Abstract
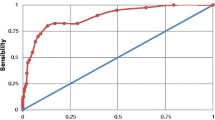
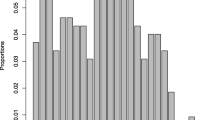
We assessed the sensitivity and specificity of the Self-Reporting Questionnaire (SRQ-20) and the Edinburgh Postnatal Depression Scale (EPDS), against the major depression module of the Mini International Neuropsychiatric Interview (MINI). Data were utilised from antenatal (n = 296) and postnatal participants (n = 366) in the Drakenstein Child Health Study (DCHS), a multidisciplinary birth cohort investigating the determinants of child health. Mothers were interviewed using the SRQ-20, the EPDS and the MINI. Receiver operating characteristic (ROC) curve analysis was performed in order to establish optimal cut-off scores. Current major depressive episode was diagnosed in 5% of antenatal and 4% of postnatal participants. At widely used threshold scores, the sensitivity of the tools ranged from 50 to 67%, although the positive predictive values at these scores were much lower (14–25%). Both tools perform acceptably in identifying mothers at risk for major depression perinatally. In identifying appropriate cut-off scores, optimising specificity and maintaining at least 30% sensitivity seems to be a feasible approach given the resourcing of South African mental health services.

Similar content being viewed by others
References
Altshuler, L. L., Cohen, L. S., Vitonis, A. F., Faraone, S. V., Harlow, B. L., Suri, R., & Stowe, Z. N. (2008). The Pregnancy Depression Scale (PDS): a screening tool for depression in pregnancy. Archives of Women’s Mental Health, 11(4), 277–285. https://doi.org/10.1007/s00737-008-0020-y.
American College of Obstetricians and Gynecologists. (2015). Screening for perinatal depression. Committee Opinion (Vol. 630). Washington, DC: American College of Obstetricians and Gynecologists.
Austin, M. P., Kildea, S., & Sullivan, E. (2007). Maternal mortality and psychiatric morbidity in the perinatal period: challenges and opportunities for prevention in the Australian setting. The Medical Journal of Australia, 186(7), 364–367.
Austin, M. P., Middleton, P., Reilly, N. M., & Highet, N. J. (2013). Detection and management of mood disorders in the maternity setting: the Australian Clinical Practice Guidelines. Women and Birth, 26(1), 2–9. https://doi.org/10.1016/j.wombi.2011.12.001.
Beck, C. T., & Gable, R. K. (2000). Postpartum Depression Screening Scale: Development and psychometric testing. Nursing Research, 49(5), 272–282.
Beck, A. T., & Steer, R. A. (1993). Beck depression inventory manual. San Antonio: Psychological Corporation.
Bennett, H. A., Einarson, A., Taddio, A., Koren, G., & Einarson, T. R. (2004). Prevalence of depression during pregnancy: systematic review. Obstetrics & Gynecology, 103(4), 698–709. https://doi.org/10.1097/01.AOG.0000116689.75396.5f.
Beusenberg, M., & Orley, J. (1994). A user’s guide to the self-reporting questionnaire. Geneva: Division of Mental Health, World Health Organization.
Bhagwanjee, A., Parekh, A., Paruk, Z., Petersen, I., & Subedar, H. (1998). Prevalence of minor psychiatric disorders in an adult African rural community in South Africa. Psychological Medicine, 28(05), 1137–1147.
Brittain, K., Myer, L., Koen, N., Koopowitz, S., Donald, K. A., Barnett, W., & Stein, D. J. (2015). Risk factors for antenatal depression and associations with infant birth outcomes: results from a South African birth cohort study. Paediatric and Perinatal Epidemiology, 29(6), 505–514. https://doi.org/10.1111/ppe.12216.
Chibanda, D., Mangezi, W., Tshimanga, M., Woelk, G., Rusakaniko, P., Stranix-Chibanda, L., et al. (2010). Validation of the Edinburgh Postnatal Depression Scale among women in a high HIV prevalence area in urban Zimbabwe. Archives of Women’s Mental Health, 13(3), 201–206. https://doi.org/10.1007/s00737-009-0073-6.
Cooper, P. J., Tomlinson, M., Swartz, L., Woolgar, M., Murray, L., & Molteno, C. (1999). Post-partum depression and the mother-infant relationship in a South African peri-urban settlement. The British Journal of Psychiatry, 175, 554–558.
Cox, J. L., Holden, J. M., & Sagovsky, R. (1987). Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry, 150, 782–786.
Deeks, J. J., & Altman, D. G. (2004). Statistics notes. Diagnostic tests 4: likelihood ratios. British Medical Journal, 329, 168–169.
Fernandes, M. C., Srinivasan, K., Stein, A. L., Menezes, G., Sumithra, R., & Ramchandani, P. G. (2011). Assessing prenatal depression in the rural developing world: a comparison of two screening measures. Archives of Women’s Mental Health, 14(3), 209–216. https://doi.org/10.1007/s00737-010-0190-2.
Field, T. (2010). Postpartum depression effects on early interactions, parenting, and safety practices: a review. Infant Behavior & Development, 33(1), 1. https://doi.org/10.1016/j.infbeh.2009.10.005.
Fisher, J., de Mello, M. C., Patel, V., Rahman, A., Tran, T., Holton, S., & Holmes, W. (2012). Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bulletin of the World Health Organization, 90, 139–149.
Gavin, N. I., Gaynes, B. N., Lohr, K. N., Meltzer-Brody, S., Gartlehner, G., & Swinson, T. (2005). Perinatal depression: a systematic review of prevalence and incidence. Obstetrics & Gynecology, 106(5, Part 1), 1071–1083. https://doi.org/10.1097/01.AOG.0000183597.31630.db.
Gelman, T., Swartz, L., Tredoux, C., & Strauss, R. (2001). Minor psychiatric morbidity in students attending a South African university health service. Journal of Clinical Psychology in Medical Settings, 8(2), 131–136. https://doi.org/10.1023/a:1009512128351.
Grigoriadis, S., VonderPorten, E. H., Mamisashvili, L., Tomlinson, G., Dennis, C. L., Koren, G., & Ross, L. E. (2013). The impact of maternal depression during pregnancy on perinatal outcomes: a systematic review and meta-analysis. The Journal of Clinical Psychiatry, 74(4), e321–e341. https://doi.org/10.4088/JCP.12r07968.
Halbreich, U., & Karkun, S. (2006). Cross-cultural and social diversity of prevalence of postpartum depression and depressive symptoms. Journal of Affective Disorders, 91(2–3), 97–111. https://doi.org/10.1016/j.jad.2005.12.051.
Halligan, S. L., Murray, L., Martins, C., & Cooper, P. J. (2007). Maternal depression and psychiatric outcomes in adolescent offspring: a 13-year longitudinal study. Journal of Affective Disorders, 97(1–3), 145–154. https://doi.org/10.1016/j.jad.2006.06.010.
Hanlon, C., Medhin, G., Alem, A., Araya, M., Abdulahi, A., Hughes, M., & Prince, M. (2008). Detecting perinatal common mental disorders in Ethiopia: validation of the self-reporting questionnaire and Edinburgh Postnatal Depression Scale. Journal of Affective Disorders, 108(3), 251–262. https://doi.org/10.1016/j.jad.2007.10.023.
Harpham, T., Reichenheim, M., Oser, R., Thomas, E., Hamid, N., Jaswal, S., & Aidoo, M. (2003). Measuring mental health in a cost-effective manner. Health Policy and Planning, 18(3), 344–349. https://doi.org/10.1093/heapol/czg041.
Husain, N., Kiran, T., Sumra, A., Naeem Zafar, S., Ur Rahman, R., Jafri, F., et al. (2014). Detecting maternal depression in a low-income country: comparison of the self-reporting questionnaire and the Edinburgh Postnatal Depression Scale. Journal of Tropical Pediatrics, 60(2), 129–133. https://doi.org/10.1093/tropej/fmt097.
Kessler, R., Andrews, G., Colpe, L., Hiripi, E., Mroczek, D., Normand, S., et al. (2002). Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine, 32(06), 959–976. https://doi.org/10.1017/S0033291702006074.
Koen, N., Brittain, K., Donald, K. A., Barnett, W., Koopowitz, S., Mare, K., et al. (2016). Psychological trauma and posttraumatic stress disorder: risk factors and associations with birth outcomes in the Drakenstein Child Health Study. European Journal of Psychotraumatology, 7, 28720. https://doi.org/10.3402/ejpt.v7.28720.
Kozinszky, Z., & Dudas, R. B. (2015). Validation studies of the Edinburgh Postnatal Depression Scale for the antenatal period. Journal of Affective Disorders, 176, 95–105. https://doi.org/10.1016/j.jad.2015.01.044.
Lawrie, T. A., Hofmeyr, G. J., de Jager, M., & Berk, M. (1998). Validation of the Edinburgh Postnatal Depression Scale on a cohort of South African women. South African Medical Journal, 88(10), 1340–1344.
Mahmud, W. M. R. W., Awang, A., Herman, I., & Mohamed, M. N. (2004). Analysis of the psychometric properties of the Malay version of Beck Depression Inventory II (BDI-II) among postpartum women in Kedah, north west of peninsular Malaysia. The Malaysian journal of medical sciences: MJMS, 11(2), 19.
McMahon, C., Trapolini, T., & Barnett, B. (2008). Maternal state of mind regarding attachment predicts persistence of postnatal depression in the preschool years. Journal of Affective Disorders, 107(1–3), 199–203. https://doi.org/10.1016/j.jad.2007.07.017.
Meltzer-Brody, S., & Stuebe, A. (2014). The long-term psychiatric and medical prognosis of perinatal mental illness. Best Practice & Research. Clinical Obstetrics & Gynaecology, 28(1), 49–60. https://doi.org/10.1016/j.bpobgyn.2013.08.009.
Milgrom, J., & Gemmill, A. W. (2014). Screening for perinatal depression. Best Practice & Research. Clinical Obstetrics & Gynaecology, 28(1), 13–23. https://doi.org/10.1016/j.bpobgyn.2013.08.014.
Natamba, B. K., Achan, J., Arbach, A., Oyok, T. O., Ghosh, S., Mehta, S., et al. (2014). Reliability and validity of the center for epidemiologic studies-depression scale in screening for depression among HIV-infected and -uninfected pregnant women attending antenatal services in northern Uganda: a cross-sectional study. BMC Psychiatry, 14(1), 303. https://doi.org/10.1186/s12888-014-0303-y.
Paschetta, E., Berrisford, G., Coccia, F., Whitmore, J., Wood, A. G., Pretlove, S., & Ismail, K. M. K. (2014). Perinatal psychiatric disorders: an overview. American Journal of Obstetrics and Gynecology, 210(6), 501–509.e506. https://doi.org/10.1016/j.ajog.2013.10.009.
Patel, V., Araya, R., Chowdhary, N., King, M., Kirkwood, B., Nayak, S., et al. (2008). Detecting common mental disorders in primary care in India: a comparison of five screening questionnaires. Psychological Medicine, 38(02), 221–228. https://doi.org/10.1017/S0033291707002334.
Paulden, M., Palmer, S., Hewitt, C., & Gilbody, S. (2009). Screening for postnatal depression in primary care: cost effectiveness analysis. BMJ, 339. doi:https://doi.org/10.1136/bmj.b5203.
Radloff, L. S. (1977). The CES-D scale a self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. https://doi.org/10.1177/014662167700100306.
Rahman, A., Iqbal, Z., Bunn, J., Lovel, H., & Harrington, R. (2004). Impact of maternal depression on infant nutritional status and illness: a cohort study. Archives of General Psychiatry, 61(9), 946–952. https://doi.org/10.1001/archpsyc.61.9.946.
Rochat, T. J., Tomlinson, M., Barnighausen, T., Newell, M. L., & Stein, A. (2011). The prevalence and clinical presentation of antenatal depression in rural South Africa. Journal of Affective Disorders, 135(1–3), 362–373. https://doi.org/10.1016/j.jad.2011.08.011.
Rochat, T. J., Tomlinson, M., Newell, M. L., & Stein, A. (2013). Detection of antenatal depression in rural HIV-affected populations with short and ultrashort versions of the Edinburgh Postnatal Depression Scale (EPDS). Archives of Women’s Mental Health, 16(5), 401–410. https://doi.org/10.1007/s00737-013-0353-z.
Santos, I., Matijasevich, A., Tavares, B., da Cruz Lima, A., Riegel, R., & Lopes, B. (2007). Comparing validity of Edinburgh scale and SRQ20 in screening for post-partum depression. Clinical Practice and Epidemiology in Mental Health, 3(1), 18.
Sawyer, A., Ayers, S., & Smith, H. (2010). Pre- and postnatal psychological wellbeing in Africa: a systematic review. Journal of Affective Disorders, 123(1–3), 17–29. https://doi.org/10.1016/j.jad.2009.06.027.
Siu, A. L., & U.S. Preventive Services Task Force. (2016). Screening for depression in adults: US Preventive Services Task Force recommendation statement. JAMA, 315(4), 380–387. https://doi.org/10.1001/jama.2015.18392.
Spies, G., Stein, D. J., Roos, A., Faure, S. C., Mostert, J., Seedat, S., & Vythilingum, B. (2009). Validity of the Kessler 10 (K-10) in detecting DSM-IV defined mood and anxiety disorders among pregnant women. Archives of Women’s Mental Health, 12(2), 69–74. https://doi.org/10.1007/s00737-009-0050-0.
Stein, A., Pearson, R. M., Goodman, S. H., Rapa, E., Rahman, A., McCallum, M., et al. (2014). Effects of perinatal mental disorders on the fetus and child. The Lancet, 384(9956), 1800–1819. https://doi.org/10.1016/S0140-6736(14)61277-0.
Stein, D. J., Koen, N., Donald, K. A., Adnams, C. M., Koopowitz, S., Lund, C., et al. (2015). Investigating the psychosocial determinants of child health in Africa: the Drakenstein Child Health Study. Journal of Neuroscience Methods. https://doi.org/10.1016/j.jneumeth.2015.03.016.
Stewart, R. C., Umar, E., Tomenson, B., & Creed, F. (2013). Validation of screening tools for antenatal depression in Malawi—a comparison of the Edinburgh Postnatal Depression Scale and Self-Reporting Questionnaire. Journal of Affective Disorders, 150(3), 1041–1047. https://doi.org/10.1016/j.jad.2013.05.036.
Tandon, S. D., Cluxton-Keller, F., Leis, J., Le, H. N., & Perry, D. F. (2012). A comparison of three screening tools to identify perinatal depression among low-income African American women. Journal of Affective Disorders, 136(1–2), 155–162. https://doi.org/10.1016/j.jad.2011.07.014.
Tesfaye, M., Hanlon, C., Wondimagegn, D., & Alem, A. (2010). Detecting postnatal common mental disorders in Addis Ababa, Ethiopia: validation of the Edinburgh Postnatal Depression Scale and Kessler Scales. Journal of Affective Disorders, 122(1–2), 102–108. https://doi.org/10.1016/j.jad.2009.06.020.
Tsai, A. C., Scott, J. A., Hung, K. J., Zhu, J. Q., Matthews, L. T., Psaros, C., & Tomlinson, M. (2013). Reliability and validity of instruments for assessing perinatal depression in African settings: systematic review and meta-analysis. PLoS One, 8(12), e82521. https://doi.org/10.1371/journal.pone.0082521.
van der Westhuizen, C., Wyatt, G., Williams, J., Stein, D., & Sorsdahl, K. (2015). Validation of the Self-Reporting Questionnaire 20-item (SRQ-20) for use in a low- and middle-income country emergency centre setting. International Journal of Mental Health and Addiction, 1–12. doi:https://doi.org/10.1007/s11469-015-9566-x.
Yelland, J. S., Sutherland, G. A., Wiebe, J. L., & Brown, S. J. (2009). A national approach to perinatal mental health in Australia: exercising caution in the roll-out of a public health initiative. Medical Journal of Australia, 191(5), 276–279.
Zubaran, C., Schumacher, M., Roxo, M. R., & Foresti, K. (2010). Screening tools for postpartum depression: validity and cultural dimensions. The African Journal of Psychiatry (Johannesbg), 13(5), 357–365.
Acknowledgements
We would like to acknowledge the Drakenstein Child Health Study staff for their commitment to the research participants and to excellence in research. We acknowledge the mothers and children who have patiently given us their time during the study.
Funding
Dan Stein and Heather Zar are supported by the Medical Research Council of South Africa. Funding for this study was provided by the Bill and Melinda Gates Foundation (grant number OPP1017641) and by the National Institute of Mental Health Brain Disorders in the Developing World: Research Across the Lifespan program (grant number 1R21MH098662-01).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Statement and Approval
All procedures involving human participants were in accordance with the ethical standards of the Faculty of Health Sciences Human Research Ethics Committee, University of Cape Town, by the Stellenbosch University Health Research Ethics Committee, and by the Western Cape Provincial Health Research Committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all patients for being included in the study.
Conflicts of Interest
Authors van der Westhuizen, Brittain, Koen, Zar and Maré declare that they have no conflicts of interest, apart from the funding information given above. In the past 3 years, Prof Stein has received research grants and/or consultancy honoraria from Biocodex, Lundbeck, Servier and Sun. In his career, Prof Stein has received research grants and/or consultancy honoraria from Abbott, ABMRF, Astrazeneca, Biocodex, Eli-Lilly, GlaxoSmithKline, Jazz Pharmaceuticals, Johnson & Johnson, Lundbeck, National Responsible Gambling Foundation, Novartis, Orion, Pfizer, Pharmacia, Roche, Servier, Solvay, Sumitomo, Sun, Takeda, Tikvah and Wyeth.
Rights and permissions
About this article
Cite this article
van der Westhuizen, C., Brittain, K., Koen, N. et al. Sensitivity and Specificity of the SRQ-20 and the EPDS in Diagnosing Major Depression Ante- and Postnatally in a South African Birth Cohort Study. Int J Ment Health Addiction 16, 175–186 (2018). https://doi.org/10.1007/s11469-017-9854-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11469-017-9854-8