Abstract
Purpose
Cross-sectional research suggests that thinking about multiple ways to reach goals (hope pathways) and the belief that one can reach them (hope agency) may be adaptive for lung cancer patients. We examined the between-person and within-person associations among aspects of hope agency and pathways thinking, daily fatigue, pain, and functional concerns (e.g., sense of independence, usefulness) among lung cancer patients during active treatment.
Methods
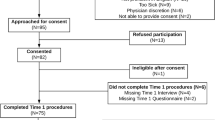
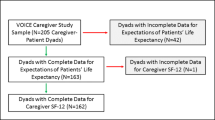
Data from a daily diary study were used to examine relations among hope agency, hope pathways, fatigue, pain, and functional concern in 50 patients with advanced lung cancer. Participants were accrued from one outpatient cancer center and completed the study between 2014 and 2015.
Results
Adjusting for covariates and the previous day’s symptoms or concern, patients who engaged in higher pathways thinking reported lower daily symptoms, whereas those who engaged in higher agency thinking reported less functional concern. Within-person increases in pathways thinking were associated with less daily fatigue, pain, and functional concern; within-person increases in agency thinking were associated with less daily fatigue and pain. Models examining symptoms and concerns as predictors of hope suggested within-person increases in functional concern and fatigue and pain were related to lower agency and pathways thinking the same day. Patients with higher fatigue and pain did not report lower agency or pathways thinking, but patients with more functional concern did.
Conclusions
Increases in hope pathways thinking may be associated with lower symptoms and better functioning in lung cancer patients. This suggests that it is important to determine the efficacy of interventions that emphasize the pathways the component of hope.
Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics, 2018. CA 68(1):7–30. https://doi.org/10.3322/caac.21442
Sung MR, Patel MV, Djalalov S, Le LW, Shepherd FA, Burkes RL, Feld R, Lin S, Tudor R, Leighl NB (2017) Evolution of symptom burden of advanced lung cancer over a decade. Clin Lung Cancer 18(3):274–280 e276. https://doi.org/10.1016/j.cllc.2016.12.010
Molassiotis A, Uyterlinde W, Hollen PJ, Sarna L, Palmer P, Krishnasamy M (2015) Supportive care in lung cancer: milestones over the past 40 years. JTO 10(1):10–18. https://doi.org/10.1097/JTO.0000000000000407
Cooley ME, Short TH, Moriarty HJ (2003) Symptom prevalence, distress, and change over time in adults receiving treatment for lung cancer. Psycho-oncology 12(7):694–708. https://doi.org/10.1002/pon.694
Given CW, Given B, Azzouz F, Kozachik S (2001) Stommel M predictors of pain and fatigue in the year following diagnosis among elderly cancer patients. JPSM 21(6):456–466. https://doi.org/10.1016/S0885-3924(01)00284-6
Brown J, Thorpe H, Napp V, Fairlamb DJ, Gower NH, Milroy R, Parmar MK, Rudd RM, Spiro SG, Stephens RJ, Waller D, West P, Peake MD (2005) Assessment of quality of life in the supportive care setting of the big lung trial in non-small-cell lung cancer. JCO 23(30):7417–7427. https://doi.org/10.1200/jco.2005.09.158
Kober KM, Cooper BA, Paul SM, Dunn LB, Levine JD, Wright F, Hammer MJ, Mastick J, Venook A, Aouizerat BE, Miaskowski C (2016) Subgroups of chemotherapy patients with distinct morning and evening fatigue trajectories. Support Care Cancer 24(4):1473–1485. https://doi.org/10.1007/s00520-015-2895-2
McCaffrey N, Bradley S, Ratcliffe J, Currow DC What aspects of quality of life are important from palliative care patients’ perspectives? A systematic review of qualitative research. JPSM 52(2):318–328.e315. https://doi.org/10.1016/j.jpainsymman.2016.02.012
Maguire R, Papadopoulou C, Kotronoulas G, Simpson MF, McPhelim J, Irvine L (2013) A systematic review of supportive care needs of people living with lung cancer. Eur J Oncol Nurs 17(4):449–464. https://doi.org/10.1016/j.ejon.2012.10.013
Curt GA, Breitbart W, Cella D, Groopman JE, Horning SJ, Itri LM, Johnson DH, Miaskowski C, Scherr SL, Portenoy RK (2000) Impact of cancer-related fatigue on the lives of patients: new findings from the fatigue coalition. Oncologist 5(5):353–360
Tanaka K, Akechi T, Okuyama T, Nishiwaki Y, Uchitomi Y (2002) Impact of dyspnea, pain, and fatigue on daily life activities in ambulatory patients with advanced lung cancer. JPSM 23(5):417–423. https://doi.org/10.1016/S0885-3924(02)00376-7
Wilson KG, Curran D, McPherson CJ (2005) A burden to others: a common source of distress for the terminally ill. Cogn Behav Ther 34(2):115–123. https://doi.org/10.1080/16506070510008461
Lofaso CR, Weigand DA (2014) Individual characteristics and self-perceived burden in cancer patients. Curr Psychol 33(2):174–184. https://doi.org/10.1007/s12144-014-9204-y
Snyder CR, Harris C, Anderson JR, Holleran SA, Irving LM, Sigmon ST, Yoshinobu L, Gibb J, Langelle C, Harney P (1991) The will and the ways: development and validation of an individual-differences measure of hope. J Pers Soc Psychol 60(4):570–585
Snyder CR, Sympson SC, Ybasco FC, Borders TF, Babyak MA, Higgins RL (1996) Development and validation of the State Hope Scale. J Pers Soc Psychol 70(2):321–335
Cheavens JS, Heiy JE, Feldman DB, Benitez C, Rand KL (2019) Hope, goals, and pathways: Further validating the Hope Scale with observer ratings. J Posit Psychol 14(4):452–462
Gum A, Snyder C (2002) Coping with terminal illness: the role of hopeful thinking. J Palliat Med 5(6):883–894. https://doi.org/10.1089/10966210260499078
Goldzweig G, Baider L, Andritsch E, Pfeffer R, Rottenberg Y (2017) A dialogue of depression and hope: elderly patients diagnosed with cancer and their spousal caregivers. J Cancer Educ 32(3):549–555. https://doi.org/10.1007/s13187-015-0975-0
Peh CX, Liu J, Bishop GD, Chan HY, Chua SM, Kua EH, Mahendran R (2016) Emotion regulation and emotional distress: the mediating role of hope on reappraisal and anxiety/depression in newly diagnosed cancer patients. Psycho-oncology 26(8):1191–1197. https://doi.org/10.1002/pon.4297
Schofield PE, Stockler MR, Zannino D, Tebbutt NC, Price TJ, Simes RJ, Wong N, Pavlakis N, Ransom D, Moylan E, Underhill C, Wyld D, Burns I, Ward R, Wilcken N, Jefford M (2016) Hope, optimism and survival in a randomised trial of chemotherapy for metastatic colorectal cancer. Support Care Cancer 24(1):401–408. https://doi.org/10.1007/s00520-015-2792-8
Rosenberg AR, Bradford MC, Bona K, Shaffer ML, Wolfe J, Baker KS, Lau N, Yi-Frazier J (2018) Hope, distress, and later quality of life among adolescent and young adults with cancer. J Psychosoc Oncol 36(2):137–144. https://doi.org/10.1080/07347332.2017.1382646
Berendes D, Keefe FJ, Somers TJ, Kothadia SM, Porter LS, Cheavens JS (2010) Hope in the context of lung cancer: relationships of hope to symptoms and psychological distress. JPSM 40(2):174–182. https://doi.org/10.1016/j.jpainsymman.2010.01.014
Fischer IC, Cripe LD, Rand KL (2018) Predicting symptoms of anxiety and depression in patients living with advanced cancer: the differential roles of hope and optimism. Support Care Cancer 26:3471–3477. https://doi.org/10.1007/s00520-018-4215-0. doi:10.1007/s00520-018-4215-0
Snyder CR (2002) Hope theory: rainbows in the mind. Psychol Inq 13(4):249–275. https://doi.org/10.1207/S15327965PLI1304_01
Rajandram RK, Ho SM, Samman N, Chan N, McGrath C, Zwahlen RA (2011) Interaction of hope and optimism with anxiety and depression in a specific group of cancer survivors: a preliminary study. BMC Res Notes 4(1):519. https://doi.org/10.1186/1756-0500-4-519
Southerland JL, Slawson DL, Pack R, Sörensen S, Lyness JM, Hirsch JK (2016) Trait hope and preparation for future care needs among older adult primary care patients. Clin Gerontol 39(2):117–126. https://doi.org/10.1080/07317115.2015.1120254
Cotton Bronk K, Hill PL, Lapsley DK, Talib TL, Finch H (2009) Purpose, hope, and life satisfaction in three age groups. J Posit Psychol 4(6):500–510. https://doi.org/10.1080/17439760903271439
Ho S, Rajandram RK, Chan N, Samman N, McGrath C, Zwahlen RA (2011) The roles of hope and optimism on posttraumatic growth in oral cavity cancer patients. Oral Oncol 47(2):121–124. https://doi.org/10.1016/j.oraloncology.2010.11.015
Steffen LE, Vowles KE, Smith BW, Gan GN, Edelman MJ (2018) Daily diary study of hope, stigma, and functioning in lung cancer patients. Health Psychol 37(3):218–227. https://doi.org/10.1037/hea0000570
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. JNCI 85(5):365–376
Lyons KD, Bakitas M, Hegel MT, Hanscom B, Hull J, Ahles TA (2009) Reliability and validity of the Functional Assessment of Chronic Illness Therapy-Palliative care (FACIT-Pal) scale. JPSM 37(1):23–32. https://doi.org/10.1016/j.jpainsymman.2007.12.015
Cella DF, Bonomi AE, Lloyd SR, Tulsky DS, Kaplan E, Bonomi P (1995) Reliability and validity of the Functional Assessment of cancer Therapy-Lung (FACT-L) quality of life instrument. Lung Cancer 12(3):199–220
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6):361–370
IBM (2016) IBM SPSS statistics for windows, version 24.0. IBM Corp., Armonk
Barta W, Tennen H, Litt M (2012) Measurement reactivity in diary research. In: Mehl MR, Conner TS (eds) Handbook of research methods for studying daily life. Guilford Press, New York, pp 108–123
Temel JS, Pirl WF, Lynch TJ (2006) Comprehensive symptom management in patients with advanced-stage non–small-cell lung cancer. Clin Lung Cancer 7(4):241–249. https://doi.org/10.3816/CLC.2006.n.001
Grealish L, Hyde MK, Legg M, Lazenby M, Aitken JF, Dunn J, Chambers SK (2019) Psychosocial predictors of hope two years after diagnosis of colorectal cancer: implications for nurse-led hope programmes. Eur J Cancer Care 0(0):e13010. https://doi.org/10.1111/ecc.13010
Lam WW, Yeo W, Suen J, Ho WM, Tsang J, Soong I, Yau TK, Wong KY, Sze WK, Ng AW, Kwong A, Suen D, Fong D, Ho S, Fielding R (2016) Goal adjustment influence on psychological well-being following advanced breast cancer diagnosis. Psycho-oncology 25(1):58–65. https://doi.org/10.1002/pon.3871
Thornton LM, Cheavens JS, Heitzmann CA, Dorfman CS, Wu SM, Andersen BL (2014) Test of mindfulness and hope components in a psychological intervention for women with cancer recurrence. JCCP 82(6):1087–1100. https://doi.org/10.1037/a0036959
Rosenberg A, Bradford M, Klein V, Etsekson N, Wharton C, Shaffer M, Yi-Frazier J (2018) The promoting resilience in stress management (PRISM) intervention for adolescents and young adults: a pilot randomized controlled trial (TH320A). JPSM 55(2):569–570. https://doi.org/10.1016/j.jpainsymman.2017.12.023
Cheavens JS, Feldman DB, Gum A, Michael ST, Snyder CR (2006) Hope therapy in a community sample: a pilot investigation. Soc Indic Res 77(1):61–78. https://doi.org/10.1007/s11205-005-5553-0
Jim HSL, Small B, Faul LA, Franzen J, Apte S, Jacobsen PB (2011) Fatigue, depression, sleep, and activity during chemotherapy: daily and intraday variation and relationships among symptom changes. Ann Behav Med 42(3):321–333. https://doi.org/10.1007/s12160-011-9294-9
Von Roenn JH, von Gunten CF (2003) Setting goals to maintain hope. J Clin Oncol 21(3):570–574
Boa S, Duncan EAS, Haraldsdottir E, Wyke S (2014) Goal setting in palliative care: a structured review. Prog Palliat Care 22(6):326–333. https://doi.org/10.1179/1743291X14Y.0000000097
Feudtner C (2005) Hope and the prospects of healing at the end of life. J Altern Complement Med 11(supplement 1):s-23–s-30. https://doi.org/10.1089/acm.2005.11.s-23
Funding
Laurie Steffen was supported by R25CA122061 (PI: Nancy Avis, Ph.D).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no competing interests. Dr. Vowles discloses grant funding from Pfizer Pharmaceuticals, outside the submitted work.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Dr. Steffen has full control of the primary data and agrees to allow the journal to review upon request.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Steffen, L.E., Cheavens, J.S., Vowles, K.E. et al. Hope-related goal cognitions and daily experiences of fatigue, pain, and functional concern among lung cancer patients. Support Care Cancer 28, 827–835 (2020). https://doi.org/10.1007/s00520-019-04878-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-04878-y