Abstract
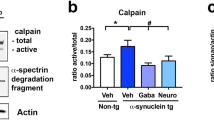
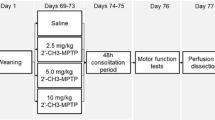
Parkinson’s disease (PD) is the most common neurodegenerative movement disorder, resulting in dopaminergic (DA) neuronal loss in the substantia nigra pars compacta (SNpc) and damage to the extranigral spinal cord neurons. Current therapies do not prevent the disease progression. Hence, developing efficacious therapeutic strategies for treatment of PD is of utmost importance. The goal of this study is to delineate the involvement of calpain-mediated inflammation and neurodegeneration in SN and spinal cord in MPTP-induced parkinsonian mice (C57BL/6 N), thereby elucidating potential therapeutic target(s). Increased calpain expression was found localized to tyrosine hydroxylase (TH+) neurons in SN with significantly increased TUNEL-positive neurons in SN and spinal cord neurons in MPTP mice. Inflammatory markers Cox-2, caspase-1, and NOS-2 were significantly upregulated in MPTP mouse spinal cord as compared to control. These parameters correlated with the activation of astrocytes, microglia, infiltration of CD4+/CD8+ T cells, and macrophages. We found that subpopulations of CD4+ cells (Th1 and Tregs) were differentially expanded in MPTP mice, which could be regulated by inhibition of calpain with the potent inhibitor calpeptin. Pretreatment with calpeptin (25 μg/kg, i.p.) attenuated glial activation, T cell infiltration, nigral dopaminergic degeneration in SN, and neuronal death in spinal cord. Importantly, calpeptin ameliorated MPTP-induced altered gait parameters (e.g., reduced stride length and increased stride frequency) as demonstrated by analyses of spatiotemporal gait indices using ventral plane videography. These findings suggest that calpain plays a pivotal role in MPTP-induced nigral and extranigral neurodegenerative processes and may be a valid therapeutic target in PD.






Similar content being viewed by others
Abbreviations
- DA:
-
Dopaminergic
- deNFP:
-
Dephosphorylated neurofilament protein
- GFAP:
-
Glial fibrillary acidic protein
- IR:
-
Immunoreactivity
- L-DOPA:
-
L-3,4-dihydroxyphenylalanine
- MPTP:
-
1-Methyl-4-phenyl-1,2,3,6-tetrahydropyridine
- PD:
-
Parkinson disease
- SN:
-
Substantia nigra
- TH:
-
Tyrosine hydroxylase
- SBDP:
-
Spectrin break down product
References
Olanow CW, Stocchi F, Lang AE (2011) Parkinson’s disease: non-motor and non-dopaminergic features. Wiley, Chichester
Weintraub D, Dietz N, Duda JE, Wolk DA, Doshi J, Xie SX, Davatzikos C, Clark CM et al (2012) Alzheimer’s disease pattern of brain atrophy predicts cognitive decline in Parkinson’s disease. Brain 135(Pt 1):170–180. doi:10.1093/brain/awr277
Palavra NC, Naismith SL, Lewis SJ (2013) Mild cognitive impairment in Parkinson’s disease: a review of current concepts. Neurol Res Int 2013:576091. doi:10.1155/2013/576091
Bocanegra Y, Trujillo-Orrego N, Pineda D (2014) Dementia and mild cognitive impairment in Parkinson’s disease: a review. Rev Neurol 59(12):555–569
Knaryan VH, Samantaray S, Le Gal C, Ray SK, Banik NL (2011) Tracking extranigral degeneration in animal models of Parkinson’s disease: quest for effective therapeutic strategies. J Neurochem 118(3):326–338. doi:10.1111/j.1471-4159.2011.07320.x
Sanchez-Lopez F, Tasset I, Aguera E, Feijoo M, Fernandez-Bolanos R, Sanchez FM, Ruiz MC, Cruz AH et al (2012) Oxidative stress and inflammation biomarkers in the blood of patients with Huntington’s disease. Neurol Res 34(7):721–724. doi:10.1179/1743132812Y.0000000073
McGeer PL, McGeer EG (2008) Glial reactions in Parkinson’s disease. Mov Disord 23(4):474–483. doi:10.1002/mds.21751
Kamer AR, Dasanayake AP, Craig RG, Glodzik-Sobanska L, Bry M, de Leon MJ (2008) Alzheimer’s disease and peripheral infections: the possible contribution from periodontal infections, model and hypothesis. J Alzheimers Dis 13(4):437–449
McGeer PL, Itagaki S, Boyes BE, McGeer EG (1988) Reactive microglia are positive for HLA-DR in the substantia nigra of Parkinson’s and Alzheimer’s disease brains. Neurology 38(8):1285–1291
Amor S, Woodroofe MN (2014) Innate and adaptive immune responses in neurodegeneration and repair. Immunology 141(3):287–291. doi:10.1111/imm.12134
Samantaray S, Knaryan VH, Shields DC, Banik NL (2013) Critical role of calpain in spinal cord degeneration in Parkinson’s disease. J Neurochem 127(6):880–890. doi:10.1111/jnc.12374
Smith JA, Das A, Ray SK, Banik NL (2012) Role of pro-inflammatory cytokines released from microglia in neurodegenerative diseases. Brain Res Bull 87(1):10–20. doi:10.1016/j.brainresbull.2011.10.004
Levesque S, Wilson B, Gregoria V, Thorpe LB, Dallas S, Polikov VS, Hong JS, Block ML (2010) Reactive microgliosis: extracellular micro-calpain and microglia-mediated dopaminergic neurotoxicity. Brain 133(Pt 3):808–821. doi:10.1093/brain/awp333
Block ML, Zecca L, Hong JS (2007) Microglia-mediated neurotoxicity: uncovering the molecular mechanisms. Nat Rev Neurosci 8(1):57–69. doi:10.1038/nrn2038
Brochard V, Combadiere B, Prigent A, Laouar Y, Perrin A, Beray-Berthat V, Bonduelle O, Alvarez-Fischer D et al (2009) Infiltration of CD4+ lymphocytes into the brain contributes to neurodegeneration in a mouse model of Parkinson disease. J Clin Invest 119(1):182–192. doi:10.1172/JCI36470
Subramaniam SR, Chesselet MF (2013) Mitochondrial dysfunction and oxidative stress in Parkinson’s disease. Prog Neurobiol 106–107:17–32. doi:10.1016/j.pneurobio.2013.04.004
Jellinger KA (2014) The pathomechanisms underlying Parkinson’s disease. Expert Rev Neurother 14(2):199–215. doi:10.1586/14737175.2014.877842
Samantaray S, Ray SK, Banik NL (2008) Calpain as a potential therapeutic target in Parkinson’s disease. CNS Neurol Disord Drug Targets 7:305–312
Shields DC, Schaecher KE, Saido TC, Banik NL (1999) A putative mechanism of demyelination in multiple sclerosis by a proteolytic enzyme, calpain. Proc Natl Acad Sci U S A 96(20):11486–11491
Trager N, Smith A, Wallace Iv G, Azuma M, Inoue J, Beeson C, Haque A, Banik NL (2014) Effects of a novel orally administered calpain inhibitor SNJ-1945 on immunomodulation and neurodegeneration in a murine model of multiple sclerosis. J Neurochem 130(2):268–279. doi:10.1111/jnc.12659
Knaryan VH, Samantaray S, Park S, Azuma M, Inoue J, Banik NL SNJ-1945, a calpain inhibitor, protects SH-SY5Y cells against MPP(+) and rotenone. J Neurochem 130 (2):280–290. doi:10.1111/jnc.12629
Crocker SJ, Smith PD, Jackson-Lewis V, Lamba WR, Hayley SP, Grimm E, Callaghan SM, Slack RS et al (2003) Inhibition of calpains prevents neuronal and behavioral deficits in an MPTP mouse model of Parkinson’s disease. J Neurosci 23(10):4081–4091
Mouatt-Prigent A, Karlsson JO, Agid Y, Hirsch EC (1996) Increased M-calpain expression in the mesencephalon of patients with Parkinson’s disease but not in other neurodegenerative disorders involving the mesencephalon: a role in nerve cell death? Neuroscience 73(4):979–987
Samantaray S, Knaryan VH, Le Gal C, Ray SK, Banik NL (2011) Calpain inhibition protected spinal cord motoneurons against 1-methyl-4-phenylpyridinium ion and rotenone. Neuroscience 192:263–274. doi:10.1016/j.neuroscience.2011.06.007
Samantaray S, Ray SK, Ali SF, Banik NL (2006) Calpain activation in apoptosis of motoneurons in cell culture models of experimental parkinsonism. Ann N Y Acad Sci 1074:349–356. doi:10.1196/annals.1369.034
Games D, Valera E, Spencer B, Rockenstein E, Mante M, Adame A, Patrick C, Ubhi K et al (2014) Reducing C-terminal-truncated alpha-synuclein by immunotherapy attenuates neurodegeneration and propagation in Parkinson’s disease-like models. J Neurosci 34(28):9441–9454. doi:10.1523/JNEUROSCI.5314-13.2014
Dufty BM, Warner LR, Hou ST, Jiang SX, Gomez-Isla T, Leenhouts KM, Oxford JT, Feany MB et al (2007) Calpain-cleavage of alpha-synuclein: connecting proteolytic processing to disease-linked aggregation. Am J Pathol 170(5):1725–1738. doi:10.2353/ajpath.2007.061232
Mishizen-Eberz AJ, Norris EH, Giasson BI, Hodara R, Ischiropoulos H, Lee VM, Trojanowski JQ, Lynch DR (2005) Cleavage of alpha-synuclein by calpain: potential role in degradation of fibrillized and nitrated species of alpha-synuclein. Biochemistry 44(21):7818–7829. doi:10.1021/bi047846q
Jin J, Shie FS, Liu J, Wang Y, Davis J, Schantz AM, Montine KS, Montine TJ et al (2007) Prostaglandin E2 receptor subtype 2 (EP2) regulates microglial activation and associated neurotoxicity induced by aggregated alpha-synuclein. J Neuroinflammation 4:2. doi:10.1186/1742-2094-4-2
Lee HJ, Patel S, Lee SJ (2005) Intravesicular localization and exocytosis of alpha-synuclein and its aggregates. J Neurosci 25(25):6016–6024. doi:10.1523/JNEUROSCI.0692-05.2005
Sulzer D (2007) Multiple hit hypotheses for dopamine neuron loss in Parkinson’s disease. Trends Neurosci 30(5):244–250. doi:10.1016/j.tins.2007.03.009
Samantaray S, Knaryan VH, Butler JT, Ray SK, Banik NL (2008) Spinal cord degeneration in C57BL/6N mice following induction of experimental parkinsonism with MPTP. J Neurochem 104(5):1309–1320. doi:10.1111/j.1471-4159.2007.05091.x
Vivacqua G, Biagioni F, Yu S, Casini A, Bucci D, D’Este L, Fornai F (2012) Loss of spinal motor neurons and alteration of alpha-synuclein immunostaining in MPTP induced Parkinsonism in mice. J Chem Neuroanat 44:76–85. doi:10.1016/j.jchemneu.2012.04.003
Litteljohn D, Mangano E, Clarke M, Bobyn J, Moloney K, Hayley S (2011) Inflammatory mechanisms of neurodegeneration in toxin-based models of Parkinson’s disease. Parkinsons Dis 713517. doi:10.4061/2011/713517
Reynolds AD, Stone DK, Hutter JA, Benner EJ, Mosley RL, Gendelman HE (2010) Regulatory T cells attenuate Th17 cell-mediated nigrostriatal dopaminergic neurodegeneration in a model of Parkinson’s disease. J Immunol 184(5):2261–2271. doi:10.4049/jimmunol.0901852
Ray SK, Banik NL (2003) Calpain and its involvement in the pathophysiology of CNS injuries and diseases: therapeutic potential of calpain inhibitors for prevention of neurodegeneration. Curr Drug Targets CNS Neurol Disord 2(3):173–189
Chera B, Schaecher KE, Rocchini A, Imam SZ, Sribnick EA, Ray SK, Ali SF, Banik NL (2004) Immunofluorescent labeling of increased calpain expression and neuronal death in the spinal cord of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-treated mice. Brain Res 1006(2):150–156. doi:10.1016/j.brainres.2004.01.065
Del Tredici K, Braak H (2012) Spinal cord lesions in sporadic Parkinson’s disease. Acta Neuropathol 124(5):643–664. doi:10.1007/s00401-012-1028-y
Reynolds AD, Stone DK, Mosley RL, Gendelman HE (2009) Nitrated {alpha}-synuclein-induced alterations in microglial immunity are regulated by CD4+ T cell subsets. J Immunol 182(7):4137–4149. doi:10.4049/jimmunol.0803982
Couch Y, Alvarez-Erviti L, Sibson NR, Wood MJ, Anthony DC (2011) The acute inflammatory response to intranigral alpha-synuclein differs significantly from intranigral lipopolysaccharide and is exacerbated by peripheral inflammation. J Neuroinflammation 8:166. doi:10.1186/1742-2094-8-166
Hurley MJ, Brandon B, Gentleman SM, Dexter DT (2013) Parkinson’s disease is associated with altered expression of CaV1 channels and calcium-binding proteins. Brain J Neurol 136(Pt 7):2077–2097. doi:10.1093/brain/awt134
Liang CL, Sinton CM, Sonsalla PK, German DC (1996) Midbrain dopaminergic neurons in the mouse that contain calbindin-D28k exhibit reduced vulnerability to MPTP-induced neurodegeneration. Neurodegeneration 5(4):313–318
McMahon A, Wong BS, Iacopino AM, Ng MC, Chi S, German DC (1998) Calbindin-D28k buffers intracellular calcium and promotes resistance to degeneration in PC12 cells. Brain Res Mol Brain Res 54(1):56–63
Mouatt-Prigent A, Agid Y, Hirsch EC (1994) Does the calcium binding protein calretinin protect dopaminergic neurons against degeneration in Parkinson’s disease? Brain Res 668(1–2):62–70
Butler JT, Samantaray S, Beeson CC, Ray SK, Banik NL (2009) Involvement of calpain in the process of Jurkat T cell chemotaxis. J Neurosci Res 87(3):626–635. doi:10.1002/jnr.21882
Smith AW, Doonan BP, Tyor WR, Abou-Fayssal N, Haque A, Banik NL (2011) Regulation of Th1/Th17 cytokines and IDO gene expression by inhibition of calpain in PBMCs from MS patients. J Neuroimmunol 232(1–2):179–185. doi:10.1016/j.jneuroim.2010.09.030
Schaecher K, Rocchini A, Dinkins J, Matzelle DD, Banik NL (2002) Calpain expression and infiltration of activated T cells in experimental allergic encephalomyelitis over time: increased calpain activity begins with onset of disease. J Neuroimmunol 129(1–2):1–9
Hickey WF, Gonatas NK, Kimura H, Wilson DB (1983) Identification and quantitation of T lymphocyte subsets found in the spinal cord of the Lewis rat during acute experimental allergic encephalomyelitis. J Immunol 131(6):2805–2809
Nayak D, Roth TL, McGavern DB (2014) Microglia development and function. Annu Rev Immunol 32:367–402. doi:10.1146/annurev-immunol-032713-120240
Cabezas R, Avila M, Gonzalez J, El-Bacha RS, Baez E, Garcia-Segura LM, Jurado Coronel JC, Capani F et al (2014) Astrocytic modulation of blood brain barrier: perspectives on Parkinson’s disease. Front Cell Neurosci 8:211. doi:10.3389/fncel.2014.00211
McDowell ML, Das A, Smith JA, Varma AK, Ray SK, Banik NL (2011) Neuroprotective effects of genistein in VSC4.1 motoneurons exposed to activated microglial cytokines. Neurochem Int 59(2):175–184. doi:10.1016/j.neuint.2011.04.011
Tichauer J, Saud K, von Bernhardi R (2007) Modulation by astrocytes of microglial cell-mediated neuroinflammation: effect on the activation of microglial signaling pathways. Neuroimmunomodulation 14(3–4):168–174. doi:10.1159/000110642
Weiss JM, Downie SA, Lyman WD, Berman JW (1998) Astrocyte-derived monocyte-chemoattractant protein-1 directs the transmigration of leukocytes across a model of the human blood–brain barrier. J Immunol 161(12):6896–6903
Laflamme N, Lacroix S, Rivest S (1999) An essential role of interleukin-1beta in mediating NF-kappaB activity and COX-2 transcription in cells of the blood–brain barrier in response to a systemic and localized inflammation but not during endotoxemia. J Neurosci Off J Socie Neurosci 19(24):10923–10930
Su X, Federoff HJ (2014) Immune responses in Parkinson’s disease: interplay between central and peripheral immune systems. BioMed Res Int 2014:275178. doi:10.1155/2014/275178
Desai BS, Monahan AJ, Carvey PM, Hendey B (2007) Blood–brain barrier pathology in Alzheimer’s and Parkinson’s disease: implications for drug therapy. Cell Transplant 16(3):285–299
Stone DK, Reynolds AD, Mosley RL, Gendelman HE (2009) Innate and adaptive immunity for the pathobiology of Parkinson’s disease. Antioxid Redox Signal 11(9):2151–2166. doi:10.1089/ARS.2009.2460
Kortekaas R, Leenders KL, van Oostrom JC, Vaalburg W, Bart J, Willemsen AT, Hendrikse NH (2005) Blood–brain barrier dysfunction in parkinsonian midbrain in vivo. Ann Neurol 57(2):176–179. doi:10.1002/ana.20369
Gonzalez H, Contreras F, Prado C, Elgueta D, Franz D, Bernales S, Pacheco R (2013) Dopamine receptor D3 expressed on CD4+ T cells favors neurodegeneration of dopaminergic neurons during Parkinson’s disease. J Immunol 190(10):5048–5056. doi:10.4049/jimmunol.1203121
Blin O, Ferrandez AM, Serratrice G (1990) Quantitative analysis of gait in Parkinson patients: increased variability of stride length. J Neurol Sci 98(1):91–97
Hausdorff JM, Cudkowicz ME, Firtion R, Wei JY, Goldberger AL (1998) Gait variability and basal ganglia disorders: stride-to-stride variations of gait cycle timing in Parkinson’s disease and Huntington’s disease. Mov Disord 13(3):428–437. doi:10.1002/mds.870130310
Morris ME, Huxham F, McGinley J, Dodd K, Iansek R (2001) The biomechanics and motor control of gait in Parkinson disease. Clin Biomech (Bristol, Avon) 16(6):459–470
Morris ME, Matyas TA, Iansek R, Summers JJ (1996) Temporal stability of gait in Parkinson’s disease. Phys Ther 76(7):763–777, discussion 778–780
Plotnik M, Hausdorff JM (2008) The role of gait rhythmicity and bilateral coordination of stepping in the pathophysiology of freezing of gait in Parkinson’s disease. Mov Disord 23(Suppl 2):S444–450. doi:10.1002/mds.21984
Schaafsma JD, Giladi N, Balash Y, Bartels AL, Gurevich T, Hausdorff JM (2003) Gait dynamics in Parkinson’s disease: relationship to Parkinsonian features, falls and response to levodopa. J Neurol Sci 212(1–2):47–53
Wu Y, Krishnan S (2010) Statistical analysis of gait rhythm in patients with Parkinson’s disease. IEEE Trans Neural Syst Rehabil Eng 18(2):150–158. doi:10.1109/TNSRE.2009.2033062
Karachi C, Grabli D, Bernard FA, Tande D, Wattiez N, Belaid H, Bardinet E, Prigent A et al (2010) Cholinergic mesencephalic neurons are involved in gait and postural disorders in Parkinson disease. J Clin Invest 120(8):2745–2754
Amende I, Kale A, McCue S, Glazier S, Morgan JP, Hampton TG (2005) Gait dynamics in mouse models of Parkinson’s disease and Huntington’s disease. J Neuroeng Rehabil 2:20. doi:10.1186/1743-0003-2-20
Goldberg NR, Hampton T, McCue S, Kale A, Meshul CK (2011) Profiling changes in gait dynamics resulting from progressive 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-induced nigrostriatal lesioning. J Neurosci Res 89(10):1698–1706. doi:10.1002/jnr.22699
Jackson-Lewis V, Przedborski S (2007) Protocol for the MPTP mouse model of Parkinson’s disease. Nat Protoc 2(1):141–151. doi:10.1038/nprot.2006.342
Jakowec MW, Petzinger GM (2004) 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-lesioned model of parkinson’s disease, with emphasis on mice and nonhuman primates. Comp Med 54(5):497–513
Przedborski S, Jackson-Lewis V, Naini AB, Jakowec M, Petzinger G, Miller R, Akram M (2001) The parkinsonian toxin 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP): a technical review of its utility and safety. J Neurochem 76(5):1265–1274
Tatton NA, Kish SJ (1997) In situ detection of apoptotic nuclei in the substantia nigra compacta of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-treated mice using terminal deoxynucleotidyl transferase labelling and acridine orange staining. Neuroscience 77(4):1037–1048
Banik NL, Hogan EL, Jenkins MG, McDonald JK, McAlhaney WW, Sostek MB (1983) Purification of a calcium-activated neutral proteinase from bovine brain. Neurochem Res 8(11):1389–1405
Samantaray S, Knaryan VH, Guyton MK, Matzelle DD, Ray SK, Banik NL (2007) The parkinsonian neurotoxin rotenone activates calpain and caspase-3 leading to motoneuron degeneration in spinal cord of Lewis rats. Neuroscience 146(2):741–755. doi:10.1016/j.neuroscience.2007.01.056
God JM, Zhao D, Cameron CA, Amria S, Bethard JR, Haque A (2014) Disruption of HLA class II antigen presentation in Burkitt lymphoma: implication of a 47,000 MW acid labile protein in CD4+ T-cell recognition. Immunology 142(3):492–505. doi:10.1111/imm.12281
Kale A, Amende I, Meyer GP, Crabbe JC, Hampton TG (2004) Ethanol’s effects on gait dynamics in mice investigated by ventral plane videography. Alcohol Clin Exp Res 28(12):1839–1848
Acknowledgments
Authors thank Dr. Ajit Kale of Mouse Specifics for helpful suggestions during analysis of gait parameters. This study was funded in part by the RO1 grants from National Institute of Neurological Disorders and Stroke of the National Institutes of Health (NINDS-NIH; NS-62327-01A2; NS-56176 and NS-65456) and the Veterans Administration (I01 BX001262 and I01 BX002349).
Conflict of Interest
Authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Samantaray, S., Knaryan, V.H., Shields, D.C. et al. Inhibition of Calpain Activation Protects MPTP-Induced Nigral and Spinal Cord Neurodegeneration, Reduces Inflammation, and Improves Gait Dynamics in Mice. Mol Neurobiol 52, 1054–1066 (2015). https://doi.org/10.1007/s12035-015-9255-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-015-9255-6