Abstract
Infections are widely believed to serve as a trigger for initiating autoimmune disease in humans. An infectious agent may activate lymphocytes in an antigen-specific manner and can also provide the nonantigen-specific second signal necessary to induce a pathogenic adaptive immune response. Collectively, the secondary signaling necessary for induction of an autoimmune disease has been referred to as the adjuvant effect. Examples of an adjuvant effect have been described in the induction of experimental thyroiditis where the administration with thyroglobulin of muramyl dipeptide of mycobacteria or lipopolysaccaride of Gram-negative bacilli provide the necessary adjuvant effect. Other commonly used adjuvants fail to induce disease, although they may elicit autoantibody formation. Myocarditis can be induced in susceptible mice by infection with cardiotrophic coxsackievirus B3 and even induced in resistant mice if an additional adjuvant effect is provided through proinflammatory cytokines like interleukin-1β and tumor necrosis factor-α. The adjuvant effect is usually exerted early after infection during the innate immune response, operating at least in part through toll-like receptors and mast cells to direct the subsequent pathogenic adaptive immune response.
Similar content being viewed by others
Autoimmune diseases in humans arise from the chance accumulation of a group of genes in the host that together heighten susceptibility to autoimmune responses [1]. The most prominent genes are members of the major histocompatibility complex (MHC), but a number of additional genes normally involved in regulation of the immune response have now been identified as contributing to the so-called autoimmune diathesis, that is, a genetic predisposition to develop autoimmune disease. In addition, stochastic variation is introduced by the specialized mechanisms that determine the broad diversity of immune system recognition, such as V(D)J recombination, receptor editing, and somatic mutation. Thus, the immune system has the potential to recognize the universe of pathogens, present or future. At the same time, antigens of the host will also be recognized. If appropriately stimulated, self-reactive lymphocytes can produce clones of lymphocytes capable of generating autoantibodies. Multiple control systems usually operate to limit and regulate such clones, but when regulation fails, autoimmune disease (or malignant disease) may result.
In addition to the genetic predisposition, it seems that an environmental factor is required to trigger the onset of the autoimmune process in humans. Among the many environmental triggers that have been implicated in the initiation of autoimmune disease, infection has remained the most prominent (Fig. 1). Infectious agents such as viruses can provide the autoantigen-specific stimulus required for activation of the T cell receptor (TCR) or B cell receptor. A number of mechanisms have been described to account for autoantigen-specific responses during or after infection including molecular mimicry, T cell degeneracy, epitope spreading, spillage of normally inaccessible antigens, and alteration of autologous antigens. Some experimental evidence for each of these potential mechanisms has been described [2]. Less attention has been directed to the requirement for additional nonantigen-specific stimuli to initiate the autoimmune response. It has long been realized that proliferation of T cells requires costimulation by a second signal in addition to engagement of the TCR. In naïve T cells, TCR engagement alone is usually ineffective in activating the pathways that are needed to induce production of proinflammatory cytokines and other growth factors. Insufficient input by secondary signals renders the cell refractory to TCR-stimulated growth, a phenomena referred to as anergy [3]. When TCR engagement alone initiates proliferation, it eventually results in T cell apoptosis because of insufficient induction of antiapoptotic factors [4]. These mechanisms prevent the unremitting proliferation of peripheral T cells that recognize self-antigens through their TCR alone. The second signal determines whether an encounter with a potential self-antigen is aborted at an early stage or proceeds to a pathogenic autoimmune outcome. Similar mechanisms prevail in the B cell. Collectively, the second signals necessary for induction of autoimmune disease have been referred to as bystander activation or the adjuvant effect. Information has accumulated rapidly in recent years that allows us to analyze the adjuvant effect at a molecular level.
Adjuvants do not have to arise from an external source. In fact, many studies have recently shown that endogenous adjuvants, especially in the form of small ribonucleoproteins, stress proteins, or products of damaged cells, can promote autoimmune responses [5–7]. Often, however, the responses are transient and do not progress to clinical disease.
Multiple sclerosis is an autoimmune disease that is associated with environmental exposure during early childhood. Several different viruses have been implicated. Some may act by molecular mimicry, whereas others provide the adjuvant effect. However, adjuvants can enhance or reduce immune responses. For example, in a model of multiple sclerosis induced by vaccinia virus expressing myelin protein, infection with the lymphocytic choriomeningitis virus can induce type 1 interferons (IFN) and reduce diseases, whereas the murine cytomegalovirus can activate antigen-presenting cells, increasing interleukin (IL)-12 and type II IFN and enhancing disease [8]. Instead of cytomegalovirus, complete Freund adjuvant can activate the immune system to induce disease.
Other autoimmune diseases can behave quite differently. For example, patients receiving type I IFN for treatment of malignancy show a significant increase in autoimmune thyroid disease [9]. In contrast, treatment of NOD mice with complete Freund adjuvant prevents the development of insulitis and autoimmune diabetes [10].
We first became aware of the importance of adjuvant in the induction of autoimmune disease during our early studies on the initiation of experimental autoimmune thyroiditis by immunization with thyroglobulin [11] (Table 1). We found that injection of purified thyroglobulin plus complete Freund adjuvant induced production of both thyroglobulin-specific autoantibodies and inflammatory lesions in the thyroid gland. In contrast, injection of thyroglobulin with incomplete Freund adjuvant, lacking the mycobacterial component, gave rise to autoantibody production but no lesions in the thyroid gland itself. We were able to follow up these observations in collaboration with Kong et al. [12] (Table 2). We found first that the injection of thyroglobulin with incomplete Freund adjuvant plus muramyl dipeptide, a component of a mycobacterial cell wall, induced characteristic lesions of thyroiditis. Similarly, injection of thyroglobulin and concurrent intravenous administration of bacterial lipopolysaccharide (LPS) induced the full picture of autoimmune disease with the production of both autoantibodies and lesions in the thyroid. On the other hand, most of the other adjuvants we tested at the time, including poly(A–U), alum, bentonite, silica, and silicone oil, induced only autoantibody production but not thyroid lesions. These findings closely associated the adjuvant effect with concurrent administration of products of infection.
Several years later, we investigated the adjuvant effect from viral infection [13]. We found that in genetically susceptible strains of mice, we could induce autoimmune myocarditis by infecting the mice with a cardiotropic strain of coxsackievirus B3 (CB3). The autoimmune disease was characterized by production of autoantibody specific for the cardiac isoform of myosin. Subsequently, we were able to induce the same autoimmune disease by direct immunization of the susceptible mice with cardiac myosin or myosin-derived peptides in the absence of the virus (Fig. 2). For the production of myocardial lesions, all of these injections of cardiac myosin or myosin peptide, however, required coadministration of complete Freund adjuvant. Sometimes, we even included pertussis toxin as a second adjuvant to increase the severity of the disease. Because we were curious about the mechanisms by which infection alters the immune process, we tested the effect of CB3 infection in mice that were genetically resistant to the induction of autoimmune myocarditis. Under usual conditions, infection of some strains of mice, such as B10.A, with CB3 induced an acute limited viral myocarditis that was not followed by the autoimmune disease. If, however, we coadministered LPS with the virus, autoimmune myocarditis developed after the viral myocarditis subsided [14] (Table 3). Because we assumed that the role of LPS as a coadjuvant was to initiate a cascade of proinflammatory cytokines, we tested the coadministration of recombinant IL-1β and found that CB3 infection plus IL-1β also led to autoimmune myocarditis even in genetically resistant strains of mice [15].
The same experiments were performed using cardiac myosin as an antigen. Immunization of B10.A in mice with cardiac myosin even with complete Freund adjuvant lead to no or only mild lesions. If, however, we included LPS with the immunization regime, then severe myocarditis was found in most of the mice [16], showing that with resistant animals, we require an even more potent adjuvant effect.
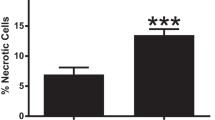
These experiments focused our attention on the very early response to the adjuvant, the response associated with natural innate immunity. With Fairweather [17], we found that the difference between strains of mice destined to develop autoimmune myocarditis and those resistant to it was apparent as early as 6 h after viral infection, taking the form of significant differences in the production of IL-1β (Table 4). To account for such a prompt early distinction between responder and nonresponder animals, we tested a number of potential antigen-presenting cells and found that there was a marked difference in the numbers of mast cells in the spleens of responder vs nonresponder mouse strains. The finding encouraged us to scrutinize the mast cell as a potential antigen-presenting cell in the initiation of the autoimmune form of myocarditis that may follow previous viral infection. We found, in fact, that mast cells not only upregulated MHC class II, a sign of activation but also the costimulatory molecules B7-1/2 and toll-like receptor 4 (TLR4) (Table 5). The experiments have led us to propose that the mast cell is a key early player in the generation of the adjuvant effect required for the initiation of an autoimmune disease after viral infection.
A final series of experiments was carried out using a surrogate marker of the adjuvant effect, where a sudden drop in the thyroid hormone, thyroxine, after immunization using complete Freund adjuvant occurred [18]. Referring back to our earlier experiments, we found that this drop in thyroxine occurred when mice were immunized with thyroglobulin and complete Freund adjuvant or thyroglobulin and LPS but not when animals were injected with thyroglobulin and incomplete Freund adjuvant or thyroglobulin alone. Looking further for a mechanism, we found that the adjuvant effect of LPS was demonstrable in wild-type mice but not in animals deficient in MyD88. This adaptor molecule is a cofactor in activating several members of the TLR family including TLR4 and TLR2. These experiments allow us to assign an obligatory role to the TLRs in the adjuvant effect of LPS. MyD88 is also essential for the induction of experimental autoimmune myocarditis by immunization with cardiac myosin and complete Freund adjuvant [19].
These experiments suggest that infection plays a major role in triggering autoimmunity. Accumulating data have shown that microbial products modulate the immune response by interacting with TLRs expressed on antigen-presenting cells. The resulting profile of cytokines, Th1, Th2, or Th17, in turn determines the pathogenicity of the autoimmune response. Returning to the mast cell, we then tested mice genetically deficient in mast cells and found that they also failed to develop the adjuvant effect when injected with complete Freud adjuvant or LPS.
In summary, we conclude that active infection or products of infection can provide the adjuvant effect necessary for the induction of many autoimmune disorders. The adjuvant effect depends upon giving early nonspecific signals to the initial innate immune response that later shape the adaptive immunity responsible for the pathogenic manifestations of autoimmunity.
References
Davidson S, Diamond B (2001) Autoimmune diseases. N Engl J Med 345:340–350
Rose NR, Griffin DE (1991) Virus-induced autoimmunity. In: Talal N (ed) Molecular autoimmunity. Academic, San Diego, CA, pp 247–272
Schwartz RN (2003) T cell anergy. Annu Rev Immunol 21:305–334
Hildeman DA, Zhu Y, Mitchell TC, Bouillet P, Strasser A, Kappler J, Marrach P (2002) Activated T cell death in vivo mediated by proapoptotic bcl-2 family member bim. Immunity 16:759–767
Rovere-Querini P, Manfredi AA, Sabbadini MG (2005) Environmental adjuvants, apoptosis and the censorship over autoimmunity. Autoimmun Rev 4:555–560
Rock KL, Hearn A, Chen CJ, Shi Y (2005) Natural endogenous adjuvants. Springer Semin Immunopathol 26:231–246
Kelly KM, Zhuang H, Nacionales DC, Scumpia PO, Lyons R, Akaogi J et al (2006) “Endogenous adjuvant” activity of the RNA components of lupus autoantigens Sm/RNP and Ro 60. Arthritis Rheum 54:1557–1567
McCoy L, Tsunoda I, Fujinami RS (2006) Multiple sclerosis and virus induced immune responses: autoimmunity can be primed by molecular mimicry and augmented by bystander activation. Autoimmunity 39:9–19
Satzger I, Meier A, Schenck F, Kapp A, Hauschild A, Gutzmer R (2007) Autoimmunity as a prognostic factor in melanoma patients treated with adjuvant low-dose interferon alpha. Int J Cancer 121:2562–2566
McInerney MF, Pek SB, Thomas DW (1991) Prevention of insulitis and diabetes onset by treatment with complete Freund’s adjuvant in NOD mice. Diabetes 40:715–725
Rose NR, Witebsky E (1959) Experimental immunological thyroiditis. In: Grabar P, Miescher P (eds) Proceedings of Immunopathology, 1st International Symposium, Basel/Seeligsberg, 1958. Benno Schwabe, Basel, pp 154–162
Kong YM, Audibert F, Giraldo AA, Rose NR, Chedid L (1985) Effects of natural or synthetic microbial adjuvants on induction of autoimmune thyroiditis. Infect Immun 49:40–45
Rose NR, Afanasyeva M (2003) From infection to autoimmunity: the adjuvant effect. ASM News 69:132–137
Lane JR, Neumann DA, Lafond-Walker A, Herskowitz A, Rose NR (1991) LPS promotes CB3-induced myocarditis in resistant B10.A mice. Cell Immunol 136:219–233
Lane JR, Neumann DA, Lafond-Walker A, Herskowitz A, Rose NR (1992) Interleukin 1 or tumor necrosis factor can promote Coxsackie B3-induced myocarditis in resistant B10.A mice. Exp Med 175:1123–1129
Neumann DA, Lane JR, Allen GS, Herskowitz A, Rose NR (1993) Viral myocarditis leading to cardiomyopathy: do cytokines contribute to pathogenesis? Clin Immunol Immunopathol 68:181–190
Fairweather D, Frisancho-Kiss S, Gatewood S, Njoku D, Steele R, Barrett M, Rose NR (2004) Mast cells and innate cytokines are associated with susceptibility to autoimmune heart disease following Coxsackievirus B3 infection. Autoimmunity 37:131–145
Rocchi R, Kimura H, Tzou SC, Suzuki K, Rose NR, Pinchera A et al (2007) Toll-like receptor-MyD88 and Fc receptor pathways of mast cells mediate the thyroid dysfunctions observed during nonthyroidal illness. Proc Natl Acad Sci USA 104:6019–6024
Marty RR, Dirnhofer S, Mauermann N, Schweikert S, Akira S, Hunziker L et al (2006) MyD88 signaling controls autoimmune myocarditis induction. Circulation 113:258–265
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rose, N.R. The Adjuvant Effect in Infection and Autoimmunity. Clinic Rev Allerg Immunol 34, 279–282 (2008). https://doi.org/10.1007/s12016-007-8049-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-007-8049-7