Abstract
Purpose
Biomechanical simulation of anatomical deformations caused by ultrasound probe pressure is of outstanding importance for several applications, from the testing of robotic acquisition systems to multi-modal image fusion and development of ultrasound training platforms. Different approaches can be exploited for modelling the probe–tissue interaction, each achieving different trade-offs among accuracy, computation time and stability.
Methods
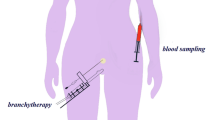
We assess the performances of different strategies based on the finite element method for modelling the interaction between the rigid probe and soft tissues. Probe–tissue contact is modelled using (i) penalty forces, (ii) constraint forces, and (iii) by prescribing the displacement of the mesh surface nodes. These methods are tested in the challenging context of ultrasound scanning of the breast, an organ undergoing large nonlinear deformations during the procedure.
Results
The obtained results are evaluated against those of a non-physically based method. While all methods achieve similar accuracy, performance in terms of stability and speed shows high variability, especially for those methods modelling the contacts explicitly. Overall, prescribing surface displacements is the approach with best performances, but it requires prior knowledge of the contact area and probe trajectory.
Conclusions
In this work, we present different strategies for modelling probe–tissue interaction, each able to achieve different compromises among accuracy, speed and stability. The choice of the preferred approach highly depends on the requirements of the specific clinical application. Since the presented methodologies can be applied to describe general tool–tissue interactions, this work can be seen as a reference for researchers seeking the most appropriate strategy to model anatomical deformation induced by the interaction with medical tools.



Similar content being viewed by others
References
Pheiffer TS, Thompson RC, Rucker DC, Simpson AL, Miga MI (2014) Model-based correction of tissue compression for tracked ultrasound in soft tissue image-guided surgery. Ultrasound Med Biol 40(4):788–803
Burcher MR, Han L, Noble JA (2001) Deformation correction in ultrasound images using contact force measurements. In: Proceedings IEEE workshop on mathematical methods in biomedical image analysis (MMBIA 2001). IEEE, pp 63–70
Priester AM, Natarajan S, Culjat MO (2013) Robotic ultrasound systems in medicine. IEEE Trans Ultrason Ferroelectr Freq Control 60(3):507–523
Huang Q, Lan J, Li X (2018) Robotic arm based automatic ultrasound scanning for three-dimensional imaging. IEEE Trans Industr Inf 15(2):1173–1182
Reckhaus M, Hochgeschwender N, Paulus J, Shakhimardanov A, Kraetzschmar GK (2010) An overview about simulation and emulation in robotics. In: Proceedings of SIMPAR, pp 365–374
Flack B, Makhinya M, Goksel O (2016) Model-based compensation of tissue deformation during data acquisition for interpolative ultrasound simulation. In: 2016 IEEE 13th international symposium on biomedical imaging (ISBI). pp 502–505
Camara M, Mayer E, Darzi A, Pratt P (2017) Simulation of patient-specific deformable ultrasound imaging in real time. In: Imaging for patient-customized simulations and systems for point-of-care ultrasound. Springer, pp 11–18
Petrinec K, Savitsky E, Terzopoulos D (2014) Patient-specific interactive simulation of compression ultrasonography. In: 2014 IEEE 27th international symposium on computer-based medical systems. pp 113–118
Ivaldi S, Peters J, Padois V, Nori F (2014) Tools for simulating humanoid robot dynamics: a survey based on user feedback. In: 2014 IEEE-RAS international conference on humanoid robots. IEEE, pp 842–849
Tagliabue E, Dall’Alba D, Magnabosco E, Tenga C, Peterlik I, Fiorini P (2019) Position-based modeling of lesion displacement in ultrasound-guided breast biopsy. IJCARS 14:1329–1339
Selmi SY, Promayon E, Sarrazin J, Troccaz J (2014) 3D interactive ultrasound image deformation for realistic prostate biopsy simulation. In: Bello F, Cotin S (eds) Biomedical simulation. Springer, Cham, pp 122–130
Horak PC, Trinkle JC (2019) On the similarities and differences among contact models in robot simulation. IEEE Robot Autom Lett 4(2):493–499
Courtecuisse H, Allard J, Kerfriden P, Bordas SP, Cotin S, Duriez C (2014) Real-time simulation of contact and cutting of heterogeneous soft-tissues. Med Image Anal 18(2):394–410
Mahmoud MZ, Aslam M, Alsaadi M, Fagiri MA, Alonazi B (2018) Evolution of robot-assisted ultrasound-guided breast biopsy systems. J Radiat Res Appl Sci 11(1):89–97
Guo R, Lu G, Qin B, Fei B (2017) Ultrasound imaging technologies for breast cancer detection and management: a review. Ultrasound Med Biol 44:37–70
Schenk O, Gärtner K (2004) Solving unsymmetric sparse systems of linear equations with Pardiso. Future Gener Comput Syst 20(3):475–487
Duriez C, Andriot C, Kheddar A (2004) Signorini’s contact model for deformable objects in haptic simulations. In: 2004 IEEE/RSJ international conference on intelligent robots and systems (IROS 2004), vol 4. Proceedings. IEEE, pp 3232–3237
Duriez C, Guébert C, Marchal M, Cotin S, Grisoni L (2009) Interactive simulation of flexible needle insertions based on constraint models. In: International conference on medical image computing and computer-assisted intervention. Springer, pp 291–299
Miller K, Lu J (2013) On the prospect of patient-specific biomechanics without patient-specific properties of tissues. J Mech Behav Biomed Mater 27:154–166
Visentin F, Groenhuis V, Maris B, Dall’Alba D, Siepel F, Stramigioli S, Fiorini P (2018) Iterative simulations to estimate the elastic properties from a series of MRI images followed by MRI-US validation. Med Biol Eng Comput 57:913–924
Marchal M, Allard J, Duriez C, Cotin S (2008) Towards a framework for assessing deformable models in medical simulation. In: International symposium on biomedical simulation. Springer, pp 176–184
Faure F, Duriez C, Delingette H, Allard J, Gilles B, Marchesseau S, Talbot H, Courtecuisse H, Bousquet G, Peterlik I, Cotin S (2012) Sofa: a multi-model framework for interactive physical simulation. In: Soft tissue biomechanical modeling for computer assisted surgery. Springer, pp 283–321
Han L, Hipwell J, Mertzanidou T, Carter T, Modat M, Ourselin S, Hawkes D (2011) A hybrid FEM-based method for aligning prone and supine images for image guided breast surgery. In: 2011 IEEE international symposium on biomedical imaging: from nano to macro. IEEE, pp 1239–1242
Miller K, Joldes G, Lance D, Wittek A (2007) Total lagrangian explicit dynamics finite element algorithm for computing soft tissue deformation. Commun Numer Methods Eng 23(2):121–134
Mendizabal A, Tagliabue E, Brunet JN, Dall’Alba D, Fiorini P, Cotin S (2019) Physics-based deep neural network for real-time lesion tracking in ultrasound-guided breast biopsy. Comput Biomech Med Workshop MICCAI
Acknowledgements
This project has received funding from the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation programme (grant agreement No 742671 “ARS” and No 688188 “MURAB”).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tagliabue, E., Dall’Alba, D., Magnabosco, E. et al. Biomechanical modelling of probe to tissue interaction during ultrasound scanning. Int J CARS 15, 1379–1387 (2020). https://doi.org/10.1007/s11548-020-02183-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-020-02183-2