Abstract
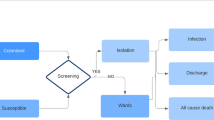
The purpose of this study was to assess the cost-effectiveness of screening all hospital inpatients for carbapenemase-producing Enterobacteriaceae (CPE) at the time of hospital admission, compared to not screening, from a US hospital perspective. We used a linked transmission/Markov model to compare outcomes for a typical hospitalized medical patient, from a community with a colonization prevalence of 0.05%. Outcomes were number of colonized patients, CPE-related clinical infections and deaths, expected quality-adjusted life years (QALYs), cost, and the incremental cost-effectiveness ratio (ICER). Sensitivity analyses were performed to assess the effect of parameter uncertainty, using a willingness-to-pay threshold of $100,000 per QALY gained. Screening prevented six CPE colonization cases per 1000 patients (1/1000 colonized with screening, 7/1000 without screening), over half of all symptomatic CPE infections (2/10,000 symptomatic with screening, 5/10,000 symptomatic without screening), and nearly half of all CPE-related deaths (8/100,000 deaths with screening, 15/100,000 deaths without screening). Screening accrued 0.0009 additional QALYs and cost an additional $24.68, compared to not screening, and was cost-effective (ICER $26,283 per QALY gained). Our results were sensitive to uncertainty in prevalence and the number of secondary colonizations per colonized patient. Screening was not cost-effective at a prevalence below 0.015% or if transmission to fewer than 0.9 new patients occurred for each colonized patient. At prevalence levels above 0.3%, screening was cost-saving compared to not screening. Screening inpatients for CPE carriage is likely cost-effective, and may be cost-saving, depending on the local prevalence of carriage.




Similar content being viewed by others
References
Siegel JD, Rhinehart E, Jackson M, Chiarello L; the Healthcare Infection Control Practices Advisory Committee (2007) Part III: precautions to prevent transmission of infectious agents. In: Centers for Disease Control and Prevention (ed) 2007 guideline for isolation precautions: preventing transmission of infectious agents in healthcare settings. CDC, Atlanta, Georgia
National Health Service (NHS) (2006) Screening for meticillin-resistant Staphylococcus aureus (MRSA) colonisation: a strategy for NHS trusts: a summary of best practice
Schechner V, Kotlovsky T, Kazma M, Mishali H, Schwartz D, Navon-Venezia S, Schwaber MJ, Carmeli Y (2013) Asymptomatic rectal carriage of blaKPC producing carbapenem-resistant Enterobacteriaceae: who is prone to become clinically infected? Clin Microbiol Infect 19(5):451–456
Nordmann P, Dortet L, Poirel L (2012) Carbapenem resistance in Enterobacteriaceae: here is the storm! Trends Mol Med 18(5):263–272
Falagas ME, Tansarli GS, Karageorgopoulos DE, Vardakas KZ (2014) Deaths attributable to carbapenem-resistant Enterobacteriaceae infections. Emerg Infect Dis 20(7):1170–1175
Calfee D, Jenkins SG (2008) Use of active surveillance cultures to detect asymptomatic colonization with carbapenem-resistant Klebsiella pneumoniae in intensive care unit patients. Infect Control Hosp Epidemiol 29(10):966–968
Kochar S, Sheard T, Sharma R, Hui A, Tolentino E, Allen G, Landman D, Bratu S, Augenbraun M, Quale J (2009) Success of an infection control program to reduce the spread of carbapenem-resistant Klebsiella pneumoniae. Infect Control Hosp Epidemiol 30(5):447–452
Hirakata Y, Izumikawa K, Yamaguchi T, Takemura H, Tanaka H, Yoshida R, Matsuda J, Nakano M, Tomono K, Maesaki S, Kaku M, Yamada Y, Kamihira S, Kohno S (1998) Rapid detection and evaluation of clinical characteristics of emerging multiple-drug-resistant gram-negative rods carrying the metallo-beta-lactamase gene blaIMP. Antimicrob Agents Chemother 42(8):2006–2011
Peleg AY, Franklin C, Bell JM, Spelman DW (2005) Dissemination of the metallo-beta-lactamase gene blaIMP-4 among gram-negative pathogens in a clinical setting in Australia. Clin Infect Dis 41(11):1549–1556
Landman D, Babu E, Shah N, Kelly P, Olawole O, Bäcker M, Bratu S, Quale J (2012) Transmission of carbapenem-resistant pathogens in New York City hospitals: progress and frustration. J Antimicrob Chemother 67(6):1427–1431
Chitnis AS, Caruthers PS, Rao AK, Lamb J, Lurvey R, Beau De Rochars V, Kitchel B, Cancio M, Török TJ, Guh AY, Gould CV, Wise ME (2012) Outbreak of carbapenem-resistant enterobacteriaceae at a long-term acute care hospital: sustained reductions in transmission through active surveillance and targeted interventions. Infect Control Hosp Epidemiol 33(10):984–992
Ho KW, Ng WT, Ip M, You JHS (2016) Active surveillance of carbapenem-resistant Enterobacteriaceae in intensive care units: is it cost-effective in a nonendemic region? Am J Infect Control 44(4):394–399
World Health Organization (WHO) (2005) Threshold values for intervention cost-effectiveness by region. Cost effectiveness and strategic planning (WHO-CHOICE)
The World Bank (2014) GDP per capita (current US$). Available online at: http://data.worldbank.org/indicator/NY.GDP.PCAP.CD
Swaminathan M, Sharma S, Poliansky Blash S, Patel G, Banach DB, Phillips M, LaBombardi V, Anderson KF, Kitchel B, Srinivasan A, Calfee DP (2013) Prevalence and risk factors for acquisition of carbapenem-resistant Enterobacteriaceae in the setting of endemicity. Infect Control Hosp Epidemiol 34(8):809–817
Social Security Administration (2015) Calculators: life expectancy. Available online at: https://www.ssa.gov/planners/lifeexpectancy.html. Cited March 10, 2015
Gold MR, Siegel JE, Russell LB, Weinstein MC (1996) Cost-effectiveness in health and medicine. Oxford University Press, Oxford
Abbey H (1952) An examination of the Reed–Frost theory of epidemics. Hum Biol 24(3):201–233
Sypsa V, Psichogiou M, Bouzala G-A, Hadjihannas L, Hatzakis A, Daikos GL (2012) Transmission dynamics of carbapenemase-producing Klebsiella pneumoniae and anticipated impact of infection control strategies in a surgical unit. PLoS One 7(7), e41068
Zimmerman FS, Assous MV, Bdolah-Abram T, Lachish T, Yinnon AM, Wiener-Well Y (2013) Duration of carriage of carbapenem-resistant Enterobacteriaceae following hospital discharge. Am J Infect Control 41(3):190–194
Guh AY, Bulens SN, Mu Y, Jacob JT, Reno J, Scott J, Wilson LE, Vaeth E, Lynfield R, Shaw KM, Vagnone PM, Bamberg WM, Janelle SJ, Dumyati G, Concannon C, Beldavs Z, Cunningham M, Cassidy PM, Phipps EC, Kenslow N, Travis T, Lonsway D, Rasheed JK, Limbago BM, Kallen AJ (2015) Epidemiology of carbapenem-resistant Enterobacteriaceae in 7 US Communities, 2012–2013. JAMA 314(14):1479–1487
Pournaras S, Zarkotou O, Poulou A, Kristo I, Vrioni G, Themeli-Digalaki K, Tsakris A (2013) A combined disk test for direct differentiation of carbapenemase-producing enterobacteriaceae in surveillance rectal swabs. J Clin Microbiol 51(9):2986–2990
Schechner V, Straus-Robinson K, Schwartz D, Pfeffer I, Tarabeia J, Moskovich R, Chmelnitsky I, Schwaber MJ, Carmeli Y, Navon-Venezia S (2009) Evaluation of PCR-based testing for surveillance of KPC-producing carbapenem-resistant members of the Enterobacteriaceae family. J Clin Microbiol 47(10):3261–3265
Lautenbach E, Harris AD, Perencevich EN, Nachamkin I, Tolomeo P, Metlay JP (2005) Test characteristics of perirectal and rectal swab compared to stool sample for detection of fluoroquinolone-resistant Escherichia coli in the gastrointestinal tract. Antimicrob Agents Chemother 49(2):798–800
Jernigan JA, Titus MG, Gröschel DH, Getchell-White S, Farr BM (1996) Effectiveness of contact isolation during a hospital outbreak of methicillin-resistant Staphylococcus aureus. Am J Epidemiol 143(5):496–504
Geffers C, Farr BM (2005) Risk of transmission of nosocomial methicillin-resistant Staphylococcus aureus (MRSA) from patients colonized with MRSA. Infect Control Hosp Epidemiol 26(2):114–115
Ben-David D, Masarwa S, Adler A, Mishali H, Carmeli Y, Schwaber MJ (2014) A national intervention to prevent the spread of carbapenem-resistant Enterobacteriaceae in Israeli post-acute care hospitals. Infect Control Hosp Epidemiol 35(7):802–809
Mittmann N, Trakas K, Risebrough N, Liu BA (1999) Utility scores for chronic conditions in a community-dwelling population. Pharmacoeconomics 15(4):369–376
Selai C, Rosser R (1995) Eliciting EuroQol descriptive data and utility scale values from inpatients. A feasibility study. Pharmacoeconomics 8:147–158
Tengs TO, Wallace A (2000) One thousand health-related quality-of-life estimates. Med Care 38(6):583–637
Mathers AJ, Poulter M, Dirks D, Carroll J, Sifri CD, Hazen KC (2014) Clinical microbiology costs for methods of active surveillance for Klebsiella pneumoniae carbapenemase-producing Enterobacteriaceae. Infect Control Hosp Epidemiol 35(4):350–355
Warren DK, Quadir WW, Hollenbeak CS, Elward AM, Cox MJ, Fraser VJ (2006) Attributable cost of catheter-associated bloodstream infections among intensive care patients in a nonteaching hospital. Crit Care Med 34(8):2084–2089
Roberts RR, Scott RD 2nd, Hota B, Kampe LM, Abbasi F, Schabowski S, Ahmad I, Ciavarella GG, Cordell R, Solomon SL, Hagtvedt R, Weinstein RA (2010) Costs attributable to healthcare-acquired infection in hospitalized adults and a comparison of economic methods. Med Care 48(11):1026–1035
Roberts RR, Hota B, Ahmad I, Scott RD 2nd, Foster SD, Abbasi F, Schabowski S, Kampe LM, Ciavarella GG, Supino M, Naples J, Cordell R, Levy SB, Weinstein RA (2009) Hospital and societal costs of antimicrobial-resistant infections in a Chicago teaching hospital: implications for antibiotic stewardship. Clin Infect Dis 49(8):1175–1184
United States Department of Labor (2015) Consumer price index inflation database. Bureau of Labor Statistics. Available online at: http://www.bls.gov/data/inflation_calculator.htm
Schwaber MJ, Carmeli Y (2014) An ongoing national intervention to contain the spread of carbapenem-resistant enterobacteriaceae. Clin Infect Dis 58(5):697–703
Wiener-Well Y, Rudensky B, Yinnon AM, Kopuit P, Schlesinger Y, Broide E, Lachish T, Raveh D (2010) Carriage rate of carbapenem-resistant Klebsiella pneumoniae in hospitalised patients during a national outbreak. J Hosp Infect 74(4):344–349
Kaase M, Szabados F, Wassill L, Gatermann SG (2012) Detection of carbapenemases in Enterobacteriaceae by a commercial multiplex PCR. J Clin Microbiol 50(9):3115–3118
Borer A, Saidel-Odes L, Riesenberg K, Eskira S, Peled N, Nativ R, Schlaeffer F, Sherf M (2009) Attributable mortality rate for carbapenem-resistant Klebsiella pneumoniae bacteremia. Infect Control Hosp Epidemiol 30(10):972–976
Qureshi ZA, Paterson DL, Potoski BA, Kilayko MC, Sandovsky G, Sordillo E, Polsky B, Adams-Haduch JM, Doi Y (2012) Treatment outcome of bacteremia due to KPC-producing Klebsiella pneumoniae: superiority of combination antimicrobial regimens. Antimicrob Agents Chemother 56(4):2108–2113
Tumbarello M, Viale P, Viscoli C, Trecarichi EM, Tumietto F, Marchese A, Spanu T, Ambretti S, Ginocchio F, Cristini F, Losito AR, Tedeschi S, Cauda R, Bassetti M (2012) Predictors of mortality in bloodstream infections caused by Klebsiella pneumoniae carbapenemase-producing K. pneumoniae: importance of combination therapy. Clin Infect Dis 55(7):943–950
Baker ST, Chiang CY, Zajac JD, Bach LA, Jerums G, MacIsaac RJ (2008) Outcomes for general medical inpatients with diabetes mellitus and new hyperglycaemia. Med J Aust 188(6):340–343
Halkin H, Goldberg J, Modan M, Modan B (1982) Reduction of mortality in general medical in-patients by low-dose heparin prophylaxis. Ann Intern Med 96(5):561–565
Beusterien KM, Davies J, Leach M, Meiklejohn D, Grinspan JL, O’Toole A, Bramham-Jones S (2010) Population preference values for treatment outcomes in chronic lymphocytic leukaemia: a cross-sectional utility study. Health Qual Life Outcomes 8:50
Coley CM, Li YH, Medsger AR, Marrie TJ, Fine MJ, Kapoor WN, Lave JR, Detsky AS, Weinstein MC, Singer DE (1996) Preferences for home vs hospital care among low-risk patients with community-acquired pneumonia. Arch Intern Med 156(14):1565–1571
Weeks JC, Tierney MR, Weinstein MC (1991) Cost effectiveness of prophylactic intravenous immune globulin in chronic lymphocytic leukemia. N Engl J Med 325(2):81–86
Lee BY, Bailey RR, Smith KJ, Muder RR, Strotmeyer ES, Lewis GJ, Ufberg PJ, Song Y, Harrison LH (2010) Universal methicillin-resistant Staphylococcus aureus (MRSA) surveillance for adults at hospital admission: an economic model and analysis. Infect Control Hosp Epidemiol 31(6):598–606
Verlee K, Berriel-Cass D, Buck K, Nguyen C (2014) Cost of isolation: daily cost of isolation determined and cost avoidance demonstrated from the overuse of personal protective equipment in an acute care facility. Am J Infect Control 42(4):448–449
Spiegelhalter DJ, Abrams KR, Myles JP (2004) Bayesian approaches to clinical trials and health-care evaluation. Wiley, Chichester, p xiv, 391 pp
Public Health England (2013) Acute trust toolkit for the early detection, management and control of carbapenemase-producing Enterobacteriaceae. London, England. Available online at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/329227/Acute_trust_toolkit_for_the_early_detection.pdf
Grundmann H, Livermore DM, Giske CG, Canton R, Rossolini GM, Campos J, Vatopoulos A, Gniadkowski M, Toth A, Pfeifer Y, Jarlier V, Carmeli Y; CNSE Working Group (2010) Carbapenem-non-susceptible Enterobacteriaceae in Europe: conclusions from a meeting of national experts. Euro Surveill 15(46). pii: 19711
Ontario Agency for Health Protection and Promotion (Public Health Ontario) (2013) Screening, testing and surveillance for antibiotic-resistant organisms (AROs). Queen’s Printer for Ontario, Toronto
Fleming C, McGeer A (2013) Antimicrobial resistance in common hospital pathogens in Ontario. Institute for Quality Management in Healthcare, Toronto
Cooper BS, Medley GF, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Duckworth G, Lai R, Ebrahim S (2004) Methicillin-resistant Staphylococcus aureus in hospitals and the community: stealth dynamics and control catastrophes. Proc Natl Acad Sci U S A 101(27):10223–10228
Spapen H, Jacobs R, Van Gorp V, Troubleyn J, Honoré PM (2011) Renal and neurological side effects of colistin in critically ill patients. Ann Intensive Care 1(1):14
Modi N, Maggs AF, Clarke C, Chapman C, Swann RA (1998) Gentamicin concentration and toxicity. Lancet 352(9121):70–71
Cheng A, Chuang YC, Sun HY, Sheng WH, Yang CJ, Liao CH, Hsueh PR, Yang JL, Shen NJ, Wang JT, Hung CC, Chen YC, Chang SC (2015) Excess mortality associated with colistin-tigecycline compared with colistin–carbapenem combination therapy for extensively drug-resistant Acinetobacter baumannii bacteremia: a multicenter prospective observational study. Crit Care Med 43(6):1194–1204
Acknowledgments
We thank David Naimark, MD MSc for the technical assistance with TreeAge during the model development.
Contributions
LL-S and TV are joint first authors, having contributed equally. Study concept and design: LL-S, TV, PK, H-HT, BS, AM. Analysis and interpretation of data: LL-S, TV. Drafting of the manuscript: LL-S, TV. Critical revision of the manuscript for important intellectual content: LL-S, TV, PK, H-HT, BS, AM. Statistical analysis: LL-S, TV.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work did not receive any funding.
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
The data used in this study are from the published literature; thus, no ethical approval was sought.
Informed consent
No unpublished patient-level data were used in this study; thus, there was no need for informed consent.
Additional information
L. Lapointe-Shaw and T. Voruganti contributed equally to this work.
Rights and permissions
About this article
Cite this article
Lapointe-Shaw, L., Voruganti, T., Kohler, P. et al. Cost-effectiveness analysis of universal screening for carbapenemase-producing Enterobacteriaceae in hospital inpatients. Eur J Clin Microbiol Infect Dis 36, 1047–1055 (2017). https://doi.org/10.1007/s10096-016-2890-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-016-2890-7