Abstract
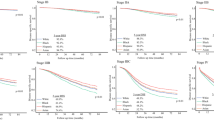
The aim of the study is to determine the influence of area-level socio-economic status and healthcare access in addition to tumor hormone-receptor subtype on individual breast cancer stage, treatment, and mortality among Non-Hispanic (NH)-Black, NH-White, and Hispanic US adults. Analysis was based on 456,217 breast cancer patients in the SEER database from 2000 to 2010. Multilevel and multivariable-adjusted logistic and Cox proportional hazards regression analysis was conducted to account for clustering by SEER registry of diagnosis. NH-Black women had greater area-level access to healthcare resources compared with women of other races. For instance, the average numbers of oncology hospitals per million population in counties with NH-Black, NH-White, and Hispanic women were 8.1, 7.7, and 5.0 respectively; average numbers of medical doctors per million in counties with NH-Black, NH-White, and Hispanic women were 100.7, 854.0, and 866.3 respectively; and average number of Ob/Gyn in counties with NH-Black, NH-White, and Hispanic women was 155.6, 127.4, and 127.3, respectively (all p values <0.001). Regardless, NH-Black women (HR 1.39, 95 % CI 1.36–1.43) and Hispanic women (HR 1.05, 95 % CI 1.03–1.08) had significantly higher breast cancer mortality compared with NH-White women even after adjusting for hormone-receptor subtype, area-level socio-economic status, and area-level healthcare access. In addition, lower county-level socio-economic status and healthcare access measures were significantly and independently associated with stage at presentation, surgery, and radiation treatment as well as mortality after adjusting for age, race/ethnicity, and HR subtype. Although breast cancer HR subtype is a strong, important, and consistent predictor of breast cancer outcomes, we still observed significant and independent influences of area-level SES and HCA on breast cancer outcomes that deserve further study and may be critical to eliminating breast cancer outcome disparities.

Similar content being viewed by others
References
Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds) (2015) SEER cancer statistics review, 1975–2012. Vol based on Nov 2014 SEER data submission. National Cancer Institute, Bethesda
McCarthy AM, Yang J, Armstrong K (2015) Increasing disparities in breast cancer mortality from 1979 to 2010 for US black women aged 20 to 49 years. Am J Public Health 105(Suppl 3):S446–S448. doi:10.2105/AJPH.2014.302297
Aizer AA, Wilhite TJ, Chen MH, Graham PL, Choueiri TK, Hoffman KE, Martin NE, Trinh QD, Hu JC, Nguyen PL (2014) Lack of reduction in racial disparities in cancer-specific mortality over a 20-year period. Cancer 120(10):1532–1539. doi:10.1002/cncr.28617
Akinyemiju TF, Soliman AS, Johnson NJ, Altekruse SF, Welch K, Banerjee M, Schwartz K, Merajver S (2013) Individual and neighborhood socioeconomic status and healthcare resources in relation to black–white breast cancer survival disparities. J Cancer Epidemiol 2013:490472. doi:10.1155/2013/490472
Jadav S, Rajan SS, Abughosh S, Sansgiry SS (2015) The role of socioeconomic status and health care access in breast cancer screening compliance among hispanics. J Public Health Manag Pract 21(5):467–476. doi:10.1097/PHH.0000000000000235
Sheppard VB, Oppong BA, Hampton R, Snead F, Horton S, Hirpa F, Brathwaite EJ, Makambi K, Onyewu S, Boisvert M, Willey S (2015) Disparities in breast cancer surgery delay: the lingering effect of race. Ann Surg Oncol 22(9):2902–2911. doi:10.1245/s10434-015-4397-3
Akinyemiju TF, Vin-Raviv N, Chavez-Yenter D, Zhao X, Budhwani H (2015) Race/ethnicity and socio-economic differences in breast cancer surgery outcomes. Cancer Epidemiol 39(5):745–751. doi:10.1016/j.canep.2015.07.010
Tao L, Gomez SL, Keegan TH, Kurian AW, Clarke CA (2015) Breast cancer mortality in African-American and non-hispanic white women by molecular subtype and stage at diagnosis: a population-based study. Cancer Epidemiol Biomarkers Prev 24(7):1039–1045. doi:10.1158/1055-9965.EPI-15-0243
Parise CA, Caggiano V (2015) The influence of socioeconomic status on racial/ethnic disparities among the ER/PR/HER2 breast cancer subtypes. J Cancer Epidemiol 2015:813456. doi:10.1155/2015/813456
Akinyemiju T, Moore JX, Altekruse SF (2015) Breast cancer survival in African-American women by hormone receptor subtypes. Breast Cancer Res Treat. doi:10.1007/s10549-015-3528-7
Boyle P (2012) Triple-negative breast cancer: epidemiological considerations and recommendations. Ann Oncol. doi:10.1093/annonc/mds187
Edge S, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A (2011) AJCC cancer staging manual, 7th edn. American Joint Committee on Cancer, Chicago, IL
Howlader N, Altekruse SF, Li CI, Chen VW, Clarke CA, Ries LAG, Cronin KA (2014) US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst 106(5):1–8. doi:10.1093/jnci/dju055
Ihemelandu CU, Leffall LD, Dewitty RL, Naab TJ, Mezghebe HM, Makambi KH, Adams-Campbell L, Frederick WA (2007) Molecular breast cancer subtypes in premenopausal and postmenopausal African-American women: age-specific prevalence and survival. J Surg Res 143:109–118. doi:10.1016/j.jss.2007.03.085
Ihemelandu CU, Naab TJ, Mezghebe HM, Makambi KH, Siram SM, Leffall LD, DeWitty RL, Frederick WA (2008) Basal cell-like (triple-negative) breast cancer, a predictor of distant metastasis in African American women. Am J Surg 195:153–158. doi:10.1016/j.amjsurg.2007.09.033
Newman L (2014) Breast cancer disparities: high-risk breast cancer and African ancestry. Surg Oncol Clin N Am 23:579–592
Parise CA, Caggiano V (2014) Breast cancer survival defined by the ER/PR/HER2 subtypes and a surrogate classification according to tumor grade and immunohistochemical biomarkers. J Cancer Epidemiol 2014:11. doi:10.1155/2014/469251
Akinyemiju TF, Pisu M, Waterbor JW, Altekruse SF (2015) Socioeconomic status and incidence of breast cancer by hormone receptor subtype. Springer 4:508. doi:10.1186/s40064-015-1282-2
Feinglass J, Rydzewski N, Yang A (2015) The socioeconomic gradient in all-cause mortality for women with breast cancer: findings from the 1998 to 2006 national cancer data base with follow-up through 2011. Ann Epidemiol 25(8):549–555. doi:10.1016/j.annepidem.2015.02.006
Kish JK, Yu M, Percy-Laurry A (2014) Altekruse SF (2014) Racial and ethnic disparities in cancer survival by neighborhood socioeconomic status in Surveillance, Epidemiology, and End Results (SEER) registries. J Natl Cancer Inst Monogr 49:236–243. doi:10.1093/jncimonographs/lgu020
Parise CA, Caggiano V (2013) Disparities in race/ethnicity and socioeconomic status: risk of mortality of breast cancer patients in the California Cancer Registry, 2000–2010. BMC Cancer 13:449. doi:10.1186/1471-2407-13-449
Silber JH, Rosenbaum PR, Clark AS, Giantonio BJ, Ross RN, Teng Y, Wang M, Niknam BA, Ludwig JM, Wang W, Even-Shoshan O, Fox KR (2013) Characteristics associated with differences in survival among black and white women with breast cancer. JAMA 310(4):389–397. doi:10.1001/jama.2013.8272
Shariff-Marco S, Yang J, John EM, Kurian AW, Cheng I, Leung R, Koo J, Monroe KR, Henderson BE, Bernstein L, Lu Y, Kwan ML, Sposto R, Vigen CL, Wu AH, Keegan TH, Gomez SL (2015) Intersection of race/ethnicity and socioeconomic status in mortality after breast cancer. J Community Health 40(6):1287–1299. doi:10.1007/s10900-015-0052-y
Roseland ME, Pressler ME, Lamerato LE, Krajenta R, Ruterbusch JJ, Booza JC, Schwartz K, Simon MS (2015) Racial differences in breast cancer survival in a large urban integrated health system. Cancer 121(20):3668–3675. doi:10.1002/cncr.29523
Akinyemiju TF, Soliman AS, Yassine M, Banerjee M, Schwartz K, Merajver S (2012) Healthcare access and mammography screening in Michigan: a multilevel cross-sectional study. Int J Equity Health 11:16. doi:10.1186/1475-9276-11-16
Fan JX, Hanson HA, Zick CD, Brown BB, Kowaleski-Jones L, Smith KR (2014) Geographic scale matters in detecting the relationship between neighbourhood food environments and obesity risk: an analysis of driver license records in Salt Lake County, Utah. BMJ Open 4(8):e005458. doi:10.1136/bmjopen-2014-005458
Subramanian SV, Chen JT, Rehkopf DH, Waterman PD, Krieger N (2006) Comparing individual- and area-based socioeconomic measures for the surveillance of health disparities: a multilevel analysis of Massachusetts births, 1989–1991. Am J Epidemiol 164(9):823–834. doi:10.1093/aje/kwj313
Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV (2003) Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures—the public health disparities geocoding project. Am J Public Health 93(10):1655–1671
Diez Roux AV (2002) A glossary for multilevel analysis. J Epidemiol Community Health 56(8):588–594
Howlader N, Altekruse SF, Li CI, Chen VW, Clarke CA, Ries LA, Cronin KA (2014) US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst 106(5):1–8. doi:10.1093/jnci/dju055
Joslin CE, Brewer KC, Davis FG, Hoskins K, Peterson CE, Pauls HA (2014) The effect of neighborhood-level socioeconomic status on racial differences in ovarian cancer treatment in a population-based analysis in Chicago. Gynecol Oncol 135(2):285–291. doi:10.1016/j.ygyno.2014.08.029
Bristow RE, Powell MA, Al-Hammadi N, Chen L, Miller JP, Roland PY, Mutch DG, Cliby WA (2013) Disparities in ovarian cancer care quality and survival according to race and socioeconomic status. J Natl Cancer Inst 105(11):823–832. doi:10.1093/jnci/djt065
Gomez DR, Liao KP, Giordano S, Nguyen H, Smith BD, Elting LS (2013) Adherence to national guidelines for antiemesis prophylaxis in patients undergoing chemotherapy for lung cancer: a population-based study. Cancer 119(7):1428–1436. doi:10.1002/cncr.27899
Devoe JE, Baez A, Angier H, Krois L, Edlund C, Carney PA (2007) Insurance + access not equal to health care: typology of barriers to health care access for low-income families. Ann Fam Med 5(6):511–518. doi:10.1370/afm.748
Bristow RE, Chang J, Ziogas A, Campos B, Chavez LR, Anton-Culver H (2015) Sociodemographic disparities in advanced ovarian cancer survival and adherence to treatment guidelines. Obstet Gynecol 125(4):833–842. doi:10.1097/AOG.0000000000000643
Hines RB, Barrett A, Twumasi-Ankrah P, Broccoli D, Engelman KK, Baranda J, Ablah EA, Jacobson L, Redmond M, Tu W, Collins TC (2015) Predictors of guideline treatment nonadherence and the impact on survival in patients with colorectal cancer. J Natl Compr Cancer Netw 13(1):51–60
Bristow RE, Chang J, Ziogas A, Anton-Culver H, Vieira VM (2014) Spatial analysis of adherence to treatment guidelines for advanced-stage ovarian cancer and the impact of race and socioeconomic status. Gynecol Oncol 134(1):60–67. doi:10.1016/j.ygyno.2014.03.561
Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R (2002) Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter? The public health disparities geocoding project. Am J Epidemiol 156(5):471–482
Acknowledgments
Dr. Akinyemiju was supported by Grant U54 CA118948 from the NIH. Mr. Moore was supported by Grant R25 CA47888 from the National Cancer Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Akinyemiju, T., Moore, J.X., Ojesina, A.I. et al. Racial disparities in individual breast cancer outcomes by hormone-receptor subtype, area-level socio-economic status and healthcare resources. Breast Cancer Res Treat 157, 575–586 (2016). https://doi.org/10.1007/s10549-016-3840-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-016-3840-x