Abstract
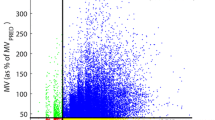
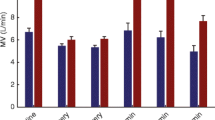
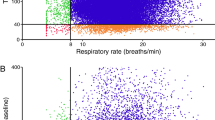
Continuous respiratory assessment is especially important during post-operative care following extubation. Respiratory depression and subsequent adverse outcomes can arise due to opioid administration and/or residual anesthetics. A non-invasive respiratory volume monitor (RVM) has been developed that provides continuous, real-time, measurements of minute ventilation (MV), tidal volume (TV), and respiratory rate (RR) via a standardized set of thoracic electrodes. Previous work demonstrated accuracy of the RVM versus standard spirometry and its utility in demonstrating response to opioids in postoperative patients. This study evaluated the correlation between RVM measurements of MV, TV and RR to ventilator measurements during general anesthesia (GA). Continuous digital RVM and ventilator traces, as well as RVM measurements of MV, TV and RR, were analyzed from ten patients (mean 62.6 ± 7.4 years; body mass index 28.6 ± 5.2 kg/m2) undergoing surgery with GA. RVM data were compared to ventilator data and bias, precision and accuracy were calculated. The average MV difference between the RVM and ventilator was −0.10 L/min (bias: −1.3 %, precision: 6.6 %, accuracy: 9.0 %. The average TV difference was 40 mL (bias: 0.4 %, precision: 7.3 %, accuracy: 9.1 %). The average RR difference was −0.22 breaths/minute (bias: −1.8 %, precision: 3.7 % accuracy: 4.1 %). Correlations between the RVM traces and the ventilator were compared at various points with correlations >0.90 throughout. Pairing the close correlation to ventilator measurements in intubated patients demonstrated by this study with previously described accuracy compared to spirometry in non-intubated patients, the RVM can be considered to have the capability to provide continuity of ventilation monitoring post-extubation This supports the use of real-time continuous RVM measurements to drive post-operative and post-extubation protocols, initiate therapeutic interventions and improve patient safety.




Similar content being viewed by others
References
George JA, Lin EE, Hanna MN, Murphy JD, Kumar K, Ko PS, Wu CL. The effect of intravenous opioid patient-controlled analgesia with and without background infusion on respiratory depression: a meta-analysis. J Opioid Manag. 2010;6(1):47–54.
Jones DA, DeVita MA, Bellomo R. Rapid-response teams. N Engl J Med. 2011;365:139–46.
Ramsay MA, Usman M, Lagow E, Mendoza M, Untalan E, De Vol E. The accuracy, precision and reliability of measuring ventilatory rate and detecting ventilatory pause by rainbow acoustic monitoring and capnometry. Anesth Analg. 2013;117(1):69–75.
American Society of Anesthesiologists: Committee for Standards and Practice Parameters: Standards for basic anesthetic monitoring. October 10, 2010; effective data July 1, 2011.
Futier E, Pereira B, Jaber S. Protective lung ventilation in operating room: systematic review. Minerva Anestesiol. 2014;80:726–35.
Voscopoulos C, Brayanov J, Ladd D, Lalli M, Panasyuk A, Freeman J. Special article: evaluation of a novel noninvasive respiration monitor providing continuous measurement of minute ventilation in ambulatory subjects in a variety of clinical scenarios. Anesth Analg. 2013;117(1):91–100.
Voscopoulos CJ, Ladd D, Brayanov J, George E. Non-invasive respiratory volume monitoring to develop a risk algorithm for the safe use of opioids. Crit Care Med. 2013;41:A16.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307–10.
Marengi N, Brayanov J, England M, MacNabb CM, Campana L, Pham DT, Ianchulev, S. Use of a continuous non-invasive respiratory volume monitor in postoperative cardiac surgery patients before and after endotracheal extubation. Anesth Analg. 2013;116:S-289.
Pesaro C. Opioid-induced sedation and respiratory depression: evidence-based monitoring guidelines. J Perianesth Nurs. 2012;27:208–11.
Willens JS, Junquist CR, Cohen A, Polomano R. ASPM survey-nurses’ practice patterns related to monitoring and preventing respiratory depression. Pain Manag Nurs. 2013;14:60–5.
Fouzas S, Politis P, Skylogianni E, Syriopouloe T, Priftis N, Chatzmichael A, Anthracopoulos MB. Knowledge on pulse oximetry among pediatric health care professionals: a multicenter survey. Pediatrics. 2010;126:e657–63.
Lynn LA, Curry JP. Patterns of unexpected in-hospital deaths: a root cause analysis. Patient Safety in Surgery 2011. BioMed Central, Ltd. www.pssjournal.com/content/5/1/3.
Liu SY, Lee TS, Bongard F. Accuracy of capnography in nonintubated surgical patients. Chest. 1992;102:1512–5.
Cheifetz IM, MacIntyre NR. Respiratory controversies in the critical care setting. Respir Care. 2007;52:636–44.
Good ML. Capnography: uses, interpretation, and pitfalls. JB Lippincott Co., editor. Philadelphia, PA: Amer Soc Anesthesiologists, 1990. p. 1–23. Print.
Kaneko Y. Clinical perspectives on capnography during sedation and general anesthesia in dentistry. Anesth Prog. 1995;42:126–30.
Fu ES, Downs JB, Schweiger JW, Miguel RV, Smith RA. Supplemental oxygen impairs detection of hypoventilation by pulse oximetry. Chest. 2004;126:1552–8.
United States Department of Health and Human Services: Centers for Medicare and Medicaid Services. Requirements for Hospital Medication Administration, Particularly Intravenous (IV) Medications and Post-Operative Care of Patients Receiving IV Opioids. 2014. http://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-14-15.pdf.
Acknowledgments
C. Marshall MacNabb, Dr. Brayanov Dr. Freeman and Dr. Ladd are employed by Respiratory Motion, Inc. Drs. Voscopoulos, Qin, Mullen and George have no financial relationship with Respiratory Motion, Inc.
Conflict of interest
C. Marshall MacNabb, Dr. Brayanov Dr. Freeman and Dr. Ladd are employed by Respiratory Motion, Inc. Drs. Voscopoulos, Qin, Mullen and George declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Voscopoulos, C.J., MacNabb, C.M., Brayanov, J. et al. The evaluation of a non-invasive respiratory volume monitor in surgical patients undergoing elective surgery with general anesthesia. J Clin Monit Comput 29, 223–230 (2015). https://doi.org/10.1007/s10877-014-9596-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-014-9596-0