Abstract
Purpose of Review
The goal of this systematic review is to analyze the effectiveness of bisphosphonates (BPs) to treat bone pain in children and adolescents who have diseases with skeletal involvement.
Recent Findings
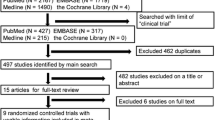
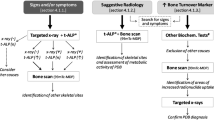
We included 24 studies (2 randomized controlled trials, 3 non-randomized controlled trials, 10 non-randomized open-label uncontrolled studies, 8 retrospective studies, and 1 study with design not specified). The majority of included studies assessed pain from a unidimensional approach, with pain intensity the most frequently evaluated dimension. Only 38% of studies used validated tools; visual analogue scale was the most frequently employed. BPs were used to alleviate bone pain in a wide variety of pediatrics conditions such as osteogenesis imperfecta, secondary osteoporosis, osteonecrosis related to chemotherapy, chronic non-bacterial osteitis, idiopathic juvenile osteoporosis, unresectable benign bone tumor, and cancer-related pain. Twenty of the 24 studies reported a positive effect of BPs for alleviating pain in different pathologies, but 58% of the studies were categorized as having high risk of bias.
Summary
Intravenous BPs are helpful in alleviating bone pain in children and adolescents. It is advised that our results be interpreted with caution due to the heterogeneity of the doses used, duration of treatments, and types of pathologies included. In addition, this review shows the paucity of high-quality evidence in the available literature and further research is needed.
Trial Registration
Before the completion of this review, the protocol was registered to PROSPERO (International prospective register of systematic reviews), PROSPERO 2020 ID # CRD42020158316. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020158316.

Similar content being viewed by others
Change history
29 October 2020
In a previous version of this publication, the author Mercedes Rodriguez Celin’s name was listed as M.R. Celin.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Caes L, et al. A comprehensive categorical and bibliometric analysis of published research articles on pediatric pain from 1975 to 2010. Pain. 2016;157(2):302–13.
Manworren RC, Stinson J. Pediatric pain measurement, assessment, and evaluation. Semin Pediatr Neurol. 2016;23(3):189–200 This seminar evaluates tools used for assesing pain and provides 3 steps for effective pain assesment: record pain history, assess child’s pain with developmentally appropriate tool and evaluate the effectiveness of pain-relieving interventions.
Hill CL, Baird WO, Walters SJ. Quality of life in children and adolescents with Osteogenesis Imperfecta: a qualitative interview based study. Health Qual Life Outcomes. 2014;12:54.
Kruger KM, et al. Mobility in osteogenesis imperfecta: a multicenter North American study. Genet Med. 2019;21(10):2311–8.
Beltramini A, Milojevic K, Pateron D. Pain assessment in newborns, infants, and children. Pediatric annals. 2017;46(10):e387–95 This review proposes a synthesis of the reliable tools to evaluate pain based on the pain context.
Stinson JN, et al. Systematic review of the psychometric properties, interpretability and feasibility of self-report pain intensity measures for use in clinical trials in children and adolescents. Pain. 2006;125(1–2):143–57.
WHO Guidelines Approved by the Guidelines Review Committee, in WHO Guidelines on the Pharmacological Treatment of Persisting Pain in Children with Medical Illnesses. World health organization copyright ©. Geneva: World Health Organization. 2012. p. 2012. These guidelines address the pharmacological management of persisting pain in children with medical illnesses.
Mitchell SAT, Majuta LA, Mantyh PW. New insights in understanding and treating bone fracture pain. Curr Osteoporos Rep. 2018;16(4):325–32 This paper describes recent advances in understanding the mechanisms that drive fracture pain and how these findings are helping to develop new therapies to treat fracture pain.
Dwan K, et al. Bisphosphonate therapy for osteogenesis imperfecta. Cochrane Database Syst Rev. 2016;10(10):Cd005088 The studies included demonstrates BPs increase bone mineral density in children and adults with OI, but do not show BPs conclusively reduce fractures, pain, improve growth and functional mobility.
Fisher JE, et al. Alendronate mechanism of action: geranylgeraniol, an intermediate in the mevalonate pathway, prevents inhibition of osteoclast formation, bone resorption, and kinase activation in vitro. Proc Natl Acad Sci U S A. 1999;96(1):133–8.
George S, et al. Short-term safety of zoledronic acid in young patients with bone disorders: an extensive institutional experience. J Clin Endocrinol Metab. 2015;100(11):4163–71.
Soares AP, et al. Bisphosphonates: Pharmacokinetics, bioavailability, mechanisms of action, clinical applications in children, and effects on tooth development. Environ Toxicol Pharmacol. 2016;42:212–7.
Chahine C, et al. Tooth extraction socket healing in pediatric patients treated with intravenous pamidronate. J Pediatr. 2008;153(5):719–20.
Reed MC, et al. Generation of osteoclasts from type 1 Gaucher patients and correlation with clinical and genetic features of disease. Gene. 2018;678:196–206.
Black DM, et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet. 1996;348(9041):1535–41.
Wong R, Wiffen PJ. Bisphosphonates for the relief of pain secondary to bone metastases. Cochrane Database Syst Rev. 2002;2002(2):Cd002068.
Chevreau M, et al. Bisphosphonates for treatment of Complex Regional Pain Syndrome type 1: A systematic literature review and meta-analysis of randomized controlled trials versus placebo. Joint Bone Spine. 2017;84(4):393–9.
Baroncelli GI, Bertelloni S. The use of bisphosphonates in pediatrics. Horm Res Paediatr. 2014;82(5):290–302 This review provides a summary on some aspects of the structure, mechanisms of action, pharmacokinetics, and bioavailability of BPs, focused on the treatment in pediatric patients.
Varenna M, Adami S, Sinigaglia L. Bisphosphonates in complex regional pain syndrome type I: how do they work? Clin Exp Rheumatol. 2014;32(4):451–4.
Sansoni P, et al. Inhibition of antigen-presenting cell function by alendronate in vitro. J Bone Miner Res. 1995;10(11):1719–25.
Walter PM. Bisphosphonates-anti-inflammatory properties. Current Medicinal Chemistry - Anti-Inflammatory & Anti-Allergy Agents. 2002;1(1):15–28.
Bhadada SK, et al. Fibrous dysplasia & McCune-Albright syndrome: an experience from a tertiary care centre in north India. Indian J Med Res. 2011;133(5):504–9.
Anghelescu DL, et al. Bisphosphonate use in pediatric oncology for pain management. Am J Hosp Palliat Care. 2019;36(2):138–42.
Beecham E, et al. Pharmacological interventions for pain in children and adolescents with life-limiting conditions. Cochrane Database Syst Rev. 2015;2015(3):Cd010750 This review shows that pain was largely evaluated as a secondary outcome and the drugs used for treatment were all adjuvants and was unable to determine the effects of pharmacological interventions for pain in children and young people with life-limiting conditions.
Sułko J, et al. Treatment of chronic recurrent multifocal osteomyelitis with bisphosphonates in children. Joint Bone Spine. 2019;86(6):783–8.
Amin NL, James RM, Phillips R. QUESTION 1: Should we be using bisphosphonates for osteonecrosis complicating childhood acute lymphoblastic leukaemia? Arch Dis Child 2016;101(3):287. This review included studies that used BPs to treat ON in ALL patients. They found methodological flaws in all the studies included, but in some cases, they found a limited evidence that BPs may be beneficial for pain management.
Buckner JL, Bowden SA, Mahan JD. Optimizing bone health in duchenne muscular dystrophy. Int J Endocrinol. 2015;2015:928385.
Marom R, et al. Pharmacological and biological therapeutic strategies for osteogenesis imperfecta. Am J Med Genet C Semin Med Genet. 2016;172(4):367–83.
Plotkin H, et al. Effect of pamidronate treatment in children with polyostotic fibrous dysplasia of bone. J Clin Endocrinol Metab. 2003;88(10):4569–75.
Majoor BC, et al. Outcome of long-term bisphosphonate therapy in mccune-albright syndrome and polyostotic fibrous dysplasia. J Bone Miner Res. 2017;32(2):264–76 This retrospective study done in Polyostotic Fibrous Dysplasia (PFD) and MCcune-Albright Syndrome (MAS) demonstrates a beneficial effect of BPs therapy on bone turnover and pain symptoms in 80% of patients with PFD and in 36% of patients with MAS.
Boyce AM, et al. A randomized, double blind, placebo-controlled trial of alendronate treatment for fibrous dysplasia of bone. J Clin Endocrinol Metab. 2014;99(11):4133–40 This RCT used AL in children and adults with FD. They found that AL led to a reduction in the bone resorption marker NTX-telopeptides, and improvement in aBMD, but no significant effect on serum osteocalcin, pain, or functional parameters.
Bishop N, et al. A randomized, controlled dose-ranging study of risedronate in children with moderate and severe osteogenesis imperfecta. J Bone Miner Res. 2010;25(1):32–40.
Ward LM, et al. Alendronate for the treatment of pediatric osteogenesis imperfecta: a randomized placebo-controlled study. J Clin Endocrinol Metab. 2011;96(2):355–64.
Moher D, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews. 2015;4(1):1.
Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, N.J.: L. Erlbaum Associates; 1988.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Medical Research Methodology. 2005;5(1):13.
McGough JJ, Faraone SV. Estimating the size of treatment effects: moving beyond p values. Psychiatry (Edgmont). 2009;6(10):21–9.
Polanin JR, Snilstveit B. Converting between effect sizes. Campbell Systematic Reviews. 2016;12(1):1–13.
Lee DK. Alternatives to P value: confidence interval and effect size. Korean J Anesthesiol. 2016;69(6):555–62.
van Tulder MW, et al. Empirical evidence of an association between internal validity and effect size in randomized controlled trials of low-back pain. Spine. 2009;34(16).
Slim K, et al. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ Journal of Surgery. 2003;73(9):712–6.
de Boer AG, et al. Cancer survivors and unemployment: a meta-analysis and meta-regression. Jama. 2009;301(7):753–62.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74.
August KJ, et al. The use of zoledronic acid in pediatric cancer patients. Pediatr Blood Cancer. 2011;56(4):610–4.
Chow LT. Giant cell rich osteosarcoma revisited-diagnostic criteria and histopathologic patterns, Ki67, CDK4, and MDM2 expression, changes in response to bisphosphonate and denosumab treatment. Virchows Arch. 2016;468(6):741–55.
DeKlotz TR, et al. Sinonasal disease in polyostotic fibrous dysplasia and McCune-Albright Syndrome. Laryngoscope. 2013;123(4):823–8.
Florenzano P, et al. Age-related changes and effects of bisphosphonates on bone turnover and disease progression in fibrous dysplasia of bone. J Bone Miner Res. 2019;34(4):653–60.
Goldsby RE, et al. Feasibility and dose discovery analysis of zoledronic acid with concurrent chemotherapy in the treatment of newly diagnosed metastatic osteosarcoma: a report from the Children's Oncology Group. Eur J Cancer. 2013;49(10):2384–91.
Grossman LS, et al. Initial experience with percutaneous IM rodding of the humeri in children with osteogenesis imperfecta. J Pediatr Orthop. 2018;38(9):484–9.
Ierardo G, et al. Bisphosphonates therapy in children with Osteogenesis imperfecta: clinical experience in oral surgery. Oral Implantol (Rome). 2017;10(3):311–6.
Sağ E, et al. Chronic recurrent multifocal osteomyelitis in children: a single center experience over five years. Turk J Pediatr. 2019;61(3):386–91.
Srinivasan R, et al. Prophylactic oral bisphosphonate therapy in duchenne muscular dystrophy. Muscle Nerve. 2016;54(1):79–85.
Wiedemann A, et al. Annual injection of zoledronic acid improves bone status in children with cerebral palsy and rett syndrome. Calcif Tissue Int. 2019;104(4):355–63.
Bianchi ML, et al. Treatment of low bone density in young people with cystic fibrosis: a multicentre, prospective, open-label observational study of calcium and calcifediol followed by a randomised placebo-controlled trial of alendronate. Lancet Respir Med. 2013;1(5):377–85.
Martín Siguero A, et al. Efficacy and safety of alendronic acid in the treatment of osteoporosis in children. Farm Hosp. 2015;39(6):350–4.
Jia Q, et al. Clinical features and prognostic factors of pediatric spine giant cell tumors: report of 31 clinical cases in a single center. Spine J. 2019;19(7):1232–41.
Bains JS, et al. A multicenter observational cohort study to evaluate the effects of bisphosphonate exposure on bone mineral density and other health outcomes in osteogenesis imperfecta. JBMR Plus. 2019;3(5):e10118.
Lambert AS, et al. Lower incidence of fracture after IV bisphosphonates in girls with Rett syndrome and severe bone fragility. PLoS One. 2017;12(10):e0186941.
Misof BM, et al. Histomorphometry and bone matrix mineralization before and after bisphosphonate treatment in boys with duchenne muscular dystrophy: a paired transiliac biopsy study. J Bone Miner Res. 2016;31(5):1060–9.
Ooi HL, et al. Intravenous zoledronic Acid given every 6 months in childhood osteoporosis. Horm Res Paediatr. 2013;80(3):179–84.
Barros ER, et al. Safety and efficacy of a 1-year treatment with zoledronic acid compared with pamidronate in children with osteogenesis imperfecta. J Pediatr Endocrinol Metab. 2012;25(5-6):485–91.
Kumar C, et al. Zoledronate for Osteogenesis imperfecta: evaluation of safety profile in children. J Pediatr Endocrinol Metab. 2016;29(8):947–52.
Liu Y, et al. Osteogenesis imperfecta type V: Genetic and clinical findings in eleven Chinese patients. Clin Chim Acta. 2016;462:201–9.
Moon SJ, et al. The effect of low-dose intravenous bisphosphonate treatment on osteoporosis in children with quadriplegic cerebral palsy. Korean J Pediatr. 2017;60(12):403–7.
Simm PJ, et al. Zoledronic acid improves bone mineral density, reduces bone turnover and improves skeletal architecture over 2 years of treatment in children with secondary osteoporosis. Bone. 2011;49(5):939–43.
Paksu MS, et al. Osteopenia in children with cerebral palsy can be treated with oral alendronate. Childs Nerv Syst. 2012;28(2):283–6.
Binh HD, et al. The clinical features of osteogenesis imperfecta in Vietnam. Int Orthop. 2017;41(1):21–9.
Patıroğlu T, et al. Treatment of thalassemia-induced osteoporosis with intermittent pamidronate infusions: Two-year follow up. Turk J Haematol. 2008;25(2):79–82.
Agarwala S, Vijayvargiya M. Bisphosphonate combination therapy for non-femoral avascular necrosis. J Orthop Surg Res. 2019;14(1):112.
Agarwala S, Banavali SD, Vijayvargiya M. Bisphosphonate combination therapy in the management of postchemotherapy avascular necrosis of the femoral head in adolescents and young adults: a retrospective study from India. J Glob Oncol. 2018;4:1–11.
Bousson V, et al. An open-label, prospective, observational study of the efficacy of bisphosphonate therapy for painful osteoid osteoma. Eur Radiol. 2018;28(2):478–86.
Han, J., et al. Comparison of clinical effect in treatment of bone tumor between zoledronic acid needle and ibandronate needle. Pak J Pharm Sci. 2018;31(4(Special)):1683-6.
Henderson BD, et al. Pamidronate treatment for osteogenesis imperfecta in black South Africans. S Afr Med J. 2016;106(6 Suppl 1):S47–9.
Otto S, et al. Ibandronate treatment of diffuse sclerosing osteomyelitis of the mandible: Pain relief and insight into pathogenesis. J Craniomaxillofac Surg. 2015;43(9):1837–42.
Wang Y, et al. Efficacy and safety of bisphosphonate therapy in mccune-albright syndrome-related polyostotic fibrous dysplasia: a single-center experience. Endocr Pract. 2019;25(1):23–30.
Girschick H, et al. The multifaceted presentation of chronic recurrent multifocal osteomyelitis: a series of 486 cases from the Eurofever international registry. Rheumatology (Oxford). 2018;57(7):1203–11.
Aslan MT, et al. Retrospective evaluation of patients diagnosed with osteo-genesis imperfecta. Guncel Pediatri-Journal of Current Pediatrics. 2017;15(1):1–5.
Marginean O, et al. Therapy with pamidronate in children with osteogenesis imperfecta. Drug Des Devel Ther. 2017;11:2507–15.
Mungan NO, et al. Comparison of calcitonin and pamidronate treatments in children with osteogenesis imperfecta. Cukurova Med J. 2013;38(4):667–74.
Mungan NO, et al. Evaluation of two different pamidronate treatment protocols in children with osteogenesis imperfecta. Cukurova Medical Journal. 2014;39(3):532–9.
Salehpour S, Tavakkoli S. Cyclic pamidronate therapy in children with osteogenesis imperfecta. J Pediatr Endocrinol Metab. 2010;23(1-2):73–80.
Thomsen MD, Rejnmark L. Clinical and radiological observations in a case series of 26 patients with fibrous dysplasia. Calcif Tissue Int. 2014;94(4):384–95.
Wiggins S, Kreikemeier R. Bisphosphonate therapy and osteogenesis imperfecta: The lived experience of children and their mothers. J Spec Pediatr Nurs. 2017;22(4).
Vuorimies I, et al. Zoledronic acid treatment in children with osteogenesis imperfecta. Horm Res Paediatr. 2011;75(5):346–53.
Bishop N, et al. Risedronate in children with osteogenesis imperfecta: a randomised, double-blind, placebo-controlled trial. Lancet. 2013;382(9902):1424–32.
Chellapandian D, et al. Bisphosphonate therapy in langerhans cell histiocytosis: an international retrospective descriptive study. Blood. 2015;126(23):2209.
Lim SW, et al. Efficacy of pamidronate in pediatric osteosarcoma patients with low bone mineral density. Ann Pediatr Endocrinol Metab. 2016;21(1):21–5.
Lin CH, et al. Cyclic pamidronate infusion for neonatal-onset osteogenesis imperfecta. Pediatr Neonatol. 2014;55(4):306–11.
Pichler K, et al. Bisphosphonates in multicentric osteolysis, nodulosis and arthropathy (MONA) spectrum disorder - an alternative therapeutic approach. Sci Rep. 2016;6:34017.
van de Meent MM, et al. Conservative treatment of children with chronic diffuse sclerosing osteomyelitis/tendoperiostitis of the mandible. J Craniomaxillofac Surg. 2017;45(12):1938–43.
Zhao Y, et al. aggressive therapy reduces disease activity without skeletal damage progression in chronic nonbacterial osteomyelitis. J Rheumatol. 2015;42(7):1245–51.
Sachdeva R, et al. Bone mineral status in pediatric heart transplant recipients: a retrospective observational study of an "at risk" cohort. Pediatr Transplant. 2010;14(3):383–7.
Bartl C, Imhoff A, Bartl R. Treatment of bone marrow edema syndrome with intravenous ibandronate. Arch Orthop Trauma Surg. 2012;132(12):1781–8.
Henry D, et al. Delaying skeletal-related events in a randomized phase 3 study of denosumab versus zoledronic acid in patients with advanced cancer: an analysis of data from patients with solid tumors. Support Care Cancer. 2014;22(3):679–87.
Royle KL, et al. Quality of life during and following sequential treatment of previously untreated patients with multiple myeloma: findings of the Medical Research Council Myeloma IX randomised study. Br J Haematol. 2018;182(6):816–29.
Uei H, Tokuhashi Y, Maseda M. Treatment outcomes of patients with spinal metastases derived from hepatocellular carcinoma. Int J Clin Oncol. 2018;23(5):886–93.
Kostik MM, Kopchak OL. Comparison of different treatment approaches of pediatric chronic non-bacterial osteomyelitis. 2019;39(1):89–96.
Padhye B, et al. Incidence and outcome of osteonecrosis in children and adolescents after intensive therapy for acute lymphoblastic leukemia (ALL). Cancer Med. 2016;5(5):960–7.
Kuijpers SC, et al. Initial results of the treatment of diffuse sclerosing osteomyelitis of the mandible with bisphosphonates. J Craniomaxillofac Surg. 2011;39(1):65–8.
Baroncelli GI, et al. Pamidronate treatment stimulates the onset of recovery phase reducing fracture rate and skeletal deformities in patients with idiopathic juvenile osteoporosis: comparison with untreated patients. J Bone Miner Metab. 2013;31(5):533–43.
Kotecha RS, et al. Use of bisphosphonates for the treatment of osteonecrosis as a complication of therapy for childhood acute lymphoblastic leukaemia (ALL). Pediatr Blood Cancer. 2010;54(7):934–40.
Leblicq C, et al. Effectiveness of pamidronate as treatment of symptomatic osteonecrosis occurring in children treated for acute lymphoblastic leukemia. Pediatr Blood Cancer. 2013;60(5):741–7.
Lee JM, et al. Efficacy of pamidronate in children with low bone mineral density during and after chemotherapy for acute lymphoblastic leukemia and non-Hodgkin lymphoma. Blood Res. 2013;48(2):99–106.
Aström E, et al. Biochemical bone markers in the assessment and pamidronate treatment of children and adolescents with osteogenesis imperfecta. Acta Paediatr. 2010;99(12):1834–40.
Atta I, et al. Effect of intravenous pamidronate treatment in children with osteogenesis imperfecta. J Coll Physicians Surg Pak. 2014;24(9):653–7.
Cornelis F, et al. Bisphosphonate therapy for unresectable symptomatic benign bone tumors: a long-term prospective study of tolerance and efficacy. Bone. 2014;58:11–6.
Garganta MD, et al. Cyclic bisphosphonate therapy reduces pain and improves physical functioning in children with osteogenesis imperfecta. BMC Musculoskelet Disord. 2018;19(1):344.
Howe W, Davis E, Valentine J. Pamidronate improves pain, wellbeing, fracture rate and bone density in 14 children and adolescents with chronic neurological conditions. Dev Neurorehabil. 2010;13(1):31–6.
Kieser DC, et al. Bisphosphonate therapy for spinal aneurysmal bone cysts. Eur Spine J. 2018;27(4):851–8.
Otaify GA, et al. Zoledronic acid in children with osteogenesis imperfecta and Bruck syndrome: a 2-year prospective observational study. Osteoporos Int. 2016;27(1):81–92.
Tsimicalis A, et al. Pain and quality of life of children and adolescents with osteogenesis imperfecta over a bisphosphonate treatment cycle. Eur J Pediatr. 2018;177(6):891–902.
Hofmann C, et al. A standardized clinical and radiological follow-up of patients with chronic non-bacterial osteomyelitis treated with pamidronate. Clin Exp Rheumatol. 2014;32(4):604–9.
Sánchez-Sánchez LM, et al. Zoledronic acid (zoledronate) in children with osteogenesis imperfecta. Gac Med Mex. 2015;151(2):164–8.
Al-Agha AE, Hayatalhazmi RS. Osteoporosis treatment with zoledronic acid in pediatric population at a university hospital in Western Saudi Arabia. A 13-year experience. Saudi Med J. 2015;36(11):1312–8.
Al-Agha AE, Shaikhain TA, Ashour AA. Safety & efficacy of cyclic zoledronic acid therapy on pediatric secondary osteoporosis. Glob J Health Sci. 2016;8(8):48648.
Bhat CS, et al. Chronic non bacterial osteitis- a multicentre study. Pediatr Rheumatol Online J. 2018;16(1):74.
Padhye B, et al. Use of zoledronic acid for treatment of chemotherapy related osteonecrosis in children and adolescents: a retrospective analysis. Pediatr Blood Cancer. 2013;60(9):1539–45.
Pastore S, et al. Chronic nonbacterial osteomyelitis may be associated with renal disease and bisphosphonates are a good option for the majority of patients. Acta Paediatr. 2016;105(7):e328–33.
Wagner S, et al. Tolerance and effectiveness on pain control of Pamidronate® intravenous infusions in children with neuromuscular disorders. Ann Phys Rehabil Med. 2011;54(6):348–58.
Roderick M, et al. Efficacy of pamidronate therapy in children with chronic non-bacterial osteitis: disease activity assessment by whole body magnetic resonance imaging. Rheumatology (Oxford). 2014;53(11):1973–6.
Sousa T, Bompadre V, White KK. Musculoskeletal functional outcomes in children with osteogenesis imperfecta: associations with disease severity and pamidronate therapy. J Pediatr Orthop. 2014;34(1):118–22.
Nghiem T, et al. Pain experiences of children and adolescents with osteogenesis imperfecta: an integrative review. Clin J Pain. 2017;33(3):271–80 This integrative review shows that research on OI has focused very little on pain experience in children and adolescents, and there is no standard method of assessing pain.
Eiser C, Varni JW. Health-related quality of life and symptom reporting: similarities and differences between children and their parents. Eur J Pediatr. 2013;172(10):1299–304.
Te Winkel ML, et al. Management and treatment of osteonecrosis in children and adolescents with acute lymphoblastic leukemia. Haematologica. 2014;99(3):430–6.
Buch K, et al. Chronic non-bacterial osteomyelitis: a review. Calcif Tissue Int. 2019;104(5):544–53 This review states that treatment of CNBO consists of alleviating symptoms with NSAIDs since the disease is often self-limiting, but more active treatments using either BPs or biological treatment are becoming more common, to prevent long term bone damage.
Miettunen PM, et al. Dramatic pain relief and resolution of bone inflammation following pamidronate in 9 pediatric patients with persistent chronic recurrent multifocal osteomyelitis (CRMO). Pediatr Rheumatol Online J. 2009;7:2.
Lange T, et al. Denosumab: a potential new and innovative treatment option for aneurysmal bone cysts. Eur Spine J. 2013;22(6):1417–22.
Tsagozis P, Brosjö O. Current strategies for the treatment of aneurysmal bone cysts. Orthop Rev (Pavia). 2015;7(4):6182.
Goldbloom EB, Cummings EA, Yhap M. Osteoporosis at presentation of childhood ALL: management with pamidronate. Pediatr Hematol Oncol. 2005;22(7):543–50.
Rauch F, et al. Risedronate in the treatment of mild pediatric osteogenesis imperfecta: a randomized placebo-controlled study. J Bone Miner Res. 2009;24(7):1282–9.
Seikaly MG, et al. Impact of alendronate on quality of life in children with osteogenesis imperfecta. J Pediatr Orthop. 2005;25(6):786–91.
Biggin A, Munns CF. Long-term bisphosphonate therapy in osteogenesis imperfecta. Curr Osteoporos Rep. 2017;15(5):412–8 This review summarizes the knowledge about long-term BP use in OI with recommendations on clinical application.
Constantino CS, et al. Effect of bisphosphonates on function and mobility among children with osteogenesis imperfecta: a systematic review. JBMR Plus. 2019;3(10):e10216.
Coluzzi F, Rolke R, Mercadante S. pain management in patients with multiple myeloma: an update. Cancers (Basel). 2019;11(12).
Mhaskar R, et al. Bisphosphonates in multiple myeloma: an updated network meta-analysis. Cochrane Database Syst Rev. 2017;12(12):Cd003188.
Kosharskyy B, et al. Intravenous infusions in chronic pain management. Pain Physician. 2013;16(3):231–49.
Corral-Gudino L, et al. Bisphosphonates for Paget's disease of bone in adults. Cochrane Database Syst Rev. 2017;12(12):Cd004956.
Porta-Sales J, et al. Evidence on the analgesic role of bisphosphonates and denosumab in the treatment of pain due to bone metastases: A systematic review within the European Association for Palliative Care guidelines project. Palliat Med. 2017;31(1):5–25.
Swezey T, et al. Incorporating the patient perspective in the study of rare bone disease: insights from the osteogenesis imperfecta community. Osteoporos Int. 2019;30(2):507–11 In this work, participants referred that fractures and bone fragility are the focus of OI treatment, but several body systems are under-studied. They emphasized breathing, hearing, effects of aging, pain, gastrointestinal problems, mental health, nutrition, menopause/pregnancy, and basilar invagination are concerns not fully addressed.
Fano V, et al. Osteogenesis imperfecta: quality of life in children. Arch Argent Pediatr. 2013;111(4):328–31.
Cuevas-Olivo R, et al. Treatment with bisphosphonates improves the quality of life in patients with diagnosis of osteogenesis imperfecta. Acta Ortop Mex. 2019;33(2):63–6.
Funding
This review was conducted with support from Shriners Hospital from Children, Chicago. Jackeline Simons received support from HHS/NIDILRR ARRT.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Peter Smith reports grants from Shriners Hospital, NIDLLR, and NIH. Jacqueline Simon reports grants from Marquette University. Gerald Harris reports grant support from NIDILRR. Karen Kruger reports grants from Shriners Hospital. Alissa Fial, Mercedes Rodrigues Celin and Joseph, Krzak declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Bone and Joint Pain
Electronic Supplementary Material
ESM 1
(DOCX 29 kb)
Rights and permissions
About this article
Cite this article
Celin, M.R., Simon, J.C., Krzak, J.J. et al. Do Bisphosphonates Alleviate Pain in Children? A Systematic Review. Curr Osteoporos Rep 18, 486–504 (2020). https://doi.org/10.1007/s11914-020-00621-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-020-00621-3