Abstract
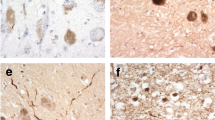
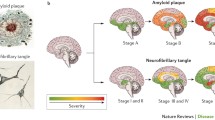
The term paraphrenia refers to a condition characterized by a strong delusional component with preservation of thought and personality. Most affected patients are women. Although a late age at onset (> 60 years) has been proposed in the literature, evidence for this assertion remains debatable. Deterioration of cognitive functions occurs very slowly but may lead to mild dementia over a period of years. Pathological studies indicate the presence of neurofibrillary tangles (NFTs), primarily within the entorhinal cortex. Compared with the severity of neuritic changes, amyloid deposition remains scant. Pyramidal cells affected by NFTs appear to be preserved. Both the clinical history and neuropathology of paraphrenia are similar to those aspects described for NFT-predominant senile dementia. Risk factors, including organic lesions, may precipitate an earlier onset of symptomatology in patients exhibiting this pathology. Many of the symptoms in paraphrenia can be explained by involvement of the entorhinal cortex.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been higlighted as: • Of importance
Berrios GE: The insanities of the third age: a conceptual history of paraphrenia. J Nutr Health Aging 2003, 7:394–399.
Kahlbaum K: Die Gruppirung der psychischen Krankheiten [in German]. Danzig, Germany: Kafemann; 1863.
Berrios GE: Presbyophrenia: the rise and fall of a concept. Psychol Med 1986, 16:267–275.
Kraepelin E: Dementia Praecox and Paraphrenia. Translated by Barclay RM. Edinburgh, Scotland: Livingstone; 1919.
Bianchi L: A Textbook of Psychiatry. London: Bailliere; 1906.
Mayer W: Uber paraphrene Psychosen [in German]. Zentralblatt fur die gesamte Neurologie und Psychiatrie 1921, 26:78–80.
McKenna PJ: Schizophrenia and Related Syndromes. Oxford: Oxford University Press; 1994.
Roth M, Morrissey JD: Problems in the diagnosis and classification of mental disorders in old age. J Ment Sci 1952, 98:66–80.
Roth M: The natural history of mental disorder in old age. J Ment Sci 1955, 101:282–301.
Kay DW, Roth M: Environmental and hereditary factors in the schizophrenias of old age (“late paraphrenia”) and their bearing on the general problem of causation in schizophrenia. J Ment Sci 1961, 107:649–686.
Hassett AM, Keks NA, Jackson HJ, Copolov DL: The diagnostic validity of paraphrenia. Aust N Z J Psychiatry 1992, 26:18–29.
Roth M, Kay DW: Late paraphrenia: a variant of schizophrenia manifest in late life or an organic clinical syndrome? A review of recent evidence. Int J Geriatr Psychiatry 1998, 13:775–784.
Howard R, Rabins P: Late paraphrenia revisited. Br J Psychiatry 1997, 171:406–408.
Howard R, Rabins PV, Seeman MV, Jeste DV: Late-onset schizophrenia and very-late-onset schizophrenia-like psychosis: an international consensus. Am J Psychiatry 2000, 157:172–178.
Ravindran AV, Yatham L, Munro A: Paraphrenia redefined. Can J Psychiatry 1999, 44:133–137.
Casanova MF, Stevens JR, Brown R, et al.: Disentangling the pathology of schizophrenia and paraphrenia. Acta Neuropathol 2002, 103:313–320.
Blessed G, Tomlinson BE, Roth M: The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. Br J Psychiatry 1968, 114:797–811.
Holden NL: Late paraphrenia or the paraphrenias? A descriptive study with a 10-year follow-up. Br J Psychiatry 1987, 150:635–639.
Hymas N, Naguib M, Levy R: Late paraphrenia—a follow-up study. Int J Geriatr Psychiatry 1989, 4:23–29.
Naguib M, Levy R: Late paraphrenia: neuropsychological impairment and structural brain abnormalities on computed tomography. Int J Geriatr Psychiatry 1987, 2:83–90.
• Korner A, Lopez AG, Lauritzen L, et al.: Late and very late first-contact schizophrenia and the risk of dementia—a nationwide register based study. Int J Geriatr Psychiatry 2009, 24:61–67. This study linked the psychiatric and somatic nationwide registers of all inpatients and outpatients in Denmark to examine whether late and very late first-contact schizophrenia carried a risk for later development of dementia. The results showed a two to three times higher risk for both of these patient groups compared with patients with osteoarthritis and the general population.
Brodaty H, Sachdev P, Koschera A, et al.: Long-term outcome of late-onset schizophrenia: 5-year follow-up study. Br J Psychiatry 2003, 103:213–219.
• Girard C, Simard M: Clinical characterization of late- and very late-onset first psychotic episode in psychiatric inpatients. Am J Geriatr Psychiatry 2008, 16:478–487. The article reviews the prevalence and initial symptoms of late- and very late–onset schizophrenia to support the nosological model proposed by the International Late-Onset Schizophrenia Group. Among the symptoms, abnormal psychomotor activity most properly differentiated very late– from late-onset schizophrenia patients.
Fish F: Senile schizophrenia. J Ment Sci 1960, 106:938–946.
Post F: Persistent Persecutory State of the Elderly. Oxford: Pergamon Press; 1966.
Targum SD, Abbott JL: Psychoses in the elderly: a spectrum of disorders. J Clin Psychiatry 1999, 60:4–10.
Petersen RC, Stevens JC, Ganguli M, et al.: Practice parameters: early detection of dementia: mild cognitive impairment (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2001, 56:1133–1142.
Reeves RR, Brister JC: Psychosis in late life: emerging issue. J Psychosoc Nurs 2008, 46:45–53.
Burns A, Forstl H: Neuropathological and neuroradiological correlates of paranoid symptoms in organic mental disease. Eur Arch Psychiatry Clin Neurosci 1997, 247:190–194.
Naguib M: Paraphrenia revisited. Br J Hosp Med 1991, 46:371–375.
Blessed G: Clinicopathological studies in mental disorder of old age: the Newcastle studies 1963–1977. In Contemporary Theses in Psychiatry. Edited by Davison K, Kerr A. Oxford: Gaskell, Alden; 1989:314–321.
Naguib M, McGuffin P, Levy R, et al.: Genetic markers in late paraphrenia—a study of HLA antigens. Br J Psychiatry 1987, 150:124–127.
Kay DW: Outcome and cause of death in mental disorders of old age: a long-term follow-up study of functional and organic psychoses. Acta Psychiatr Scand 1962, 38:249–276.
Bozikas VP, Kovari E, Bouras C, Karavatos A: Neurofibrillary tangles in elderly patients with late onset schizophrenia. Neurosci Lett 2002, 324:109–112.
Casanova MF: Preservation of hippocampal pyramidal cells in paraphrenia. Schizophr Res 2003, 62:141–146.
Bobinski M, Wegiel J, Tamawski M, et al.: Duration of neurofibrillary changes in the hippocampal pyramidal neurons. Brain Res 1998, 799:156–158.
Casanova MF, Lindzen EC: Changes in gray-/white matter ratios in the parahippocampal gyri of paraphrenic patients. Am J Geriatr Psychiatry 2003, 11:605–609.
• Jellinger KA, Attems J: Neurofibrillary tangle predominant dementia: comparison with classical Alzheimer disease. Acta Neuropathol 2007, 113:107–117. The article presents a comprehensive review of the history, nomenclature, and neuropathology of NFT-predominant dementia. The main author boasts one of the biggest series of autopsy cases on the subject.
Casanova MF, Struble RG, Whitehouse PJ, Price DL: A historical perspective on the neuropathology of dementia with emphasis on the senile plaque. Bol Asoc Med P R 1988, 80:424–428.
Simchowicz T: Histologische studien über die senile demenz. In Histologische und histopathologische Arbeiten über die Grosshirnrinde mit besonderer Berücksichtigung der pathologischen Anatomie der Geisteskrankheiten, edn 4 [in German]. Edited by Nissl F, Alzheimer A. Jena, Germany: Fischer; 1911:267–444.
Alzheimer A: Uber eigenartige Krankheitsfalle des spateren Alters [in German]. Z ges Neurol Psychiatr 1911, 4:356–385.
Schnitzler JG: Zur abgrenzung der sogenannten Alzheimerschen Krankheit [in German]. Z ges Neurol Psychiatr 1911, 7:34–57.
Terry RD, Hansen LA, DeTeresa R, et al.: Senile dementia of the Alzheimer type without neocortical neurofibrillary tangles. J Neuropathol Exp Neurol 1987, 46:262–268.
Ulrich J, Spillantini MG, Goedert M, et al.: Abundant neurofibrillary tangles without senile plaques in a subset of patients with senile dementia. Neurodegeneration 1992, 1:257–264.
Jellinger KA, Bancher C: Senile dementia with tangles (tangle predominant form of senile dementia). Brain Pathol 1998, 8:367–376.
Yamada M: Senile dementia of the neurofibrillary tangle type (tangle-only dementia): neuropathological criteria and clinical guidelines for diagnosis. Neuropathology 2003, 23:311–317.
Yamada M, Itoh Y, Suematsu N, Mathsushita M: Dementia of the Alzheimer type and related dementias in the aged: DAT subgroups and senile dementia of the neurofibrillary type. Neuropathology 1996, 16:89–98.
Bancher C, Egensperger R, Kosel S, et al.: Low prevalence of apolipoprotein E epsilon 4 allele in the neurofibrillary tangle predominant form of senile dementia. Acta Neuropathol 1997, 94:403–409.
Bancher C, Jellinger KA: Neurofibrillary tangle predominant form of senile dementia of Alzheimer type: a rare subtype in very old subjects. Acta Neuropathol 1994, 88:565–570.
Iseki E, Yamamoto R, Murayama N, et al.: Immunohistochemical investigation of neurofibrillary tangles and their tau isoforms in brains of limbic neurofibrillary tangle dementia. Neurosci Lett 2006, 404:29–33.
Yamada M, Itoh Y, Sodeyama N: Senile dementia of the neurofibrillary tangle type a comparison with Alzheimer’s disease. Dement Geriatr Cogn Disord 2001, 12:117–125.
Yamada M, Itoh Y, Sodeyama N, et al.: Senile dementia of the neurofibrillary tangle type (SD-NFT): a clinical, neuropathological, and molecular genetic study. In Neuroscientific Basis of Dementia. Edited by Tanaka C, McGeer PL, Ihara Y. Basel, Switzerland: Birkhauser-Verlag; 2001:95–99.
Itoh Y, Yamada M, Suematsu N, et al.: An immunohistochemical study of centenarian brains: a comparison. J Neurol Sci 1998, 157:73–81.
Yamada M, Itoh Y, Sodeyama N, et al.: Aging of the human limbic system: observations of the centenarian brains and analyses of genetic risk factors for the senile changes. Neuropathology 1998, 18:228–234.
Hyman BT, Trojanowski JQ: Editorial on consensus recommendations for the postmortem diagnosis of Alzheimer disease from the National Institute on Aging and the Reagan Institute Working Group on diagnostic criteria for the neuropathological assessment of Alzheimer disease. J Neuropathol Exp Neurol 1997, 56:1095–1097.
Inestrosa NC, Marzolo MP, Bonnefont AB: Cellular and molecular basis of estrogen’s neuroprotection. Potential relevance for Alzheimer’s disease. Mol Neurobiol 1998, 17:73–86.
Disclosure
No potential conflict of interest relevant to this article was reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Casanova, M.F. The Pathology of Paraphrenia. Curr Psychiatry Rep 12, 196–201 (2010). https://doi.org/10.1007/s11920-010-0108-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11920-010-0108-8