was negative in all cases. Seven of 8 (87.5%) p16-expressing cases were available for testing by HPV PCR; all were negative for HPV DNA. A retrospective control group of 12 patients with possible SCC metastatic to lung was also identified; high-risk HPV DNA was present in 3, confirming metastasis. p16 expression in lung SCC is not uncommon and may not discriminate between primary pulmonary SCC and metastasis from HPV-associated oropharyngeal primary. Confirmatory HPV testing (high risk HPV DNA or E6/E7 mRNA) is recommended to differentiate metastasis from oropharyngeal primary from two separate primaries.


Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
Casiraghi M, De Pas T, Maisonneuve P, Brambilla D, Ciprandi B, Galetta D, et al. A 10-year single-center experience on 708 lung metastasectomies: the evidence of the "international registry of lung metastases". J Thoracic Oncol. 2011;6(8):1373–8. https://doi.org/10.1097/JTO.0b013e3182208e58.
Duprez F, Berwouts D, De Neve W, Bonte K, Boterberg T, Deron P, et al. Distant metastases in head and neck cancer. Head Neck. 2017;39(9):1733–43. https://doi.org/10.1002/hed.24687.
WHO classification of tumours of the lung, pleura, thymus, and heart. Lyon: 2015.
Trosman SJ, Koyfman SA, Ward MC, Al-Khudari S, Nwizu T, Greskovich JF, et al. Effect of human papillomavirus on patterns of distant metastatic failure in oropharyngeal squamous cell carcinoma treated with chemoradiotherapy. JAMA Otolaryngol Head Neck Surg. 2015;141(5):457–62. https://doi.org/10.1001/jamaoto.2015.136.
Wiegand S, Zimmermann A, Wilhelm T, Werner JA. Survival after distant metastasis in head and neck cancer. Anticancer Res. 2015;35(10):5499–502.
Goldstraw P, Chansky K, Crowley J, Rami-Porta R, Asamura H, Eberhardt WE, et al. The IASLC lung cancer staging project: proposals for revision of the TNM stage groupings in the forthcoming (Eighth) edition of the TNM classification for lung cancer. J Thoracic Oncol. 2016;11(1):39–51. https://doi.org/10.1016/j.jtho.2015.09.009.
Lewis JS Jr, Beadle B, Bishop JA, Chernock RD, Colasacco C, Lacchetti C, et al. Human papillomavirus testing in head and neck carcinomas: guideline from the College of American Pathologists. Arch Pathol Lab Med. 2018;142(5):559–97. https://doi.org/10.5858/arpa.2017-0286-CP.
Fakhry C, Lacchetti C, Rooper LM, Jordan RC, Rischin D, Sturgis EM, et al. Human papillomavirus testing in head and neck carcinomas: ASCO clinical practice guideline endorsement of the college of american pathologists guideline. J Clin Oncol. 2018;36(31):3152–61. https://doi.org/10.1200/jco.18.00684.
Esposito V, Baldi A, Tonini G, Vincenzi B, Santini M, Ambrogi V, et al. Analysis of cell cycle regulator proteins in non-small cell lung cancer. J Clin Pathol. 2004;57(1):58–63. https://doi.org/10.1136/jcp.57.1.58.
Lewis JS Jr. Human papillomavirus testing in head and neck squamous cell carcinoma in 2020: where are we now and where are we going? Head Neck Pathol. 2020. https://doi.org/10.1007/s12105-019-01117-y.
Lewis JS Jr. Morphologic diversity in human papillomavirus-related oropharyngeal squamous cell carcinoma: Catch Me If You Can! Mod Pathol. 2017;30(s1):S44–s53. https://doi.org/10.1038/modpathol.2016.152.
Serra S, Chetty R. p16. J Clin Pathol. 2018;71(10):853–8. https://doi.org/10.1136/jclinpath-2018-205216.
Liggett WH Jr, Sidransky D. Role of the p16 tumor suppressor gene in cancer. J Clin Oncol. 1998;16(3):1197–206. https://doi.org/10.1200/jco.1998.16.3.1197.
Estevao D, Costa NR, Gil da Costa RM, Medeiros R. Hallmarks of HPV carcinogenesis: the role of E6, E7 and E5 oncoproteins in cellular malignancy. Biochim Biophys Acta Gene Regul Mech. 2019;1862(2):153–62. https://doi.org/10.1016/j.bbagrm.2019.01.001.
Sedghizadeh PP, Billington WD, Paxton D, Ebeed R, Mahabady S, Clark GT, et al. Is p16-positive oropharyngeal squamous cell carcinoma associated with favorable prognosis? A systematic review and meta-analysis. Oral Oncol. 2016;54:15–27. https://doi.org/10.1016/j.oraloncology.2016.01.002.
Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tan PF, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363(1):24–35. https://doi.org/10.1056/NEJMoa0912217.
Seiwert TY, Foster CC, Blair EA, Karrison TG, Agrawal N, Melotek JM, et al. OPTIMA: a phase II dose and volume de-escalation trial for human papillomavirus-positive oropharyngeal cancer. Ann Oncol. 2019;30(2):297–302. https://doi.org/10.1093/annonc/mdy522.
Li JG, Li L, Zhang SW. Different expression of p16INK4a and p14ARF in cervical and lung cancers. Eur Rev Med Pharmacol Sci. 2013;17(22):3007–111.
Cheng YL, Lee SC, Harn HJ, Chen CJ, Chang YC, Chen JC, et al. Prognostic prediction of the immunohistochemical expression of p53 and p16 in resected non-small cell lung cancer. Eur J Cardio-Thoracic Surg. 2003;23(2):221–8. https://doi.org/10.1016/s1010-7940(02)00749-2.
Huang CI, Taki T, Higashiyama M, Kohno N, Miyake M. p16 protein expression is associated with a poor prognosis in squamous cell carcinoma of the lung. Br J Cancer. 2000;82(2):374–80. https://doi.org/10.1054/bjoc.1999.0929.
Zhou Y, Hoti N, Ao M, Zhang Z, Zhu H, Li L, et al. Expression of p16 and p53 in non-small-cell lung cancer: clinicopathological correlation and potential prognostic impact. Biomarkers Med. 2019;13(9):761–71. https://doi.org/10.2217/bmm-2018-0441.
Sterlacci W, Tzankov A, Veits L, Zelger B, Bihl MP, Foerster A, et al. A comprehensive analysis of p16 expression, gene status, and promoter hypermethylation in surgically resected non-small cell lung carcinomas. J Thoracic Oncol. 2011;6(10):1649–57. https://doi.org/10.1097/JTO.0b013e3182295745.
Jin M, Inoue S, Umemura T, Moriya J, Arakawa M, Nagashima K, et al. Cyclin D1, p16 and retinoblastoma gene product expression as a predictor for prognosis in non-small cell lung cancer at stages I and II. Lung Cancer (Amsterdam, Netherlands). 2001;34(2):207–18. https://doi.org/10.1016/s0169-5002(01)00225-2.
Gatta LB, Balzarini P, Tironi A, Berenzi A, Benetti A, Angiero F, et al. Human papillomavirus DNA and p16 gene in squamous cell lung carcinoma. Anticancer Res. 2012;32(8):3085–9.
Plaza JA, Ramirez NC, Nuovo GJ. Utility of HPV analysis for evaluation of possible metastatic disease in women with cervical cancer. Int J Gynecol Pathol. 2004;23(1):7–12. https://doi.org/10.1097/01.pgp.0000101084.35393.03.
Bishop JA, Ogawa T, Chang X, Illei PB, Gabrielson E, Pai SI, et al. HPV analysis in distinguishing second primary tumors from lung metastases in patients with head and neck squamous cell carcinoma. Am J Surg Pathol. 2012;36(1):142–8. https://doi.org/10.1097/PAS.0b013e3182395c7b.
Srinivasan M, Taioli E, Ragin CC. Human papillomavirus type 16 and 18 in primary lung cancers—a meta-analysis. Carcinogenesis. 2009;30(10):1722–8. https://doi.org/10.1093/carcin/bgp177.
Zhai K, Ding J, Shi HZ. HPV and lung cancer risk: a meta-analysis. J Clin Virol. 2015;63:84–90. https://doi.org/10.1016/j.jcv.2014.09.014.
Xiong WM, Xu QP, Li X, Xiao RD, Cai L, He F. The association between human papillomavirus infection and lung cancer: a system review and meta-analysis. Oncotarget. 2017;8(56):96419–32. https://doi.org/10.18632/oncotarget.21682.
Tsyganov MM, Pevzner AM, Ibragimova MK, Deryusheva IV, Litviakov NV. Human papillomavirus and lung cancer: an overview and a meta-analysis. J Cancer Res Clin Oncol. 2019;145(8):1919–37. https://doi.org/10.1007/s00432-019-02960-w.
Acknowledgments
The authors thank the Human Tissue Resource Center at the University of Chicago for performing all immunohistochemical and in situ hybridization studies.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schulte, J.J., Steinmetz, J., Furtado, L.V. et al. Metastatic HPV-Associated Oropharyngeal Versus Primary Pulmonary Squamous Cell Carcinoma: is p16 Immunostain Useful?. Head and Neck Pathol 14, 966–973 (2020). https://doi.org/10.1007/s12105-020-01165-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-020-01165-9