Abstract
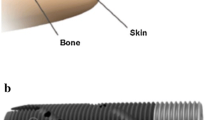
Percutaneous osseointegrated (OI) prostheses directly connect an artificial limb to the residual appendicular skeleton via a permanently implanted endoprosthesis with a bridging connector that protrudes through the skin. The resulting stoma produces unique medical and biological challenges. Previously, a study using a large animal amputation model indicated that infection could be largely prevented, for at least a 12-month period, but the terminal epithelium continued to downgrow. The current study was undertaken to test the longer-term efficacy of this implant construct to maintain a stable skin-implant interface for 24 months. Using the previously successful amputation and implantation surgical procedure, a total of eight sheep were fitted with a percutaneous OI prosthesis. Two animals were removed from the study due to early complications. Of the remaining six sheep, one (16.7%) became infected at 15-months post-implantation and five remained infection-free for the intended 24 months. The histological data of the remaining animals further confirmed the grossly observable epithelial downgrowth. Albeit a receding interface, it was clear that all animals that survived to the end of the study had residual fibrous soft-tissue ingrowth into, and debris within, the exposed titanium porous-coated surface. Overall, the data demonstrated that the porous coated subdermal barrier offered initial protection against infection. However, the fibrous skin attachment was continuously lysed over time by the down-growing epithelium.






Similar content being viewed by others
References
Branemark P-I, Chien S. The osseointegration book: from calvarium to calcaneus. Berlin, London: Quintessenz; 2005.
Pendegrass CJ, Goodship AE, Blunn GW. Development of a soft tissue seal around bone-anchored transcutaneous amputation prostheses. Biomaterials. 2006;27:4183–91.
Kang NV, Pendegrass C, Marks L, Blunn G. Osseocutaneous integration of an intraosseous transcutaneous amputation prosthesis implant used for reconstruction of a transhumeral amputee: case report. J Hand Surg. 2010;35:1130–4.
Juhnke DL, Beck JP, Jeyapalina S, Aschoff HH. Fifteen years of experience with Integral-Leg-Prosthesis: cohort study of artificial limb attachment system. J Rehabil Res Dev. 2015;52:407–20.
Kang NV, Morritt D, Pendegrass C, Blunn G. Use of ITAP implants for prosthetic reconstruction of extra-oral craniofacial defects. J Plast Reconstr Aesthet Surg. 2013;66:497–505.
Jeyapalina S, Beck JP, Bachus KN, Bloebaum RD. Cortical bone response to the presence of load-bearing percutaneous osseointegrated prostheses. Anat Rec. 2012;295:1437–45.
Aschoff HH, Kennon RE, Keggi JM, Rubin LE. Transcutaneous, distal femoral, intramedullary attachment for above-the-knee prostheses: an endo-exo device. J Bone Joint Surg Am. 2010;92:180–6.
Aschoff HH. The endo-exo-femoral prosthesis. Traumatol Orthop Surg Russia. 2011;1:101–5.
Al Muderis M, Khemka A, Lord SJ, Van de Meent H, Frolke JP. Safety of osseointegrated implants for transfemoral amputees: a two-center prospective cohort study. J Bone Joint Surg Am. 2016;98:900–9.
Hagberg K, Branemark R. One hundred patients treated with osseointegrated transfemoral amputation prostheses—rehabilitation perspective. J Rehabil Res Dev. 2009;46:331–44.
Hagberg K, Branemark R, Gunterberg B, Rydevik B. Osseointegrated trans-femoral amputation prostheses: prospective results of general and condition-specific quality of life in 18 patients at 2-year follow-up. Prosthet Orthot Int. 2008;32:29–41.
Rydevik B, Shubayev VI, Myers RR. Osseoperception. In: Brånemark P-I, Chien S, Gröndahl H-G, Robinson K, editors. The osseointegration book from calvarium to calcaneus. Berlin: Quintessenz; 2005. p. 149–56.
Jacobs R, Van Steenberghe D. From osseoperception to implant-mediated sensory-motor interactions and related clinical implications. J Oral Rehabil. 2006;33:282–92.
Hagberg K, Haggstrom E, Jonsson S, Rydevik B, Branemark R. Osseoperception and osseointegrated prosthetic limbs. Psychoprosthetics. London: Springer; 2008. p. 131–40.
Klineberg I. Introduction: from osseointegration to osseoperception. The functional translation. Clin Exp Pharmacol Physiol. 2005;32:97–9.
Branemark R, Berlin O, Hagberg K, Bergh P, Gunterberg B, Rydevik B. A novel osseointegrated percutaneous prosthetic system for the treatment of patients with transfemoral amputation: a prospective study of 51 patients. Bone Joint J. 2014;96B:106–13.
Tillander J, Hagberg K, Hagberg L, Branemark R. Osseointegrated titanium implants for limb prostheses attachments: infectious complications. Clin Orthop Relat Res. 2010;468:2781–8.
Tsikandylakis G, Berlin O, Branemark R. Implant survival, adverse events, and bone remodeling of osseointegrated percutaneous implants for transhumeral amputees. Clin Orthop Relat Res. 2014;472:2947–56.
Jeyapalina S, Beck JP, Bachus KN, Williams DL, Bloebaum RD. Efficacy of a porous-structured titanium subdermal barrier for preventing infection in percutaneous osseointegrated prostheses. J Orthop Res. 2012;30:1304–11.
Holt BM, Bachus KN, Beck JP, Bloebaum RD, Jeyapalina S. Immediate post-implantation skin immobilization decreases skin regression around percutaneous osseointegrated prosthetic implant systems. J Biomed Mater Res A. 2013;101:2075–82.
Holt BM, Betz DH, Ford TA, Beck JP, Bloebaum RD, Jeyapalina S. Pig dorsum model for examining impaired wound healing at the skin-implant interface of percutaneous devices. J Mater Sci Mater Med. 2013;24:2181–93.
Isackson D, McGill LD, Bachus KN. Percutaneous implants with porous titanium dermal barriers: an in vivo evaluation of infection risk. Med Eng Phys. 2011;33:418–26.
Mitchell SJ, Jeyapalina S, Nichols FR, Agarwal J, Bachus KN. Negative pressure wound therapy limits downgrowth in percutaneous devices. Wound Repair Regen. 2016;24:35–44.
von Recum AF. Applications and failure modes of percutaneous devices: a review. J Biomed Mater Res. 1984;18:323–36.
Shelton TJ, Beck JP, Bloebaum RD, Bachus KN. Percutaneous osseointegrated prostheses for amputees: limb compensation in a 12-month ovine model. J Biomech. 2011;44:2601–6.
Emmanual J, Hornbeck C, Bloebaum RD. A polymethyl methacrylate method for large specimens of mineralized bone with implants. Stain Technol. 1987;62:401–10.
Freedberg IM, Tomic-Canic M, Komine M, Blumenberg M. Keratins and the keratinocyte activation cycle. J Invest Dermatol. 2001;116:633–40.
Tomic-Canic M, Komine M, Freedberg IM, Blumenberg M. Epidermal signal transduction and transcription factor activation in activated keratinocytes. J Dermatol Sci. 1998;17:167–81.
Gerritsen M, Lutterman JA, Jansen JA. Wound healing around bone-anchored percutaneous devices in experimental diabetes mellitus. J Biomed Mater Res. 2000;53:702–9.
Gerritsen M, Lutterman JA, Jansen JA. The influence of impaired wound healing on the tissue reaction to percutaneous devices using titanium fiber mesh anchorage. J Biomed Mater Res. 2000;52:135–41.
Jansen JA, Paquay YG, van der Waerden JP. Tissue reaction to soft-tissue anchored percutaneous implants in rabbits. J Biomed Mater Res. 1994;28:1047–54.
Jansen JA, van der Waerden JP, de Groot K. Epithelial reaction to percutaneous implant materials: in vitro and in vivo experiments. J Invest Surg. 1989;2:29–49.
Chehroudi B, Brunette DM. Subcutaneous microfabricated surfaces inhibit epithelial recession and promote long-term survival of percutaneous implants. Biomaterials. 2002;23:229–37.
Pendegrass CJ, Goodship AE, Price JS, Blunn GW. Nature’s answer to breaching the skin barrier: an innovative development for amputees. J Anat. 2006;209:59–67.
Sullivan J, Uden M, Robinson KP, Sooriakumaran S. Rehabilitation of the trans-femoral amputee with an osseointegrated prosthesis: the United Kingdom experience. Prosthet Orthot Int. 2003;27:114–20.
Jansen JA, van der Waerden JP, van der Lubbe HB, de Groot K. Tissue response to percutaneous implants in rabbits. J Biomed Mater Res. 1990;24:295–307.
Hugate R, Clarke R, Hoeman T, Friedman A. Transcutaneous implants in a porcine model: the use of highly porous tantalum. Int J Adv Mater Res. 2015;1:32–40.
Acknowledgements
This research is supported by the Department of Defense (W81XWH-11-1-0435) grant, the Office of Rehabilitation R&D Service, DVA SLC HCS, the Albert & Margaret Hofmann Chair, and the Department of Orthopaedics, University of Utah School of Medicine, Salt Lake City. Authors would like to express their sincere gratitude to the DJO Global for supplying the implants, and IMDS Inc. for animal study support. Authors also would like to thank Roy D. Bloebaum, Ph.D., and his team at the Bone and Joint Research Laboratory, SLC VA Medical Center for embedding the post-mortem samples and for acquiring the SEM data. While the US Army Medical Research Acquisition Activity (Fort Detrick, MD, USA) awarded and administering acquisition office for this study, the content of this research does not necessarily reflect the position or the policy of the Government, and no official endorsement should be inferred.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declares that they have no competing interests.
Rights and permissions
About this article
Cite this article
Jeyapalina, S., Beck, J., Agarwal, J. et al. A 24-month evaluation of a percutaneous osseointegrated limb-skin interface in an ovine amputation model. J Mater Sci: Mater Med 28, 179 (2017). https://doi.org/10.1007/s10856-017-5980-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-017-5980-x