Abstract
Background
Lichtheimia species are emerging opportunistic fungal pathogens in the Mucorales, causing serious skin and respiratory infections in immunocompromised patients. Established agents are Lichtheimia corymbifera and L. ramosa, while L. ornata is a novel agent. Available data on a species-specific analysis of Lichtheimia infections are limited.
Methods
The first case of a fatal rhino-orbital-cerebral infection in a hematopoietic stem cell transplantation recipient caused by L. ornata is reported; the agent was identified by sequencing the ITS ribosomal region. We reviewed the literature on mucormycosis due to Lichtheimia species between 2009 and 2018, with an analysis of risk factors and epidemiological and clinical data.
Results
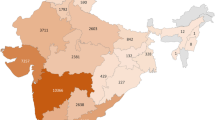
In addition to our Lichtheimia ornata case, 44 cases of human Lichtheimia were analyzed. Lichtheimia predominated in Europe (68.2%), followed by Asia (16%), and Africa (9%). The most common underlying condition was hematological malignancy (36.3%), followed by trauma/major surgery (27.3%), while diabetes mellitus was rare (11.4%). Site of infection was mostly skin and soft tissues (45.5%) and lung (25%), while relatively few cases were disseminated (13.6%) or rhinocerebral (11.4%). Mortality (36.4%) was mainly due to disseminated and rhinocerebral infections.
Conclusion
In contrast to Rhizopus, the most common agent of mucormycosis recorded in patients with diabetes mellitus, Lichtheimia infections were primarily associated with hematological malignancies and major skin barrier damage. Given the fact that classical rhinocerebral mucormycosis remains difficult to treat, independent of causative species, timely application of amphotericin B accessory to debridement may be required for patient survival.





Similar content being viewed by others
References
Schwartze VU, Jacobsen ID. Mucormycoses caused by Lichtheimia species. Mycoses. 2014;57:73–8.
Lanternier F, Dannaoui E, Morizot G, Elie C, Garcia-Hermoso D, Huerre M, et al. A global analysis of mucormycosis in France: the RetroZygo Study (2005–2007). Clin Infect Dis. 2012;54(Suppl 1):S35–43.
Guinea J, Escribano P, Vena A, Muñoz P, Martínez-Jiménez MDC, Padilla B, et al. Increasing incidence of mucormycosis in a large Spanish hospital from 2007 to 2015: epidemiology and microbiological characterization of the isolates. PLoS ONE. 2017;12(6):e0179136.
Pana ZD, Seidel D, Skiada A, Groll AH, Petrikkos G, Cornely OA, et al. Invasive mucormycosis in children: an epidemiologic study in European and non-European countries based on two registries. BMC Infect Dis. 2016;16:667.
De Hoog GS, Guarro J, Gené J, Figueras MJ. Atlas of Clinical Fungi. E-version 4.1.4. Utrecht/Reus 2016: Westerdijk Fungal Biodiversity Institute/Universitat Rovira i Virgili.
Schwartze VU, Hoffmann K, Nyilasi I, Vágvölgyi C, de Hoog S, Voigt K, et al. Lichtheimia species exhibit differences in virulence potential. PLoS ONE. 2012;7:e40908.
Alastruey-Izquierdo A, Hoffmann K, de Hoog GS, Rodriguez-Tudela JL, Voigt K, Bibashi E, et al. Species recognition and clinical relevance of the zygomycetous genus Lichtheimia (syn. Absidia pro parte, Mycocladus). J Clin Microbiol. 2010;48:2154–70.
Ronquist F, Huelsenbeck JP. MrBayes 3: Bayesian phylogenetic inference under mixed models. Bioinformatics. 2003;19:1572–4.
CLSI. Reference method for broth dilution antifungal susceptibility testing of filamentous fungi. CLSI standard M38. 3rd ed. Wayne, PA: Clinical and Laboratory Standards Institute; 2017.
Borras R, Rosello P, Chilet M, Bravo D, de Lomas JG, Navarro D. Positive result of the Aspergillus galactomannan antigen assay using bronchoalveolar lavage fluid from a patient with an invasive infection due to Lichtheimia ramosa. J Clin Microbiol. 2010;48:3035–6.
Blazquez D, Ruiz-Contreras J, Fernández-Cooke E, González-Granado I, Delgado MD, Menendez MT, et al. Lichtheimia corymbifera subcutaneous infection successfully treated with amphotericin B. J Pediatric Surg. 2010;45:E13–E1515.
Woo PC, Lau SK, Ngan AH, Tung ET, Leung SY, To KK, et al. Lichtheimia hongkongensis sp. nov., a novel Lichtheimia sp. associated with rhinocerebral, gastrointestinal, and cutaneous mucormycosis. Diagn Microbiol Infect Dis. 2010;66:274–84.
Bibashi E, de Hoog GS, Pavlidis TE, Symeonidis N, Sakantamis A, Walther G. Wound infection caused by Lichtheimia ramosa due to a car accident. Med Mycol. 2012;2:7–10.
Nikitina YA, Klimko NN, Kolbin AS, Boychenko GE, Garbuzova AI, Golubeva V. Successful treatment of pulmonary mucormycosis in a child with aplastic anemia. Oncohematol 2013;8:52–8.
Kleinotiene G, Posiunas G, Raistenskis J, Zurauskas E, Stankeviciene S, Daugelaviciene V, et al. Liposomal amphotericin B and surgery as successful therapy for pulmonary Lichtheimia corymbifera zygomycosis in a pediatric patient with acute promyelocytic leukemia on antifungal prophylaxis with posaconazole. Med Oncol. 2013;30:433.
Guymer C, Khurana S, Suppiah R, Hennessey I, Cooper C. Successful treatment of disseminated mucormycosis in a neutropenic patient with T-cell acute lymphoblastic leukaemia. BMJ Case Rep. 2013;10:1–5.
Eickhardt S, Braendstra P, Clasen-Linde E, Jensen KE, Alhede M, Bjarnsholt T, et al. A non-fatal case of invasive zygomycete (Lichtheimia corymbifera) infection in an allogeneic haematopoietic cell transplant recipient. APMIS 2013;121:456–9.
Irtan S, Lamerain M, Lesage F, Verkarre V, Bougnoux ME, Lanternier F, et al. Mucormycosis as a rare cause of severe gastrointestinal bleeding after multivisceral transplantation. Transpl Infect Dis. 2013;15:E235–E238238.
Cateau E, Randriamalala E, Elsendoorn A, Giot JP, du Sorbier CM, Rodier MH. Fatal-mixed cutaneous zygomycosis–aspergillosis: a case report. Mycopathologia. 2013;176:423–7.
Poirier P, Nourrisson C, Gibold L, Chalus E, Guelon D, Descamp S, et al. Three cases of cutaneous mucormycosis with Lichtheimia spp (ex Absidia/ Mycocladus) in ICU. Possible cross-transmission in an intensive care unit between 2 cases. J Mycol Méd. 2013;23:265–9.
Millon L, Larosa F, Lepiller Q, Legrand F, Rocchi S, Daguindau E, et al. Quantitative polymerase chain reaction detection of circulating DNA in serum for early diagnosis of mucormycosis in immunocompromised patients. Clin Infect Dis. 2013;56:e95–e101.
Klimko NN, Khostelidi SN, Volkova AG, Popova MO, Bogomolova TS, Zuborovskaya LS, et al. Mucormycosis in haematological patients: case report and results of prospective study in Saint Petersburg, Russia. Mycoses. 2014;57:91–6.
Shigemura T, Nakazawa Y, Matsuda K, Motobayashi M, Saito S, Koike K. Evaluation of Mucorales DNA load in cerebrospinal fluid in a patient with possible cerebral mucormycosis treated with intravenous liposomal amphotericin B. Int J Infect Dis. 2014;29:200–2.
Kutlu M, Ergin C. Pulmonary mucormycosis due to Lichtheimia ramosa in a patient with HIV infection. Mycopathologia. 2014;178:111–5.
De Chaumont A, Pierret C, Janvier F, Goudard Y, De Kerangal X, Chapuis O. Mucormycosis: a rare complication of an amputation. Ann Vasc Surg. 2014;28:1035.e15–e19.
Sherif MZ, Iman ME, Nadia AE, Abdel-Ghany K. Mucormycosis in Cairo, Egypt: review of 10 reported cases. Med Mycol. 2014;52:73–80.
Lambert D, Nerot C, Huguenin A, Diallo S, Mzabi A, OhI X, et al. Post-traumatic mucormycosis due to Lichtheimia corymbifera: three case reports. J Mycol Méd. 2014;2:345–50.
Stefan Z, Ralf B. Lichtheimia infection in a lymphoma patient: case report and a brief review of the available diagnostic tools. Mycopathologia. 2016;181:561–6.
Mouronte-Roibás C, Leiro-Fernández V, Botana-Rial M, Ramos-Hernández C, Lago-Preciado G, Fiaño-Valverde C, et al. Lichtheimia ramosa: a fatal case of mucormycosis. Can Respir J. 2016;2016:2178218. https://doi.org/10.1155/2016/2178218.
Tyll T, Lyskova P, Hubka V, Muller M, Zelenka L, Curdova M, et al. Early diagnosis of cutaneous mucormycosis due to Lichtheimia corymbifera after a traffic accident. Mycopathologia. 2016;181:119–24.
Suzuki D, Kobayashi R, Hori D, Kishimoto K, Sano H, Yasuda K, et al. Stem cell transplantation for acute myeloid leukemia with pulmonary and cerebral mucormycosis. Pediatr Int. 2016;58:569–72.
Gupta N, Singh G, Aggarwal K, Thakar A, Xess I. Invasive mucormycosis in a case of aluminium phosphide poisoning. J Clin Diagn Res. 2017;11:001–2.
Geng C, Lv X, Li J, Jiang Q, Yang R, Zhan P. Chronic subcutaneous infection due to Lichtheimia ramosa. J Eur Acad Dermatol Venereol. 2019;33(1):e26–e2929. https://doi.org/10.1111/jdv.15137.
Thielen BK, Barnes AMT, Sabin AP, Huebner B, Nelson S, Wesenberg E, et al. Widespread Lichtheimia infection in a patient with extensive burns: opportunities for novel antifungal agents. Mycopathologia. 2019;184(1):121–8. https://doi.org/10.1007/s11046-018-0281-6.
Garcia-Hermoso D, Hoinard D, Gantier JC, Grenouillet F, Dromer F, Dannaoui E. Molecular and phenotypic evaluation of Lichtheimia corymbifera (formerly Absidia corymbifera) complex isolates associated with human mucormycosis: rehabilitation of L. ramosa. J Clin Microbiol. 2009;47:3862–70.
Schulze B, Rambach G, Schwartze VU, Voigt K, Schubert K, Speth C, et al. Ketoacidosis alone does not predispose to mucormycosis by Lichtheimia in a murine pulmonary infection model. Virulence. 2017;8:1657–67.
Chakrabarti A, Singh R. Mucormycosis in India: unique features. Mycoses. 2014;57(Suppl 3):85–90.
Yang LW, Ho HM, Chien CY. Notes on zygomycetes of Taiwan (X): the genus Lichtheimia in Taiwan. Fung Sci. 2012;27:109–20.
Alastruey-Izquierdo A, Cuesta I, Walther G, Cuenca-Estrella M, Rodriguez-Tudela JL. Antifungal susceptibility profile of human-pathogenic species of Lichtheimia. Antimicrob Agents Chemother. 2010;54(7):3058–60.
Bouchara JP, Chaturvedi V. The curious case of “case report” of infections caused by human and animal fungal pathogens: an educational tool, an online archive, or a format in need of retooling. Mycopathologia. 2018;183(6):879–91.
Acknowledgments
The authors thank Xinlei Fan from Beijing Forestry University and Bingbing Zhang from School of Public Health, Guizhou Medical University, for their important contributions to the methodology.
Funding
This work was supported by the District Science Foundation Program (NSFC No. 81960368) from National Natural Science Foundation of China.
Author information
Authors and Affiliations
Contributions
YJ formulated the hypothesis, carried out strains collection, DNA extraction and sequencing, phylogenetic tree construction, and physiology tests, and participated in the data analysis and manuscript revision; JP drafted the manuscript, carried out the literature search, and performed the systematic analysis and data extraction. CT performed the phylogenetic tree construction and wrote parts of the manuscript. ML and KX had access to the data and participated in preparation of the manuscript. YC participated in the data interpretation and analysis. PEV supervised the statistical analyses and reviewed the manuscript. HL and SdH participated in the design of the study, statistical analysis, and manuscript revision and review. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Statement
The authors confirm that this material is original and has not been published in whole or in part elsewhere; that the manuscript is not currently being considered for publication in another journal; and that all authors have been personally and actively involved in substantive work leading to the manuscript and will hold themselves jointly and individually responsible for its content. In addition, the authors confirm that they have completed the checklist for submission of a case report to Mycopathologia published by Bouchara et al. [40].
Additional information
Handling Editor: José Francisco Cano Lira.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pan, J., Tsui, C., Li, M. et al. First Case of Rhinocerebral Mucormycosis Caused by Lichtheimia ornata, with a Review of Lichtheimia Infections. Mycopathologia 185, 555–567 (2020). https://doi.org/10.1007/s11046-020-00451-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-020-00451-y