Abstract
Background
Acute myocardial infarction (MI) and the ensuing ischemic heart disease are approaching epidemic state. Unfortunately, no definitive therapies are available and human regenerative therapies have conflicting results. Limited stem cell retention following intracoronary administration has reduced the clinical efficacy of this novel therapy. Cathelicidin related antimicrobial peptides (CRAMPs) enhance chemotactic responsiveness of BMSPCs to low SDF-1 gradients, suggesting a potential role in BMSPCs engraftment. Here, we assessed the therapeutic efficacy of CRAMPs in the context of BMSPCs recruitment and retention via intracardiac delivery of CRAMP-treated BMSPCs or CRAMP-releasing hydrogels (HG) post-AMI.
Methods
For cell transplantation experiments, mice were randomized into 3 groups: MI followed by injection of PBS, BMMNCs alone, and BMMNCs pre-incubated with CRAMP. During the in vivo HG studies, BM GFP chimera mice were randomized into 4 groups: MI followed by injection of HG alone, HG + SDF-1, HG + CRAMP, HG + SDF-1 + CRAMP. Changes in cardiac function at 5 weeks after MI were assessed using echocardiography. Angiogenesis was assessed using isolectin staining for capillary density.
Results
Mice treated with BMMNCs pre-incubated with CRAMP had smaller scars, enhanced cardiac recovery and less adverse remodeling. Histologically, this group had higher capillary density. Similarly, sustained CRAMP release from hydrogels enhanced the therapeutic effect of SDF-1, leading to enhanced functional recovery, smaller scar size and higher capillary density.
Conclusion
Cathelicidins enhance BMMNC retention and recruitment after intramyocardial administration post-AMI resulting in improvements in heart physiology and recovery. Therapies employing these strategies may represent an attractive method for improving outcomes of regenerative therapies in human studies.









Similar content being viewed by others
Abbreviations
- AMI:
-
Acute Myocardial Infarction
- BM:
-
Bone Marrow
- BMMNCs:
-
Bone Marrow mononuclear cells
- CRAMP:
-
Cathelicidin-related antimicrobial peptides
- EF:
-
Ejection Fraction
- ESV:
-
End Systolic Volume
- LAD:
-
Left Anterior Descending Artery
- LV:
-
Left Ventricle
- PB:
-
Peripheral Blood
References
Roger, V. L., Go, A. S., Lloyd-Jones, D. M., et al. (2011). Heart disease and stroke statistics--2011 update: A report from the American Heart Association. Circulation, 123, e18–e209.
McMurray, J., & Pfeffer, M. (2005). Heart failure. Lancet, 365, 1877–1889.
Sanganalmath, S. K., & Bolli, R. (2013). Cell therapy for heart failure: A comprehensive overview of experimental and clinical studies, current challenges, and future directions. Circulation Research, 113, 810–834.
Zanetti, M., Gennaro, R., & Romeo, D. (1995). Cathelicidins: A novel protein family with a common proregion and a variable C-terminal antimicrobial domain. FEBS Letters, 374, 1–5.
Youn, S. W., Lee, S. W., Lee, J., et al. (2011). COMP-Ang1 stimulates HIF-1alpha-mediated SDF-1 overexpression and recovers ischemic injury through BM-derived progenitor cell recruitment. Blood, 117, 4376–4386.
McQuibban, G. A., Butler, G. S., Gong, J. H., et al. (2001). Matrix metalloproteinase activity inactivates the CXC chemokine stromal cell-derived factor-1. The Journal of Biological Chemistry, 276, 43503–43508.
McQuibban, G. A., Gong, J. H., Wong, J. P., Wallace, J. L., Clark-Lewis, I., & Overall, C. M. (2002). Matrix metalloproteinase processing of monocyte chemoattractant proteins generates CC chemokine receptor antagonists with anti-inflammatory properties in vivo. Blood, 100, 1160–1167.
Purcell, B. P., Elser, J. A., Mu, A., Margulies, K. B., & Burdick, J. A. (2012). Synergistic effects of SDF-1alpha chemokine and hyaluronic acid release from degradable hydrogels on directing bone marrow derived cell homing to the myocardium. Biomaterials, 33, 7849–7857.
MacArthur Jr., J. W., Purcell, B. P., Shudo, Y., et al. (2013). Sustained release of engineered stromal cell-derived factor 1-alpha from injectable hydrogels effectively recruits endothelial progenitor cells and preserves ventricular function after myocardial infarction. Circulation, 128, S79–S86.
Wu, W., Kim, C. H., Liu, R., et al. (2012). The bone marrow-expressed antimicrobial cationic peptide LL-37 enhances the responsiveness of hematopoietic stem progenitor cells to an SDF-1 gradient and accelerates their engraftment after transplantation. Leukemia, 26, 736–745.
Karapetyan, A. V., Klyachkin, Y. M., Selim, S. M., et al. (2013). Bioactive lipids and cationic antimicrobial peptides as new potential regulators for trafficking of bone marrow derived stem cell in patients with acute myocardial infarction. Stem Cells and Development, 22, 1645–1656.
Gao, E., Lei, Y. H., Shang, X., et al. (2010). A novel and efficient model of coronary artery ligation and myocardial infarction in the mouse. Circulation Research, 107, 1445–1453.
Rodell, C. B., Kaminski, A. L., & Burdick, J. A. (2013). Rational design of network properties in guest-host assembled and shear-thinning hyaluronic acid hydrogels. Biomacromolecules, 14, 4125–4134.
Abbott, J. D., Huang, Y., Liu, D., Hickey, R., Krause, D. S., & Giordano, F. J. (2004). Stromal cell-derived factor-1alpha plays a critical role in stem cell recruitment to the heart after myocardial infarction but is not sufficient to induce homing in the absence of injury. Circulation, 110, 3300–3305.
Klyachkin, Y. M., Nagareddy, P. R., Ye, S., et al. (2015). Pharmacological elevation of circulating bioactive Phosphosphingolipids enhances myocardial recovery after acute infarction. Stem Cells Translational Medicine, 4, 1333–1343.
Brenner, W., Aicher, A., Eckey, T., et al. (2004). 111In-labeled CD34+ hematopoietic progenitor cells in a rat myocardial infarction model. Journal of Nuclear Medicine, 45, 512–518.
Kucia, M., Jankowski, K., Reca, R., et al. (2004). CXCR4-SDF-1 signalling, locomotion, chemotaxis and adhesion. J Mol Histol, 35, 233–245.
Marquez-Curtis, L. A., Turner, A. R., Sridharan, S., Ratajczak, M. Z., & Janowska-Wieczorek, A. (2011). The ins and outs of hematopoietic stem cells: Studies to improve transplantation outcomes. Stem Cell Reviews, 7, 590–607.
Agarwal, U., Ghalayini, W., Dong, F., et al. (2010). Role of cardiac myocyte CXCR4 expression in development and left ventricular remodeling after acute myocardial infarction. Circulation Research, 107, 667–676.
Loffredo, F. S., Steinhauser, M. L., Gannon, J., & Lee, R. T. (2011). Bone marrow-derived cell therapy stimulates endogenous cardiomyocyte progenitors and promotes cardiac repair. Cell Stem Cell, 8, 389–398.
Wu, J. M., Hsueh, Y. C., Ch'ang, H. J., et al. (2015). Circulating cells contribute to cardiomyocyte regeneration after injury. Circulation Research, 116, 633–641.
Wojakowski, W., Tendera, M., Kucia, M., et al. (2009). Mobilization of bone marrow-derived Oct-4+ SSEA-4+ very small embryonic-like stem cells in patients with acute myocardial infarction. Journal of the American College of Cardiology, 53, 1–9.
Karapetyan, A. V., Klyachkin, Y. M., Selim, S., et al. (2013). Bioactive lipids and cationic antimicrobial peptides as new potential regulators for trafficking of bone marrow-derived stem cells in patients with acute myocardial infarction. Stem Cells and Development, 22, 1645–1656.
Abdel-Latif, A., Zuba-Surma, E. K., Ziada, K. M., et al. (2010). Evidence of mobilization of pluripotent stem cells into peripheral blood of patients with myocardial ischemia. Experimental Hematology, 38, 1131–1142.e1.
Fukuhara, S., Tomita, S., Nakatani, T., Yutani, C., & Kitamura, S. (2005). Endogenous bone-marrow-derived stem cells contribute only a small proportion of regenerated myocardium in the acute infarction model. The Journal of Heart and Lung Transplantation, 24, 67–72.
Pfosser, A., El-Aouni, C., Pfisterer, I., et al. (2010). NF kappaB activation in embryonic endothelial progenitor cells enhances neovascularization via PSGL-1 mediated recruitment: Novel role for LL37. Stem Cells, 28, 376–385.
Rodell, C. B., MacArthur, J. W., Dorsey, S. M., Wade, R. J., Woo, Y. J., & Burdick, J. A. (2015). Shear-thinning supramolecular hydrogels with secondary autonomous covalent crosslinking to modulate viscoelastic properties. Advanced Functional Materials, 25, 636–644.
Anker, S. D., Coats, A. J., Cristian, G., et al. (2015). A prospective comparison of alginate-hydrogel with standard medical therapy to determine impact on functional capacity and clinical outcomes in patients with advanced heart failure (AUGMENT-HF trial). European Heart Journal, 36, 2297–2309.
Frey, N., Linke, A., Suselbeck, T., et al. (2014). Intracoronary delivery of injectable bioabsorbable scaffold (IK-5001) to treat left ventricular remodeling after ST-elevation myocardial infarction: A first-in-man study. Circulation. Cardiovascular Interventions, 7, 806–812.
Lee, R. J., Hinson, A., Bauernschmitt, R., et al. (2015). The feasibility and safety of Algisyl-LVR as a method of left ventricular augmentation in patients with dilated cardiomyopathy: Initial first in man clinical results. International Journal of Cardiology, 199, 18–24.
Acknowledgments
Dr. Abdel-Latif is supported by the University of Kentucky Clinical and Translational Science Pilot Award (UL1TR000117), the UK COBRE Early Career Program (P20 GM103527) and the NIH Grant R56 HL124266. Dr. Nagareddy is supported by the NIH Pathway to Independence Award (1K99HL122505-01). Dr. Ye is supported by the T32 grant (HL091812). Dr. Ratajczak is supported by NIH grants 2R01 DK074720 and R01HL112788. Christopher B. Rodell is supported by an American Heart Association Predoctoral Fellowship. Jason A. Burdick is supported by an American Heart Association Established Investigator Award.
Author information
Authors and Affiliations
Contributions
Yuri Klyachkin: conception and design, data analysis and interpretation and manuscript writing. Amr Idris: conception and design, data analysis and interpretation and manuscript writing. Christopher B. Rodell: conception and design, synthesis and preparation of hydrogels, data analysis and interpretation and manuscript writing. Himi Tripathi: collection and/or assembly of data and data analysis and interpretation. Shaojing Ye: collection and/or assembly of data and data analysis and interpretation. Prabakara Nagareddy: collection and/or assembly of data and data analysis and interpretation. Ahmed Asfour: collection and/or assembly of data. Erhe Gao: collection and/or assembly of data. Rahul Annabathula: collection and/or assembly of data. Jason A Burdick: conception and design, data interpretation and manuscript writing. Mariusz Ratajczak: conception and design, data analysis and interpretation and manuscript writing. Ahmed Abdel-Latif: conception and design, data analysis and interpretation, provision of study material or patients, financial support and manuscript writing.
Corresponding author
Ethics declarations
Conflict of Interest
None
Electronic supplementary material
Supplemental Figure 1
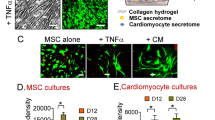
Preincubation with CRAMP increases the retention of transplanted BM cells after myocardial infarction. Representative flow cytometry plots demonstrating the higher percentage of GFP+ BM cells in the heart 4 days after AMI and transplantation (Panel A). Quantitatively, GFP+ cells were 3–4 time higher when preincubated with CRAMP compared to controls (Panel B). Interestingly, BM cells showed higher proliferative state compared to cardiac cells as evident from the percentage of cells in G2M phase (Panel C) and BrdU positive cells (Panel D). Values are mean ± SEM (*P < 0.05, **P < 0.001 vs. HG, N = 3 animals/group). BMMNCs; bone marrow mononuclear cells, CRAMP; cathelicidin related antimicrobial peptide, GFP; green fluorescence protein. (PNG 49 kb)
Supplemental Figure 2
Limited numbers of GFP+ bone marrow cells identified in the heart 5 weeks after transplantation. Representative confocal images demonstrating single and rare GFP (green) labelled bone marrow cells in cardiac sections at 5 weeks after AMI in mice treated with CRAMP-preincubated BMMNCs. Scale bars represent 50 μm. (PNG 203 kb)
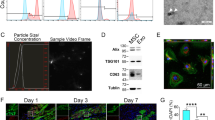
Supplemental Figure 3
CRAMP incubation enhances CXCR4 expression on bone marrow-derived stem cells. Quantitative analysis of the median fluorescence intensity (MFI) and geometric mean of CXCR4 expression, as assessed by flow cytometry, on Lin-/cKit+ bone marrow-derived cells at various time points after CRAMP incubation. CXCR4 (APC) signal intensity peaked at 3 h after CRAMP incubation. Values are mean ± SEM (*P < 0.05, **P < 0.01, **P < 0.001 vs. 1 h, N = 3). (PNG 30 kb)
Supplemental Figure 4
HG supplementation with SDF-1, HF or both enhances cardiomyocyte turnover. Representative confocal images demonstrating BrdU+ (white) cardiomyocytes (red) in the peri-infarct border (Panel A) and remote zone (Panel B) (yellow arrows) at 5 weeks after AMI in mice treated HG alone or supplemented with SDF-1 and/or CRAMP. Panel C-Quantitative analysis of the number of BrdU+ cardiomyocytes per field. Values are mean ± SEM (*P < 0.05, **P < 0.01 vs. HG, N = 3 animals/group). Scale bars represent 50 μm. (PNG 190 kb)
Rights and permissions
About this article
Cite this article
Klyachkin, Y.M., Idris, A., Rodell, C.B. et al. Cathelicidin Related Antimicrobial Peptide (CRAMP) Enhances Bone Marrow Cell Retention and Attenuates Cardiac Dysfunction in a Mouse Model of Myocardial Infarction. Stem Cell Rev and Rep 14, 702–714 (2018). https://doi.org/10.1007/s12015-018-9833-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-018-9833-x