Abstract
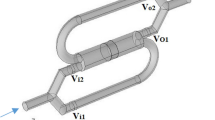
The onset of thromboembolic phenomena in blood oxygenators, even in the presence of adequate anticoagulant strategies, is a relevant concern during extracorporeal circulation (ECC). For this reason, the evaluation of the thrombogenic potential associated with extracorporeal membrane oxygenators should play a critical role into the preclinical design process of these devices. This study extends the use of computational fluid dynamics simulations to guide the hemodynamic design optimization of oxygenators and evaluate their thrombogenic potential during ECC. The computational analysis accounted for both macro- (i.e., vortex formation) and micro-scale (i.e., flow-induced platelet activation) phenomena affecting the performances of a hollow-fiber membrane oxygenator with integrated heat exchanger. A multiscale Lagrangian approach was adopted to infer the trajectory and loading history experienced by platelet-like particles in the entire device and in a repetitive subunit of the fiber bundles. The loading history was incorporated into a damage accumulation model in order to estimate the platelet activation state (PAS) associated with repeated passes of the blood within the device. Our results highlighted the presence of blood stagnation areas in the inlet section that significantly increased the platelet activation levels in particles remaining trapped in this region. The order of magnitude of PAS in the device was the same as the one calculated for the components of the ECC tubing system, chosen as a term of comparison for their extensive diffusion. Interpolating the mean PAS values with respect to the number of passes, we obtained a straightforward prediction of the thrombogenic potential as a function of the duration of ECC.
Similar content being viewed by others
Abbreviations
- BRD:
-
Blood recirculating device
- CFD:
-
Computational fluid dynamics
- DPM:
-
Discrete phase modeling
- ECC:
-
Extracorporeal circulation
- HE:
-
Heat exchanger
- OXY:
-
Oxygenator
- PAS:
-
Platelet activity state
- SA:
-
Stress accumulation
References
Alemu Y, Bluestein D (2007) Flow-induced platelet activation and damage accumulation in a mechanical heart valve: numerical studies. Artif Organs 31(9): 677–688. doi:10.1111/j.1525-1594.2007.00446.x
Alemu Y, Girdhar G, Xenos M, Sheriff J, Jesty J, Einav S, Bluestein D (2010) Design optimization of a mechanical heart valve for reducing valve thrombogenicity-A case study with ATS valve. ASAIO J 56(5): 389–396. doi:10.1097/MAT.0b013e3181e65bf9
Apel J, Paul R, Klaus S, Siess T, Reul H (2001) Assessment of hemolysis related quantities in a microaxial blood pump by computational fluid dynamics. Artif Organs 25(5): 341–347. doi:10.1046/j.1525-1594.2001.025005341.x
Ballyk PD, Steinman DA, Ethier CR (1994) Simulation of non-Newtonian blood flow in an end-to-side anastomosis. Biorheology 31(5): 565–586
Banks J, Bressloff NW (2007) Turbulence modeling in three-dimensional stenosed arterial bifurcations. J Biomech Eng 129(1): 40–50. doi:10.1115/1.2401182
Bird RB, Stewart WE, Lightfoot EN (2002) Transport Phenomena, 2nd edition. John Wiley, New York
Bluestein D (2006) Towards optimization of the thrombogenic potential of blood recirculating cardiovascular devices using modeling approaches. Expert Rev Med Devic 3(3): 267–270. doi:10.1586/17434440.3.3.267
Bluestein D, Chandran KB, Manning KB (2010) Towards non-thrombogenic performance of blood recirculating devices. Ann Biomed Eng 38(3): 1236–1256. doi:10.1007/s10439-010-9905-9
Dierickx PW, De Wachter D, Verdonck PR (2000) Blood flow around hollow fibers. Int J Artif Organs 23(9): 610–617
Dumont K, Vierendeels J, Kaminsky R, van Nooten G, Verdonck P, Bluestein D (2007) Comparison of the hemodynamic and thrombogenic performance of two bileaflet mechanical heart valves using a CFD/FSI model. J Biomech Eng 129(4): 558–565. doi:10.1115/1.2746378
Eloot S, De Wachter D, Van Tricht I, Verdonck P (2002) Computational flow modeling in hollow-fiber dialyzers. Artif Organs 26(7): 590–599. doi:10.1046/j.1525-1594.2002.07081.x
Fiore B, Soncini M, Vesentini S, Penati A, Visconti G, Redaelli A (2006) Multi-scale analysis of the toraymyxin adsorption cartridge. Part II: computational fluid-dynamic study. Int J Artif Organs 29(2): 251–260
Fiore GB, Morbiducci U, Ponzini R, Redaelli A (2009) Bubble tracking through computational fluid dynamics in arterial line filters for cardiopulmonary bypass. ASAIO J 55(5): 438–444. doi:10.1097/MAT.0b013e3181b3800c00002480-200909000-00003[pii]
Fiore GB, Pennati G, Inzoli F, Mastrantonio F, Galavotti D (1998) Effects of blood flow pulse frequency on mass transfer efficiency of a commercial hollow fibre oxygenator. Int J Artif Organs 21(9): 535–541
Fiore GB, Redaelli A, Guadagni G, Inzoli F, Fumero R (2002) Development of a new disposable pulsatile pump for cardiopulmonary bypass: computational fluid-dynamic design and in vitro tests. ASAIO J 48(3): 260–267
Gage KL, Gartner MJ, Burgreen GW, Wagner WR (2002) Predicting membrane oxygenator pressure drop using computational fluid dynamics. Artif Organs 26(7): 600–607
Gartner MJ, Wilhelm CR, Gage KL, Fabrizio MC, Wagner WR (2000) Modeling flow effects on thrombotic deposition in a membrane oxygenator. Artif Organs 24(1): 29–36
Goodman PD, Barlow ET, Crapo PM, Mohammad SF, Solen KA (2005) Computational model of device-induced thrombosis and thromboembolism. Ann Biomed Eng 33(6): 780–797
Graefe R, Borchardt R, Arens J, Schlanstein P, Schmitz-Rode T, Steinseifer U (2010) Improving oxygenator performance using computational simulation and flow field-based parameters. Artif Organs 34(11): 930–936. doi:10.1111/j.1525-1594.2010.01157.x
Haworth WS (2003) The development of the modern oxygenator. Ann Thorac Surg 76(6): S2216–S2219. doi:10.1016/j.athoracsur.2003.09.012
Hormes M, Borchardt R, Mager I, Rode TS, Behr M, Steinseifer U (2011) A validated CFD model to predict O and CO transfer within hollow fiber membrane oxygenators. Int J Artif Organs 34(3): 317–325. doi:416396B2-E82B-43ED-841D-40D440D5FB14[pii]
Idelchik IE (1994) Handbook of Hydraulic Resistance. Begell House, Boca Raton, FL
Johnston BM, Johnston PR, Corney S, Kilpatrick D (2004) Non-Newtonian blood flow in human right coronary arteries: steady state simulations. J Biomech 37(5): 709–720. doi:10.1016/j.jbiomech.2003.09.016
Kawahito S, Maeda T, Motomura T, Takano T, Nonaka K, Linneweber J, Mikami M, Ichikawa S, Kawamura M, Glueck J, Sato K, Nose Y (2001) Development of a new hollow fiber silicone membrane oxygenator: in vitro study. Artif Organs 25(6): 494–498. doi:10.1046/j.1525-1594.2001.06706-3.x
Kim J, Moin P, Moser R (1987) Turbulence statistics in fully developed channel flow at low Reynolds number. Journal of Fluid Mechanics 177: 133–166. doi:10.1017/S0022112087000892
Legendre D, Antunes P, Bock E, Andrade A, Biscegli JF, Ortiz JP (2008) Computational fluid dynamics investigation of a centrifugal blood pump. Artif Organs 32(4): 342–348. doi:10.1111/j.1525-1594.2008.00552.x
Linneweber J, Chow TW, Kawamura M, Moake JL, Nose Y (2002) In vitro comparison of blood pump induced platelet microaggregates between a centrifugal and roller pump during cardiopulmonary bypass. Int J Artif Organs 25(6): 549–555
Mellgren K, Skogby M, Jarnas A, Friberg LG, Wadenvik H, Mellgren G (1996) Platelet activation and degradation in an experimental extracorporeal system. A comparison between a silicone membrane and a hollow-fibre oxygenator. Perfusion 11(5): 383–388
Morbiducci U, Ponzini R, Nobili M, Massai D, Montevecchi FM, Bluestein D, Redaelli A (2009) Blood damage safety of prosthetic heart valves. Shear-induced platelet activation and local flow dynamics: a fluid-structure interaction approach. J Biomech 42(12): 1952–1960. doi:10.1016/j.jbiomech.2009.05.014
Mueller XM, Tevaearai HT, Augstburger M, Horisberger J, von Segesser LK (1998) Experimental evaluation of the Dideco D903 Avant 1.7 hollow-fibre membrane oxygenator. Perfusion 13(5): 353–359
Niimi Y, Ichinose F, Ishiguro Y, Terui K, Uezono S, Morita S, Yamane S (1999) The effects of heparin coating of oxygenator fibers on platelet adhesion and protein adsorption. Anesth Analg 89(3): 573–579
Nobili M, Sheriff J, Morbiducci U, Redaelli A, Bluestein D (2008) Platelet activation due to hemodynamic shear stresses: damage accumulation model and comparison to in vitro measurements. ASAIO J 54(1): 64–72. doi:10.1097/MAT.0b013e31815d689800002480-200801000-00012[pii]
Pappalardo F, Della Valle P, Crescenzi G, Corno C, Franco A, Torracca L, Alfieri O, Galli L, Zangrillo A, D’Angelo A (2006) Phosphorylcholine coating may limit thrombin formation during high-risk cardiac surgery: a randomized controlled trial. Ann Thorac Surg 81(3): 886–891. doi:10.1016/j.athoracsur.2005.09.006
Ramstack JM, Zuckerman L, Mockros LF (1979) Shear-induced activation of platelets. J Biomech 12(2): 113–125
Schaadt J (1999) Oxygenator thrombosis: an international phenomenon. Perfusion 14(6): 425–435
Sheriff J, Bluestein D, Girdhar G, Jesty J (2010) High-shear stress sensitizes platelets to subsequent low-shear conditions. Ann Biomed Eng 38(4): 1442–1450. doi:10.1007/s10439-010-9936-2
Swartz MA, Fleury ME (2007) Interstitial flow and its effects in soft tissues. Annu Rev Biomed Eng 9: 229–256. doi:10.1146/annurev.bioeng.9.060906.151850
Tanaka M, Kawahito K, Adachi H, Isawa H, Ino T (2001) Platelet damage caused by the centrifugal pump: laser-light scattering analysis of aggregation patterns. Artif Organs 25(9): 719–723
Varghese SS, Frankel SH (2003) Numerical modeling of pulsatile turbulent flow in stenotic vessels. J Biomech Eng 125(4): 445–460
Verdonck P (2002) The role of computational fluid dynamics for artificial organ design. Artif Organs 26(7): 569–570
Vesentini S, Soncini M, Zaupa A, Silvestri V, Fiore GB, Redaelli A (2006) Multi-scale analysis of the toraymyxin adsorption cartridge. Part I: molecular interaction of polymyxin B with endotoxins. Int J Artif Organs 29(2): 239–250
Xenos M, Girdhar G, Alemu Y, Jesty J, Slepian M, Einav S, Bluestein D (2010) Device Thrombogenicity Emulator (DTE)–design optimization methodology for cardiovascular devices: a study in two bileaflet MHV designs. J Biomech 43(12): 2400–2409. doi:10.1016/j.jbiomech.2010.04.020
Yamaguchi T, Ishikawa T, Imai Y, Matsuki N, Xenos M, Deng Y, Bluestein D (2010) Particle-based methods for multiscale modeling of blood flow in the circulation and in devices: challenges and future directions. Sixth International Bio-Fluid Mechanics Symposium and Workshop March 28-30, 2008 Pasadena, California. Ann Biomed Eng 38(3): 1225–1235
Zimmermann AK, Weber N, Aebert H, Ziemer G, Wendel HP (2007) Effect of biopassive and bioactive surface-coatings on the hemocompatibility of membrane oxygenators. J Biomed Mater Res B Appl Biomater 80(2): 433–439. doi:10.1002/jbm.b.30614
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pelosi, A., Sheriff, J., Stevanella, M. et al. Computational evaluation of the thrombogenic potential of a hollow-fiber oxygenator with integrated heat exchanger during extracorporeal circulation. Biomech Model Mechanobiol 13, 349–361 (2014). https://doi.org/10.1007/s10237-012-0445-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10237-012-0445-0