Abstract
Aims
Previous studies showed that serum 1,5-anhydroglucitol (1,5-AG) levels are significantly reduced in patients with diabetes mellitus (DM). However, it remains unclear how 1,5-AG levels acutely change in response to a glucose load. This study explored acute changes in 1,5-AG levels after a glucose load and the related influencing factors in individuals with differing degrees of glucose tolerance.
Methods
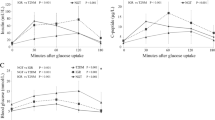
A total of 681 participants (353 without DM and 328 with DM) without a prior history of DM were enrolled. All participants underwent an oral glucose tolerance test. Fasting and postload (30, 60, 120, and 180 min) levels of plasma glucose, serum 1,5-AG, and insulin were measured.
Results
In all participant groups, serum 1,5-AG levels were slightly elevated after a glucose load and reached peak values at 120 min after loading (all P < 0.05). Regression analysis showed that body weight was negatively associated with the difference between peak and baseline 1,5-AG levels (Δ1,5-AG, standardized β = −0.119, P < 0.01). A strong and positive association between 1,5-AG0 and Δ1,5-AG was also found independent of other confounding factors (standardized β = 0.376, P < 0.01). The ratio of the Δ1,5-AG to the 1,5-AG0 was higher in DM patients (7.3% [3.4–11.5%]) than in those without DM (6.2% [3.6–9.2%]).
Conclusions
In contrast to the established decline in 1,5-AG levels with long-term hyperglycemia, the present study showed that serum 1,5-AG levels slightly increased by 6–7% after a glucose load. Further studies in different 1,5-AG transport models are needed to investigate the relevant metabolic pathways.


Similar content being viewed by others
References
Koga M (2014) 1,5-Anhydroglucitol and glycated albumin in glycemia. Adv Clin Chem 64:269–301
Ma X, Hao Y, Hu X et al (2015) 1,5-anhydroglucitol is associated with early-phase insulin secretion in chinese patients with newly diagnosed type 2 diabetes mellitus. Diabetes Technol Ther 17(5):320–326
McGill JB, Cole TG, Nowatzke W et al (2004) Circulating 1,5-anhydroglucitol levels in adult patients with diabetes reflect longitudinal changes of glycemia: a U.S. trial of the GlycoMark assay. Diabetes Care 27(8):1859–1865
Nerby CL, Stickle DF (2009) 1,5-anhydroglucitol monitoring in diabetes: a mass balance perspective. Clin Biochem 42(3):158–167
Stettler C, Stahl M, Allemann S et al (2008) Association of 1,5-anhydroglucitol and 2-h postprandial blood glucose in type 2 diabetic patients. Diabetes Care 31(8):1534–1535
Dungan KM, Buse JB, Largay J et al (2006) 1,5-anhydroglucitol and postprandial hyperglycemia as measured by continuous glucose monitoring system in moderately controlled patients with diabetes. Diabetes Care 29(6):1214–1219
Kim MJ, Jung HS, Hwang-Bo Y et al (2013) Evaluation of 1,5-anhydroglucitol as a marker for glycemic variability in patients with type 2 diabetes mellitus. Acta Diabetol 50(4):505–510
Kim WJ, Park CY (2013) 1,5-Anhydroglucitol in diabetes mellitus. Endocrine 43(1):33–40
Yamanouchi T, Shinohara T, Ogata N, Tachibana Y, Akaoka I, Miyashita H (1996) Common reabsorption system of 1,5-anhydro-d-glucitol, fructose, and mannose in rat renal tubule. Biochim Biophys Acta 1291(1):89–95
Akanuma Y, Morita M, Fukuzawa N, Yamanouchi T, Akanuma H (1988) Urinary excretion of 1,5-anhydro-d-glucitol accompanying glucose excretion in diabetic patients. Diabetologia 31(11):831–835
Goto M, Yamamoto-Honda R, Shimbo T et al (2011) Correlation between baseline serum 1,5-anhydroglucitol levels and 2-h post-challenge glucose levels during oral glucose tolerance tests. Endocr J 58(1):13–17
Department of Noncommunicable Disease Surveillance (1999) Report of a WHO Consultation: definition, diagnosis and classification of diabetes mellitus and its complication: Part1: diagnosis and classification of diabetes mellitus. World Health Organization, Geneva
World Health Organization (2000) Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894:1–253
Nowak N, Skupien J, Cyganek K, Matejko B, Malecki MT (2013) 1,5-Anhydroglucitol as a marker of maternal glycaemic control and predictor of neonatal birthweight in pregnancies complicated by type 1 diabetes mellitus. Diabetologia 56(4):709–713
Wang Y, Yuan Y, Zhang Y et al (2016) Serum 1,5-anhydroglucitol level as a screening tool for diabetes mellitus in a community-based population at high risk of diabetes. Acta Diabetol Nov 28 [Epub ahead of print]
Sun J, Dou JT, Wang XL et al (2011) Correlation between 1,5-anhydroglucitol and glycemic excursions in type 2 diabetic patients. Chin Med J (Engl) 124(22):3641–3645
Pramodkumar TA, Jayashri R, Gokulakrishnan K et al (2016) Relationship of glycemic control markers—1,5 anhydroglucitol, fructosamine, and glycated hemoglobin among Asian Indians with different degrees of glucose intolerance. Indian J Endocrinol Metab 20(5):690–695
Ma X, Hu X, Zhou J et al (2015) Glycated albumin is more closely correlated with coronary artery disease than 1,5-anhydroglucitol and glycated hemoglobin A1c. Cardiovasc Diabetol 14:16
Selvin E, Rawlings A, Lutsey P et al (2016) Association of 1,5-Anhydroglucitol with cardiovascular disease and mortality. Diabetes 65(1):201–208
Kim WJ, Park CY, Park SE et al (2012) Serum 1,5-anhydroglucitol is associated with diabetic retinopathy in Type 2 diabetes. Diabet Med 29(9):1184–1190
Watanabe M, Kokubo Y, Higashiyama A, Ono Y, Miyamoto Y, Okamura T (2011) Serum 1,5-anhydro-d-glucitol levels predict first-ever cardiovascular disease: an 11-year population-based cohort study in Japan, the Suita study. Atherosclerosis 216(2):477–483
Ikeda N, Hara H, Hiroi Y (2015) Ability of 1,5-anhydro-d-glucitol values to predict coronary artery disease in a non-diabetic population. Int Heart J 56(6):587–591
Ikeda N, Hara H, Hiroi Y (2014) 1,5-Anhydro-d-glucitol predicts coronary artery disease prevalence and complexity. J Cardiol 64(4):297–301
Fujiwara T, Yoshida M, Yamada H et al (2015) Lower 1,5-anhydroglucitol is associated with denovo coronary artery disease in patients at high cardiovascular risk. Heart Vessels 30(4):469–476
Takahashi S, Shimada K, Miyauchi K et al (2016) Low and exacerbated levels of 1,5-anhydroglucitol are associated with cardiovascular events in patients after first-time elective percutaneous coronary intervention. Cardiovasc Diabetol 15(1):145
Kato A, Kunimatsu T, Yamashita Y, Adachi I, Takeshita K, Ishikawa F (2013) Protective effects of dietary 1,5-anhydro-d-glucitol as a blood glucose regulator in diabetes and metabolic syndrome. J Agric Food Chem 61(3):611–617
Yamanouchi T, Inoue T, Ichiyanagi K, Sakai T, Ogata N (2003) 1,5-Anhydroglucitol stimulates insulin release in insulinoma cell lines. Biochim Biophys Acta 1623(2–3):82–87
Stickle D, Turk J (1997) A kinetic mass balance model for 1,5-anhydroglucitol: applications to monitoring of glycemic control. Am J Physiol 273(4 Pt 1):E821–E830
Yamanouchi T, Akaoka I, Akanuma Y, Akanuma H, Miyashita E (1990) Mechanism for acute reduction of 1,5-anhydroglucitol in rats treated with diabetogenic agents. Am J Physiol 258(3 Pt 1):E423–E427
Yamanouchi T, Akanuma H, Takaku F, Akanuma Y (1986) Marked depletion of plasma 1,5-anhydroglucitol, a major polyol, in streptozocin-induced diabetes in rats and the effect of insulin treatment. Diabetes 35(2):204–209
Acknowledgements
This work was funded by the Shanghai Municipal Science and Technology Commission Medical Guide Project (15411963500), the Natural Science Foundation of Xinjiang Uygur Autonomous Region of China (2016D01C084), and the Shanghai Municipal Education Commission—Gaofeng Clinical Medicine Grant Support (20161430).
Author contribution
J.Z. and W.J. designed the study. X.M., H.S., and X.H. collected data. H.S. analyzed data and wrote the draft. X.M., J.Y., and Y.W. provided technical support. J.Z., Y.B., and W.J. revised the paper and contributed to the discussion. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have nothing to disclose.
Ethical disclosure
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethics Committee of Shanghai Jiao Tong University Affiliated Sixth People's Hospital and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and animal rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Managed by Massimo Federici.
Hang Su, Xiaojing Ma and Jun Yin have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Su, H., Ma, X., Yin, J. et al. Serum 1,5-anhydroglucitol levels slightly increase rather than decrease after a glucose load in subjects with different glucose tolerance status. Acta Diabetol 54, 463–470 (2017). https://doi.org/10.1007/s00592-017-0968-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-017-0968-z