Abstract
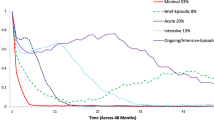
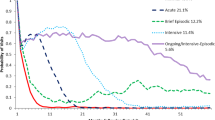
This longitudinal study examined the parallel trajectories of mental health service use and mental health status among children placed in Florida out-of-home care. The results of growth curve modeling suggested that children with greater mental health problems initially received more mental health services. Initial child mental health status, however, had no effect on subsequent service provision when all outpatient mental health services were included. When specific types of mental health services, such as basic outpatient, targeted case management, and intensive mental health services were examined, results suggested that children with compromised functioning during the baseline period received more intensive mental health services over time. However, this increased provision of intensive mental health services did not improve mental health status, rather it was significantly associated with progressively worse mental health functioning. These findings underscore the need for regular comprehensive mental health assessments focusing on specific needs of the child.


Similar content being viewed by others
References
US Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau (2014) The AFCARS report: preliminary FY 2013 as of July 2014 No. 21. http://www.acf.hhs.gov/programs/cb/resource/afcars-report-21
Farmer EM, Burns BJ, Chapman MV, Phillips SD, Angold A, Costello EJ (2001) Use of mental health services by youth in contact with social services. Soc Serv Rev 75:605–624
Landsverk J, Garland AF, Leslie LK (2002) Mental health services for children reported to child protective services. In: Hendrix CT, Berliner L, Jenny C, Briere J, Reid T (eds) APSAC handbook on child maltreatment, 2nd edn. Sage, Thousand Oaks, pp 487–507
Leslie LK, Landsverk J, Ezzet-Lofstrom R, Tschann JM, Slymen DJ, Garland AF (2000) Children in foster care: factors influencing outpatient mental health service use. Child Abuse Negl 24:465–476
Oswald SH, Heil K, Goldbeck L (2010) History of maltreatment and mental health problems in foster children: a review of the literature. J Pediatr Psychol 35:462–472
Whitted KS, Delavega E, Lennon-Dearing R (2012) The youngest victims of violence: examining the mental health needs of young children who are involved in the child welfare and juvenile justice systems. Child Adolesc Soc Work J 30:181–195
Bilaver LA, Jaudes PK, Koepke D, Goerge RM (1999) The health of children in foster care. Soc Serv Rev 73:401–417
DosReis S, Zito JM, Safer DJ, Soeken KL (2001) Mental health services for youths in foster care and disabled youths. Am J Public Health 91:1094–1099
Kerker BD, Dore MM (2006) Mental health needs and treatment of foster youth: barriers and opportunities. Am J Orthopsychiatry 76:138–147
Petrenko CL, Culhane SE, Garrido EF, Taussig HN (2011) Do youth in out-of-home care receive recommended mental health and educational services following screening evaluations? Child Youth Serv Rev 33:1911–1918
Staudt MM (2003) Mental health services utilization by maltreated children: research findings and recommendations. Child Maltreat 8:195–203
Heneghan A, Stein REK, Hurlburt MS, Zhang J, Rolls-Reutz J, Landsverk J, Horwitz SM (2013) mental health problems in teens investigated by U.S. child welfare agencies. J Adolesc Health 52:634–640
Substance Abuse and Mental Health Services Administration (2013) Table 16. Alcohol dependence or abuse in the past year, by age group and state: percentages, annual averages based on 2011 and 2012 NSDUHs. In 2011–2012 National survey on drug use and health: model-based prevalence estimates (50 states and the District of Columbia) (pp 32–33). Rockville: Substance Abuse and Mental Health Services Administration. http://www.samhsa.gov/data/NSDUH/2k12State/Tables/NSDUHsaeTables2012.pdf
Perou R (2013) Mental health surveillance among children—United States, 2005–2011. US Department of Health and Human Services. Centers for Disease Control and Prevention. http://www.cdc.gov/mmwr/preview/mmwrhtml/su6202a1.htm?s_cid=su6202a1_w
Bronfenbrenner U (1979) The ecology of human development: experiments by nature and design. Harvard University Press, Cambridge
Lochman JE (2004) Contextual factors in risk and prevention research. Merrill Palmer Q (Wayne State Univ Press) 50:311–325
Wert MV, Mishna F, Malti, T (2016) A conceptual model of the relationship between maltreatment and externalizing, antisocial, and criminal behavior problems, and the intervening role of child welfare service delivery. Aggress Violent Behav 29:10–19
Anderson HD (2011) Suicide ideation, depressive symptoms, and out-of-home placement among youth in the U.S. child welfare system. J Clin Child Adolesc Psychol 40:790–796
Bruskas D (2008) Children in foster care: a vulnerable population at risk. J Child Adolesc Psychiatr Nurs 21:70–77
Bruskas D (2010) Developmental health of infants and children subsequent to foster care. J Child Adolesc Psychiatr Nurs 23:231–241
Bellamy JL, Gopalan G, Traube DE (2010) A national study of the impact of outpatient mental health services for children in long-term foster care. Clin Child Psychol Psychiatry 15:467–479
Stiffman AR, Pescosolido B, Cabassa LJ (2004) Building a model to understand youth service access: the gateway provider model. Ment Health Serv Res 6:189–198
Burns BJ, Phillips SD, Wagner HR, Barth RP, Kolko DJ, Campbell Y, Landsverk J (2004) Mental health need and access to mental health services by youths involved with child welfare: a national survey. J Am Acad Child Adolesc Psychiatry 43:960–970
Leslie LK, Hurlburt MS, James S, Landsverk J, Slymen DJ, Zhang J (2005) Relationship between entry into child welfare and mental health service use. Psychiatr Serv 56:981–987
Leslie LK, Hurlburt MS, Landsverk J, Barth R, Slymen DJ (2004) Outpatient mental health services for children in foster care: a national perspective. Child Abuse Negl 28:697–712
Harman JS, Childs GE, Kelleher, KJ (2000) Mental health care utilization and expenditures by children in foster care. Arch Pediatr Adolesc Med 154:1114–1117
Shin SH (2005) Need for and actual use of mental health service by adolescents in the child welfare system. Child Youth Serv Rev 27:1071–1083
Achenbach TM (1991) Manual for the child behavior checklist/4–18 and 1991 profile. University of Vermont Department of Psychiatry, Burlington
US Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau (2012) Child welfare outcomes 2008–2011: Report to Congress. http://archive.acf.hhs.gov/programs/cb/pubs/cwo07-10/cwo07-10.pdf
Tabone JK, Thompson R, Wiley TR (2010) The impact of early mental health services on child behavioral outcomes: comparisons between and within trajectory groups. Child Youth Serv Rev 32:292–297
Kolko DJ, Baumann BL, Caldwell N (2003) Child abuse victims’ involvement in community agency treatment: service correlates, short-term outcomes, and relationship to reabuse. Child Maltreat 8:272–287
Weisz JR, Kazdin AE (eds) (2010) Evidence-based psychotherapies for children and adolescents, 2nd edn. Guilford Press, New York
Yampolskaya S, Mowery D, Sharrock P (2012) Effect of child welfare prepaid mental health plan services on youth outcomes. (Agency for Health Care Administration (AHCA) series 220–155). Louis de la Parte Florida Mental Health Institute, University of South Florida, Tampa
Angold A, Costello EJ, Burns BJ, Erkanli A, Farmer EM (2000) Effectiveness of nonresidential specialty mental health services for children and adolescents in the “real world”. J Am Acad Child Adolesc Psychiatry 39:154–160
Trask EV, Fawley-King K, Garland AF, Aarons GA (2016) Do aftercare mental health services reduce risk of psychiatric rehospitalization for children? Psychol Serv 13:127–132
Gearing RE, Schwalbe CS, Short KD (2012) Adolescent adherence to psychosocial treatment: mental health clinicians’ perspectives on barriers and promoters. Psychother Res 22:317–326
Gopalan G, Goldstein L, Klingenstein K, Sicher C, Blake C, McKay MM (2010) Engaging families into child mental health treatment: updates and special considerations. J Can Acad Child Adolesc Psychiatry 19:182–196
Thompson R (2009) The impact of early mental health services on the trajectory of externalizing behavioral problems in a sample of high-risk pre-adolescent children. Child Youth Serv Rev 31:16–22
Angold A, Erkanli A, Farmer EM, Fairbank JA, Burns BJ, Keeler G, Costello EJ (2002) Psychiatric disorder, impairment, and service use in rural African American and White youth. Arch Gen Psychiatry 59:893–901
Thompson R, May MA (2006) Caregivers’ perceptions of child mental health needs and service utilization: an urban 8-year old sample. J Behav Health Ser Res 33:474–482
Florida Statutes (2013) Chapter 39 (39.01)
Ward JC, Dow MG, Saunders TL, Halls SC, Penner KF, Musante KA, Sachs-Ericcson N (2006) Children’s functional assessment rating scale. University of South Florida, Louis de la Parte Florida Mental Health Institute, Tampa. http://outcomes.fmhi.usf.edu/_assets/docs/cfarsmanual.pdf
Ward JC, Dow MG, Saunders TL, Halls SC, Penner KF, Musante K A et al (2004) The manual of children’s functional assessment rating scale. University of South Florida, Tampa
Achenbach TM (2001) Child behavior checklist for ages 6–18. ASEBA. University of Vermont, Burlington
Michalcin D (2008) A comparison of the children’s functional assessment rating scale and the child behavior checklist used in a wraparound program. Capella University, Ann Arbor
Schwartz RC (1999) Reliability and validity of the functional assessment rating scale. Psychol Rep 84:389–391
Muthén LK, Muthén BO (1998–2015) Mplus user’s guide, 7th edn. Muthén & Muthén, Los Angeles
Preacher KJ, Wichman AL, MacCallum RC, Briggs NE (2008) Latent growth curve modeling. Sage, Thousand Oaks
Muthén LK, Muthén BO (2007) Growth modeling with latent variables using Mplus. Mplus short courses. Muthén & Muthén, Los Angeles
Curran PJ, Hussong AM (2003) The use of latent trajectory models in psychopathology research. J Abnorm Psychol 112:526–544
Bentler PM (1990) Fit indexes, Lagrange multipliers, constraint changes and incomplete data in structural models. Multivar Behav Res 25:163–172
Tucker L, Lewis C (1973) A reliability coefficient for maximum likelihood factor analysis. Psychometrika 38:1–10
MacCallum RC, Browne MW, Sugawara HM (1996) Power analysis and determination of sample size for covariance structure modeling. Psychol Methods 1:130–149
Bollen KA, Long JS (1993) Testing structural equation models. Sage, Newbury Park
Hu LT, Bentler PM (1999) Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling 6:1–55
Horwitz SM, Hurlburt MS, Zhang J (2009) Patterns and predictors of mental health services use by children in contact with the child welfare system. In: Webb MB, Dowd K, Harden BJ, Landsverk J, Testa MF (eds) Child welfare and child well-being. Oxford University Press, Oxford, pp 279–327
Glisson C, Green P (2006) The role of specialty mental health care in predicting child welfare and juvenile justice out-of-home placements. Res Soc Work Pract 16:480–490
Horwitz SM, Hurlburt MS, Goldhaber-Fiebert JD, Heneghan AM, Zhang J, Rolls-Reutz J, Fisher E, Landsverk J, Ruth EK, Stein RE (2012) Mental health services use by children investigated by child welfare agencies. Pediatrics 130:861–869
Fontanella CA, Gupta L, Hiance-Steelesmith DL, Valentine S (2015) Continuity of care for youth in foster care with serious emotional disturbances. Child Youth Serv Rev 50:38–43
Fong HF, French B, Rubin D, Wood JN (2015) Mental health services for children and caregivers remaining at home after suspected maltreatment. Child Youth Serv Rev 58:50–59
Guibord M, Bell T, Romano E, Rouillard L (2011) Risk and protective factors for depression and substance use in an adolescent child welfare sample. Child Youth Serv Rev 33:2127–2137
Funding
The funding was provided by Florida Agency for Health Care Administration (Grant No. MED 134).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yampolskaya, S., Sharrock, P.J., Clark, C. et al. Utilization of Mental Health Services and Mental Health Status Among Children Placed in Out-of-Home Care: A Parallel Process Latent Growth Modeling Approach. Child Psychiatry Hum Dev 48, 728–740 (2017). https://doi.org/10.1007/s10578-016-0699-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-016-0699-3