Abstract
Background
Immunoglobulin A (IgA) autoantibodies to tissue transglutaminase (tTG) are commonly used for screening and diagnosing of celiac disease (CD). Seroreactivity for anti-Saccharomyces cerevisiae antibody (ASCA) and bacterial antigens have also been detected in CD patients. The aim of this study was to examine prospectively serologic responses to microbial targets in adult CD patients at the time of diagnosis and during a gluten-free diet (GFD). Further, we wanted to evaluate whether these serologic specificities could provide new tools for the follow-up of CD patients.
Methods
Data on 55 adult biopsy-proven CD patients were available for follow-up study. Upper gastrointestinal endoscopy was performed on all patients. Sera from patients were tested for antibodies to tTG and ASCA and additionally analyzed with IgA enzyme-linked immunosorbent assays to Pseudomonas fluorescens-associated sequence, I2, and to a Bacteroides caccae TonB-linked outer membrane protein, OmpW.
Results
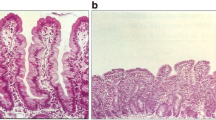
At the time of diagnosis, 91% of CD cases were positive for tTG and 49% for ASCA; positive seroreactivity to I2 was found in 86% and to OmpW in 60% of CD patients at the time of diagnosis. The frequency of seropositivity and serum levels of these antibodies decreased during GFD. Moreover, we found that the decline in the serum levels was significant in all of these markers (p < 0.005). Interestingly, we also found that serum levels of ASCA correlated with the grade of mucosal morphology (p = 0.021), as the ASCA serum levels declined in accordance with mucosal healing.
Conclusions
Commensal enteric bacteria seem to play a role in the small intestinal mucosal damage in CD. This was proven by the serological responses to different microbial antigens shown in this study. Serum levels of ASCA, anti-I2, and anti-OmpW antibodies decreased significantly during GFD, indicating that these serologic markers are gluten dependent in CD patients. These specificities could provide new tools in the follow-up of CD patients.


Similar content being viewed by others
References
Walker-Smith JA, Guandalini S, Schmitz J. Revised criteria for diagnosis of coeliac disease. Arch Dis Child. 1990;65:909–11.
Mäki M, Holm K, Koskimies S, Hällström O, Visakorpi JK. Normal small bowel biopsy followed by coeliac disease. Arch Dis Child. 1990;65:1137–41.
Marsh MN. Gluten, major histocompatibility complex, and the small intestine. A molecular and immunobiologic approach to the spectrum of gluten sensitivity (‘celiac sprue’). Gastroenterology. 1992;102:330–54.
Dieterich W, Ehnis T, Bauer M, Donner P, Volta U, Riecken EO, et al. Identification of tissue transglutaminase as the autoantigen of celiac disease. Nat Med. 1997;3:797–801.
Troncone R, Maurano F, Rossi M, Micillo M, Greco L, Auricchio R, et al. IgA antibodies to tissue transglutaminase: an effective diagnostic test for celiac disease. J Pediatr. 1999;134:166–71.
Salmi TT, Collin P, Järvinen O, Haimila K, Partanen J, Laurila K, et al. Immunoglobulin A autoantibodies against transglutaminase 2 in the small intestinal mucosa predict forthcoming celiac disease. Aliment Pharmacol Ther. 2006;24:541–52.
Nemec G, Ventura A, Stefano M, Di Leo G, Baldas V, Tommasini A, et al. Looking for celiac disease: diagnostic accuracy of two rapid commercial assays. Am J Gastroenterol. 2006;101:1597–600.
Damoiseaux JG, Bouten B, Linders AM, Austen J, Roozendaal C, Russel MG, et al. Diagnostic value of anti-Saccharomyces cerevisiae and antineutrophil cytoplasmic antibodies for inflammatory bowel disease: high prevalence in patients with celiac disease. J Clin Immunol. 2002;22:281–8.
Granito A, Zauli D, Muratori P, Muratori L, Grassi A, Bortolotti R, et al. Anti-saccaharomyces cerevisiae and perinuclear anti-neutrophil cytoplasmic antibodies in coeliac disease before and after gluten-free diet. Aliment Pharmacol Ther. 2005;21:881–7.
Sartor RB. Induction of mucosal immune responses by bacteria and bacterial components. Curr Opin Gastroenterol. 2001;17:555–61.
Ashorn S, Raukola H, Välineva T, Ashorn M, Wei B, Braun J, et al. Elevated serum anti-Saccharomyces Cerevisiae, anti-I2 and anti-OmpW antibody levels in Patients with suspicion of celiac disease. J Clin Immunol. 2008;28:486–94.
Bürgin-Wolff A, Dahlbom I, Hadziselimovic F, Petersson CJ. Antibodies against human tissue transglutaminase and endomysium in diagnosing and monitoring coeliac disease. Scand J Gastroenterol. 2002;37:685–91.
Di Domenico MR, Annaluisa S, Pluvio R, Iovine C, Rea F. The role of anti-endomysium and anti-transglutaminase antibodies in the diagnosis and follow-up of celiac disease. Pediatr Med Chir. 2002;24:208–12.
Kaukinen K, Collin P, Laurila K, Kaartinen T, Partanen J, Mäki M. Resurrection of gliadin antibodies in coeliac disease. Deamidated gliadin peptide antibody test provides additional diagnostic benefit. Scand J Gastroenterol. 2007;19:1–6.
Mallant-Hent RCh, Mary B, von Blomberg E, Yüksel Z, Wahab PJ, Gundy C, et al. Disappearance of anti-Saccharomyces cerevisiae antibodies in coeliac disease during gluten-free diet. Eur J Gastroenterol Hepatol. 2006;18:75–8.
Toumi D, Mankaï A, Belhadj R, Ghedira-Besbes L, Jeddi M, Ghedira I. Anti-Saccharomyces cerevisiae antibodies in coeliac disease. Scand J Gastroenterol. 2007;42:821–6.
Collin P, Kaukinen K, Vogelsang H, Korponay-Szabó I, Sommer R, Schreier E, et al. Antiendomysial and antihuman recombinant tissue transglutaminase antibodies in the diagnosis of coeliac disease: a biopsy-proven European multicentre study. Eur J Gastroenterol Hepatol. 2005;17:85–91.
Amundsen SS, Adamovic S, Hellqvist A, Nilsson S, Gudjónsdóttir AH, Ascher H, et al. A comprehensive screen for SNP associations on chromosome region 5q31-33 in Swedish/Norwegian celiac disease families. Eur J Hum Genet. 2007;15:980–7.
Landers CJ, Cohavy O, Misra R, Yang H, Lin YC, Braun J, et al. Selected loss of tolerance evidenced by Crohn’s disease-associated immune responses to auto- and microbial antigens. Gastroenterology. 2002;123:689–99.
Holm K, Maki M, Savilahti E, Lipsanen V, Laippala P, Koskimies S. Intraepithelial gamma delta T-cell-receptor lymphocytes and genetic susceptibility to coeliac disease. Lancet. 1992;339:1500–3.
Papp M, Norman GL, Altorjay I, Lakatos PL. Utility of serological markers in inflammatory bowel diseases: gadget or magic? World J Gastroenterol. 2007;13:2028–36.
Papp M, Altorjay I, Norman GL, Shums Z, Palatka K, Vitalis Z, et al. Seroreactivity to microbial components in Crohn’s disease is associated with ileal involvement, noninflammatory disease behavior and NOD2/CARD15 genotype, but not with risk for surgery in a Hungarian cohort of IBD patients. Inflamm Bowel Dis. 2007;13:984–92.
Arnott ID, Landers CJ, Nimmo EJ, Drummond HE, Smith BK, Targan SR, et al. Sero-reactivity to microbial components in Crohn’s disease is associated with disease severity and progression, but not NOD2/CARD15 genotype. Am J Gastroenterol. 2004;99:2376–84.
Mow WS, Vasiliauskas EA, Lin YC, Fleshner PR, Papadakis KA, Taylor KD, et al. Association of antibody responses to microbial antigens and complications of small bowel Crohn’s disease. Gastroenterology. 2004;126:414–24.
Peeters M, Geypens B, Claus D, Nevens H, Ghoos Y, Verbeke G, et al. Clustering of increased small intestinal permeability in families in Crohn’s disease. Gasteroenterology. 1997;113:802–07.
Clemente MG, De Virgiliis S, Kang JS, Macatagney R, Musu MP, Di Pierro MR, et al. Early effects of gliadin on enterocyte intracellular signalling involved in intestinal barrier function. Gut. 2003;52:218–23.
Kaila B, Orr K, Bernstein CN. The anti-Saccharomyces cerevisiae antibody assay in a province-wide practice: accurate in identifying cases of Crohn’s disease and predicting inflammatory disease. Can J Gastroenterol. 2005;19:717–21.
van Elburg RM, Uil JJ, Mulder CJ, Heymans HS. Intestinal permeability in patients with coeliac disease and relatives of patients with coeliac disease. Gut. 1993;34:354–7.
Sander GR, Cummins AG, Henshall T, Powell BC. Rapid disruption of intestinal barrier function by gliadin involves altered expression of apical junctional proteins. FEBS Lett. 2005;579:4851–5.
Ciccocioppo R, Finamore A, Ara C, Di Sabatino A, Mengheri E, Corazza GR. Altered expression, localization, and phosphorylation of epithelial junctional proteins in celiac disease. Am J Clin Pathol. 2006;125:502–11.
Acknowledgments
This study was supported by grants from the Paediatric Research Foundation, The Competitive Research Funding of the Pirkanmaa Hospital District, and NIH PO1-DK 46763 (J.B.). The authors would like to acknowledge Ms Leena Ripsaluoma for excellent assistance in recruitment of the patients and Ms Kaija Laurila and Ms Marja-Leena Koskinen for technical support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ashorn, S., Välineva, T., Kaukinen, K. et al. Serological Responses to Microbial Antigens in Celiac Disease Patients During a Gluten-Free Diet. J Clin Immunol 29, 190–195 (2009). https://doi.org/10.1007/s10875-008-9255-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-008-9255-7