Abstract
Background
This paper is addressing outcome differences in interesting subgroups from a previous randomized controlled trial of the extent of mesial temporal lobe resection (TLR) for drug-resistant epilepsy, by looking at effects of randomization, intended resection group, center, and true resection extent on seizure outcome.
Methods
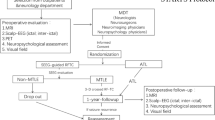
One hundred and seventy-nine cases with volumetrically assessed resection extent were used. Analyses of the extent of resection and subgroups and within subgroups for the two treatment arms will be performed, looking for confounding factors and using statistical methods (chi-square test, logistic regression analysis, and two-factorial ANOVA).
Results
True resection extent varied considerably. Outcome comparison for right versus left resections, subgroups with mesial temporal sclerosis (MTS), or largest and smallest resections revealed no remarkable difference, compared to overall class I outcome. The intent-to-treat analyses within these subgroups revealed differences for class I outcome, albeit lacking in significance, except for better TLR outcome. Small true resection volume differences or randomization into the two resection groups could not explain the outcome differences between the selective amygdalohippocampectomy (SAH) and TLR subgroups. Logistic regression analysis showed an interaction between intended resection length and surgery type, confirming the impression of different impacts of the intended resection length under the two surgery types. The outcome difference between SAH and TLR was more likely explained by a center effect. In a two-factorial ANOVA for resected hippocampal volume, Engel outcome class I, and resection type, the outcome was not found to be correlated with true resection volume. A multifactorial logistic regression showed a mild interaction between the resection type with center on the Engel outcome class, extent of resection, and surgery type interacted, as did the extent of resection and center.
Conclusion
Patients with quite similar extent of resection can be seizure free or non-seizure free. In this cohort, seizure freedom rates fell again when the extent of mesial resection was maximized. Differences in class I outcome for SAH and TLR were not due to erroneous randomization, true resection extent, or presence of MTS, but were influenced by a center effect. Subgroup analyses did not help to provide arguments to favor one surgery type over the other.



Similar content being viewed by others
References
Awad IA, Katz A, Hahn JF, Kong AK, Ahl J, Luders H (1989) Extent of resection in temporal lobectomy for epilepsy. I. Interobserver analysis and correlation with seizure outcome. Epilepsia 30:756–762
Jack CR Jr, Sharbrough FW, Marsh WR (1988) Use of MR imaging for quantitative evaluation of resection for temporal lobe epilepsy. Radiology 169:463–468
Jones-Gotman M, Zatorre RJ, Olivier A, Andermann F, Cendes F, Staunton H, McMackin D, Siegel AM, Wieser HG (1997) Learning and retention of words and designs following excision from medial or lateral temporal-lobe structures. Neuropsychologia 35:963–973
Mueller CA, Scorzin J, Koenig R, Urbach H, Fimmers R, Zentner J, Lehmann TN, Schramm J (2007) Comparison of manual tracing versus a semiautomatic radial measurement method in temporal lobe MRI volumetry for pharmacoresistant epilepsy. Neuroradiology 49:189–201. doi:10.1007/s00234-006-0171-3
Nayel MH, Awad IA, Luders H (1991) Extent of mesiobasal resection determines outcome after temporal lobectomy for intractable complex partial seizures. Neurosurgery 29:55–60, discussion 60-51
Novak K, Czech T, Prayer D, Dietrich W, Serles W, Lehr S, Baumgartner C (2002) Individual variations in the sulcal anatomy of the basal temporal lobe and its relevance for epilepsy surgery: an anatomical study performed using magnetic resonance imaging. J Neurosurg 96:464–473
O'Neill RT (1997) Secondary endpoints cannot be validly analyzed if the primary endpoint does not demonstrate clear statistical significance. Control Clin Trials 18:550–556
Schramm J (2008) Temporal lobe epilepsy surgery and the quest for optimal extent of resection: a review. Epilepsia 49:1296–1307
Schramm J, Lehmann TN, Zentner J, Mueller CA, Scorzin J, Fimmers R, Meencke HJ, Schulze-Bonhage A, C.E. Elger (2010) Randomized controlled trial of 2.5 versus 3.5 cm mesial temporal resection in temporal lobe epilepsy. Part 1: intent-to-treat-analysis. Acta Neurochirurgica (in press)
Siegel AM, Wieser HG, Wichmann W, Yasargil GM (1990) Relationships between MR-imaged total amount of tissue removed, resection scores of specific mediobasal limbic subcompartments and clinical outcome following selective amygdalohippocampectomy. Epilepsy Res 6:56–65
Urbach H, Hattingen J, von Oertzen J, Luyken C, Clusmann H, Kral T, Kurthen M, Schramm J, Blumcke I, Schild HH (2004) MR imaging in the presurgical workup of patients with drug-resistant epilepsy. AJNR Am J Neuroradiol 25:919–926
Vajkoczy P, Krakow K, Stodieck S, Pohlmann-Eden B, Schmiedek P (1998) Modified approach for the selective treatment of temporal lobe epilepsy: transsylvian-transcisternal mesial en bloc resection. J Neurosurg 88:855–862
Wyler AR, Hermann BP, Somes G (1995) Extent of medial temporal resection on outcome from anterior temporal lobectomy: a randomized prospective study. Neurosurgery 37:982–990, discussion 990–981
Acknowledgements
This study was funded as part of the transregional collaborative research consortium SFB-TR3 “Mesial temporal lobe epilepsies” of the Deutsche Forschungsgemeinschaft (DFG). The authors thank H. Urbach M.D. and R. Koenig M.D. (Department of Neuroradiology, University Clinic, Bonn) as well as Bluemcke M.D. (Department of Neuropathology, University Clinic, Erlangen) for help with MRI volumetry and reference pathology. Additional thanks go to other members of the study group: S. Roeske, S. Kaaden, C. Scheiwe, M.D., B. Harzheim, P. Süßmann, S. Ferl, D. and Meinken-Jäggi for organizational and volumetric support. K. Wagner, C. Helmstaedter PhD, S. Kaaden, S. Roeske, and F. Oltmanns helped with neuropsychological assessment, B.J. Steinhoff M.D., M. Merschhemke M.D., C. Dehnicke M.D., and C. Bien, M.D. helped with presurgical evaluation. D. Haun PhD helped with statistics and graphs.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schramm, J., Lehmann, T.N., Zentner, J. et al. Randomized controlled trial of 2.5-cm versus 3.5-cm mesial temporal resection—part 2: volumetric resection extent and subgroup analyses. Acta Neurochir 153, 221–228 (2011). https://doi.org/10.1007/s00701-010-0901-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-010-0901-5