Abstract
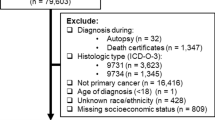
The potential role of socioeconomic status (SES) in the survival of patients with myelodysplastic syndromes (MDS) has not been evaluated. We conducted the first study to assess the prognostic role of neighborhood SES among a cohort of 2,118 patients (age ≥ 66 years) who were diagnosed with incident MDS in the United States during 2001–2002. Principal component analysis was used to develop a summary SES score by combining multiple measures of neighborhood SES. The score was then used to classify the census tract each patient resided in into a category of high, medium, or low SES. Hazard ratios (HRs) were estimated using multivariate Cox proportional hazard models. After adjusting for age, gender, comorbidities, and histological subtypes, compared with MDS patients lived in high-SES census tracts, those resided in medium (HR = 1.14, 95% CI: 1.01–1.30) and low (HR = 1.17, 95% CI: 1.02–1.34) SES census tracts had significantly increased the risks of death. The impact of SES on survival was more apparent for patients with refractory anemia with ringed sideroblasts—patients residing in medium (HR = 1.85, 95% CI: 1.17–2.91) and low (HR = 2.06, 95% CI: 1.27–3.37) census tracts had a nearly two-fold increased the risk of mortality, compared with those living in high-SES census tracts. In conclusion, this population-based study suggests that neighborhood SES status is a significant and independent determinant of survival among elderly patients with MDS in the United States.

Similar content being viewed by others
References
Woods LM, Rachet B, Coleman MP (2006) Origins of socio-economic inequalities in cancer survival: a review. Ann Oncol 17:5–19. doi:10.1093/annonc/mdj007
Kogevinas M, Pearce N, Susser M, et al (eds) (1997) Social inequalities and cancer, IARC Sci Publ No 138. International Agency for Research on Cancer, Lyon, pp 1–15
Auchincloss AH, Van Nostrand JF, Ronsaville D (2001) Access to health care for older persons in the United States: personal, structural, and neighborhood characteristics. J Aging Health 13:329–354. doi:10.1177/089826430101300302
Kirby JB, Kaneda T (2005) Neighborhood socioeconomic disadvantage and access to health care. J Health Soc Behav 46:15–31
Prentice JC (2006) Neighborhood effects on primary care access in Los Angeles. Soc Sci Med 62:1291–1303. doi:10.1016/j.socscimed.2005.07.029
Byers TE, Wolf HJ, Bauer KR et al (2008) The impact of socioeconomic status on survival after cancer in the United States: findings from the National Program of Cancer Registries Patterns of Care Study. Cancer 113:582–591. doi:10.1002/cncr.23567
Rachet B, Mitry E, Shah A, Cooper N, Coleman MP (2008) Survival from non-Hodgkin lymphoma in England and Wales up to 2001. Br J Cancer 99(Suppl 1):S104–S106. doi:10.1038/sj.bjc.6604605
Rachet B, Mitry E, Shah A, Cooper N, Coleman MP (2008) Survival from adult leukaemia in England and Wales up to 2001. Br J Cancer 99(Suppl 1):S116–S118. doi:10.1038/sj.bjc.6604609
Roswall N, Olsen A, Christensen J, Rugbjerg K, Mellemkjaer L (2008) Social inequality and incidence of and survival from Hodgkin lymphoma, non-Hodgkin lymphoma and leukaemia in a population-based study in Denmark, 1994–2003. Eur J Cancer 44:2058–2073. doi:10.1016/j.ejca.2008.06.011
Wang M, Burau KD, Fang S, Wang H, Du XL (2008) Ethnic variations in diagnosis, treatment, socioeconomic status, and survival in a large population-based cohort of elderly patients with non-Hodgkin lymphoma. Cancer 113:3231–3241. doi:10.1002/cncr.23914
Bray C, Morrison DS, McKay P (2008) Socio-economic deprivation and survival of non-Hodgkin lymphoma in Scotland. Leuk Lymphoma 49:917–923. doi:10.1080/10428190801933377
Rodriguez CP, Baz R, Jawde RA et al (2008) Impact of socioeconomic status and distance from treatment center on survival in patients receiving remission induction therapy for newly diagnosed acute myeloid leukemia. Leuk Res 32:413–420. doi:10.1016/j.leukres.2007.07.015
Bennett J (2002) The myelodysplastic syndromes: pathobiology and clinical management. In: Cheson B (ed) Basic and Clinical Oncology, vol 27. Marcel Dekker, New York
Greenberg P, Cox C, LeBeau MM et al (1997) International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood 89:2079–2088
Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF (2002) Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care 40: IV-3–18
Fritz A (ed) (2000) International classification of diseases for oncology, 3rd edn. World Health Organization, Geneva
Piccirillo JF, Spitznagel EL Jr, Vermani N, Costas I, Schnitzler M (2004) Comparison of comorbidity indices for patients with head and neck cancer. Med Care 42:482–486. doi:10.1097/01.mlr.0000124254.88292.a1
Sharma G, Freeman J, Zhang D, Goodwin JS (2008) Trends in end-of-life ICU use among older adults with advanced lung cancer. Chest 133:72–78. doi:10.1378/chest.07-1007
Wong YN, Mitra N, Hudes G et al (2006) Survival associated with treatment vs observation of localized prostate cancer in elderly men. Jama 296:2683–2693. doi:10.1001/jama.296.22.2683
Keating NL, Landrum MB, Meara E, Ganz PA, Guadagnoli E (2005) Do increases in the market share of managed care influence quality of cancer care in the fee-for-service sector? J Natl Cancer Inst 97:257–264
Yost K, Perkins C, Cohen R, Morris C, Wright W (2001) Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control 12:703–711. doi:10.1023/A:1011240019516
Liberatos P, Link BG, Kelsey JL (1988) The measurement of social class in epidemiology. Epidemiol Rev 10:87–121
Liu L, Deapen D, Bernstein L (1998) Socioeconomic status and cancers of the female breast and reproductive organs: a comparison across racial/ethnic populations in Los Angeles County, California (United States). Cancer Causes Control 9:369–380. doi:10.1023/A:1008811432436
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383. doi:10.1016/0021-9681(87)90171-8
Romano PS, Roos LL, Jollis JG (1993) Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol 46:1075–1079. doi:10.1016/0895-4356(93)90103-8 (discussion 1081–1090)
Wang R, Gross CP, Halene S, Ma X (2009) Comorbidities and survival in a large cohort of patients with newly diagnosed myelodysplastic syndromes. Leuk Res. doi:10.1016/j.leukres.2009.02.005
Shadduck RK, Latsko JM, Rossetti JM, Haq B, Abdulhaq H (2007) Recent advances in myelodysplastic syndromes. Exp Hematol 35:137–143. doi:10.1016/j.exphem.2007.01.022
Kasner MT, Luger SM (2009) Update on the therapy for myelodysplastic syndrome. Am J Hematol 84:177–186. doi:10.1002/ajh.21352
Steensma DP, Tefferi A (2007) Risk-based management of myelodysplastic syndrome. Oncology (Williston Park) 21:43–54 (discussion 57–48, 62)
Ma X, Does M, Raza A, Mayne ST (2007) Myelodysplastic syndromes: incidence and survival in the United States. Cancer 109:1536–1542. doi:10.1002/cncr.22570
Boehm A, Sperr WR, Leitner G et al (2008) Comorbidity predicts survival in myelodysplastic syndromes or secondary acute myeloid leukaemia after allogeneic stem cell transplantation. Eur J Clin Invest 38:945–952. doi:10.1111/j.1365-2362.2008.02041.x
Della Porta MG, Kuendgen A, Malcovati L et al (2008) Myelodysplastic Syndrome (MDS)-Specific comorbidity index for predicting the impact of extra-hematological comorbidities on survival of patients with MDS. ASH Annual Meeting Abstracts 112:2677
Pelz D, Nachtkamp K, Kündgen A, Strupp C, Haas R, Germing U (2007) C015 Influence of comorbidity factors on the prognosis of patients with myelodysplastic syndromes (MDS). Leuk Res 31:S30–S31. doi:10.1016/S0145-2126(07)70053-X
Blustein J, Hoy EC (2000) Who is enrolled in for-profit vs. nonprofit Medicare HMOs. Health Aff (Millwood) 19:210–220. doi:10.1377/hlthaff.19.1.210
Do DP, Finch BK (2008) The link between neighborhood poverty and health: context or composition? Am J Epidemiol: kwn182
Macintyre S, Ellaway A, Cummins S (2002) Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med 55:125–139. doi:10.1016/S0277-9536(01)00214-3
Acknowledgments
This work was supported by a grant from the National Cancer Institute (K07 CA119108). Dr Gross’s efforts were supported by Beeson Career Development Award (1 K08 AG24842). The linked SEER–Medicare database was used for this study. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the Applied Research Program, NCI; the Office of Research, Development and Information, CMS; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER–Medicare database.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, R., Gross, C.P., Halene, S. et al. Neighborhood socioeconomic status influences the survival of elderly patients with myelodysplastic syndromes in the United States. Cancer Causes Control 20, 1369–1376 (2009). https://doi.org/10.1007/s10552-009-9362-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-009-9362-7