Abstract
Purpose
Patient preference is an essential component of patient-centered supportive cancer care; however, little is known about the factors that shape preference for treatment. This study sought to understand what factors may contribute to patient preference for two non-pharmacological interventions, acupuncture or cognitive behavioral therapy for insomnia (CBT-I).
Methods
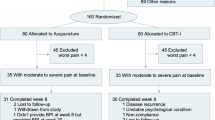
We conducted individual, open-ended, semi-structured interviews among cancer survivors who had completed active treatment and met the diagnostic criteria for insomnia disorder. Two forms of codes were used for analysis: a priori set of codes derived from the key ideas and a set of codes that emerged from the data.
Results
Among 53 participants, the median age was 60.7 (range 27–83), 30 participants (56.6%) were female, and 18 (34%) were non-white. We identified three themes that contributed to an individual’s treatment preference: perception of the treatment’s evidence base, experience with the treatment, and consideration of personal factors. Participants gave preference to the treatment perceived as having stronger evidence. Participants also reflected on positive or negative experiences with both of the interventions, counting their own experiences, as well as those of trusted sources. Lastly, participants considered their own unique circumstances and factors such as the amount of work involved, fit with personality, or fit with their “type” of insomnia.
Conclusions
Knowledge of the evidence base, past experience, and personal factors shaped patient preference regardless of whether they accurately represent the evidence. Acknowledging these salient factors may help inform patient-centered decision-making and care.

Similar content being viewed by others
References
Palesh OG, Roscoe JA, Mustian KM, Roth T, Savard J, Ancoli-Israel S, Heckler C, Purnell JQ, Janelsins MC, Morrow GR (2010) Prevalence, demographics, and psychological associations of sleep disruption in patients with cancer: University of Rochester Cancer Center-Community Clinical Oncology Program. J Clin Oncol 28(2):292–298. https://doi.org/10.1200/JCO.2009.22.5011
Savard J, Ivers H, Villa J, Caplette-Gingras A, Morin CM (2011) Natural course of insomnia comorbid with cancer: an 18-month longitudinal study. J Clin Oncol 29(26):3580–3586. https://doi.org/10.1200/JCO.2010.33.2247
Fiorentino L, Rissling M, Liu L, Ancoli-Israel S (2011) The symptom cluster of sleep, fatigue and depressive symptoms in breast cancer patients: severity of the problem and treatment options. Drug Discov Today Dis Models 8(4):167–173. https://doi.org/10.1016/j.ddmod.2011.05.001
Bower JE (2008) Behavioral symptoms in patients with breast cancer and survivors. J Clin Oncol 26(5):768–777. https://doi.org/10.1200/JCO.2007.14.3248
Bower JE, Ganz PA, Irwin MR, Kwan L, Breen EC, Cole SW (2011) Inflammation and behavioral symptoms after breast cancer treatment: do fatigue, depression, and sleep disturbance share a common underlying mechanism? J Clin Oncol 29(26):3517–3522. https://doi.org/10.1200/JCO.2011.36.1154
Van Onselen C, Cooper BA, Lee K, Dunn L, Aouizerat BE, West C, Dodd M, Paul S, Miaskowski C (2012) Identification of distinct subgroups of breast cancer patients based on self-reported changes in sleep disturbance. Support Care Cancer 20(10):2611–2619. https://doi.org/10.1007/s00520-012-1381-3
Colagiuri B, Christensen S, Jensen AB, Price MA, Butow PN, Zachariae R (2011) Prevalence and predictors of sleep difficulty in a national cohort of women with primary breast cancer three to four months postsurgery. J Pain Symptom Manag 42(5):710–720. https://doi.org/10.1016/j.jpainsymman.2011.02.012
Franzen PL, Buysse DJ (2008) Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci 10(4):473–481
Liu L, Fiorentino L, Rissling M, Natarajan L, Parker BA, Dimsdale JE, Mills PJ, Sadler GR, Ancoli-Israel S (2013) Decreased health-related quality of life in women with breast cancer is associated with poor sleep. Behav Sleep Med 11(3):189–206. https://doi.org/10.1080/15402002.2012.660589
Grutsch JF, Ferrans C, Wood PA, Du-Quiton J, Quiton DF, Reynolds JL, Ansell CM, Oh EY, Daehler MA, Levin RD, Braun DP, Gupta D, Lis CG, Hrushesky WJ (2011) The association of quality of life with potentially remediable disruptions of circadian sleep/activity rhythms in patients with advanced lung cancer. BMC Cancer 11(1):193. https://doi.org/10.1186/1471-2407-11-193
Mormont MC, Waterhouse J (2002) Contribution of the rest-activity circadian rhythm to quality of life in cancer patients. Chronobiol Int 19(1):313–323. https://doi.org/10.1081/CBI-120002606
Mormont MC, Waterhouse J, Bleuzen P, Giacchetti S, Jami A, Bogdan A, Lellouch J, Misset JL, Touitou Y, Levi F (2000) Marked 24-h rest/activity rhythms are associated with better quality of life, better response, and longer survival in patients with metastatic colorectal cancer and good performance status. Clin Cancer Res 6(8):3038–3045
Moore TA, Berger AM, Dizona P (2011) Sleep aid use during and following breast cancer adjuvant chemotherapy. Psychooncology 20(3):321–325. https://doi.org/10.1002/pon.1756
Kripke DF (2006) Risks of chronic hypnotic use. In: Lader M, Cardinali DP, Pandi-Perumal SR (eds) Sleep and sleep disorders: a neuropsychopharmacological approach. Springer Science, Berlin, pp 141–145. https://doi.org/10.1007/0-387-27682-3_15
Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD, Clinical Guidelines Committee of the American College of Physicians (2016) Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med 165(2):125–133. https://doi.org/10.7326/M15-2175
Llewellyn CD, Horney DJ, McGurk M, Weinman J, Herold J, Altman K, Smith HE (2011) Assessing the psychological predictors of benefit finding in patients with head and neck cancer. Psychooncology 22:97–105
Preference Collaborative Review Group (2008) Patients’ preferences within randomised trials: systematic review and patient level meta-analysis. BMJ 337(oct31 1):a1864. https://doi.org/10.1136/bmj.a1864
Choi TY, Kim JI, Lim HJ, Lee MS (2017) Acupuncture for managing cancer-related insomnia: a systematic review of randomized clinical trials. Integr Cancer Ther 16(2):135–146. https://doi.org/10.1177/1534735416664172
Yun H, Sun L, Mao JJ (2017) Growth of integrative medicine at leading cancer centers between 2009 and 2016: a systematic analysis of NCI-designated comprehensive cancer center websites. J Natl Cancer Inst Monogr 2017(52). https://doi.org/10.1093/jncimonographs/lgx004
Johnson JA, Rash JA, Campbell TS, Savard J, Gehrman PR, Perlis M, Carlson LE, Garland SN (2015) A systematic review and meta-analysis of randomized controlled trials of cognitive behavior therapy for insomnia (CBT-I) in cancer survivors. Sleep Med Rev 27:20–28
Matthews EE, Arnedt JT, McCarthy MS, Cuddihy LJ, Aloia MS (2013) Adherence to cognitive behavioral therapy for insomnia: a systematic review. Sleep Med Rev 17(6):453–464. https://doi.org/10.1016/j.smrv.2013.01.001
Ong JC, Kuo TF, Manber R (2008) Who is at risk for dropout from group cognitive-behavior therapy for insomnia? J Psychosom Res 64(4):419–425. https://doi.org/10.1016/j.jpsychores.2007.10.009
Lu W, Dean-Clower E, Doherty-Gilman A, Rosenthal DS (2008) The value of acupuncture in cancer care. Hematol Oncol Clin North Am 22(4):631–648, viii. https://doi.org/10.1016/j.hoc.2008.04.005
Zhao K (2013) Acupuncture for the treatment of insomnia. Int Rev Neurobiol 111:217–234. https://doi.org/10.1016/B978-0-12-411545-3.00011-0
Yeung WF, Chung KF, Zhang SP, Yap TG, Law AC (2009) Electroacupuncture for primary insomnia: a randomized controlled trial. Sleep 32(8):1039–1047. https://doi.org/10.1093/sleep/32.8.1039
Yeung WF, Chung KF, Leung YK, Zhang SP, Law AC (2009) Traditional needle acupuncture treatment for insomnia: a systematic review of randomized controlled trials. Sleep Med 10(7):694–704. https://doi.org/10.1016/j.sleep.2008.08.012
Ruan JW, Wang CH, Liao XX, Yan YS, Hu YH, Rao ZD, Wen M, Zeng XX, Lai XS (2009) Electroacupuncture treatment of chronic insomniacs. Chin Med J 122(23):2869–2873
Cheuk DK, Yeung WF, Chung KF, Wong V (2012) Acupuncture for insomnia. Cochrane Database Syst Rev 9:CD005472
Ernst E, Lee MS, Choi TY (2011) Acupuncture for insomnia? An overview of systematic reviews. Eur J Gen Pract 17(2):116–123. https://doi.org/10.3109/13814788.2011.568475
Cao H, Pan X, Li H, Liu J (2009) Acupuncture for treatment of insomnia: a systematic review of randomized controlled trials. J Altern Complement Med 15(11):1171–1186. https://doi.org/10.1089/acm.2009.0041
Garland SN, Gehrman P, Barg FK, Xie SX, Mao JJ (2016) CHoosing Options for Insomnia in Cancer Effectively (CHOICE): design of a patient centered comparative effectiveness trial of acupuncture and cognitive behavior therapy for insomnia. Contemp Clin Trials 47:349–355. https://doi.org/10.1016/j.cct.2016.02.010
Sidani S, Epstein DR, Bootzin RR, Moritz P, Miranda J (2009) Assessment of preferences for treatment: validation of a measure. Res Nurs Health 32(4):419–431. https://doi.org/10.1002/nur.20329
Curry LA, Nembhard IM, Bradley EH (2009) Qualitative and mixed methods provide unique contributions to outcomes research. Circulation 119(10):1442–1452. https://doi.org/10.1161/CIRCULATIONAHA.107.742775
Morgenthaler T, Kramer M, Alessi C, Friedman L, Boehlecke B, Brown T, Coleman J, Kapur V, Lee-Chiong T, Owens J, Pancer J, Swick T, American Academy of Sleep Medicine (2006) Practice parameters for the psychological and behavioral treatment of insomnia: an update. An American Academy of Sleep Medicine report. Sleep 29(11):1415–1419
Berger AM, Matthews EE, Kenkel AM (2017) Management of sleep-wake disturbances comorbid with cancer. Oncology (Williston Park) 31(8):610–617
Denberg TD, Melhado TV, Steiner JF (2006) Patient treatment preferences in localized prostate carcinoma: the influence of emotion, misconception, and anecdote. Cancer 107(3):620–630. https://doi.org/10.1002/cncr.22033
Shirk JD, Crespi CM, Saucedo JD, Lambrechts S, Dahan E, Kaplan R, Saigal C (2017) Does patient preference measurement in decision aids improve decisional conflict? A randomized trial in men with prostate cancer. Patient. https://doi.org/10.1007/s40271-017-0255-7
Schmidt K, Damm K, Prenzler A, Golpon H, Welte T (2016) Preferences of lung cancer patients for treatment and decision-making: a systematic literature review. Eur J Cancer Care (Engl) 25(4):580–591. https://doi.org/10.1111/ecc.12425
Hamelinck VC, Bastiaannet E, Pieterse AH, Jannink I, van de Velde CJ, Liefers GJ, Stiggelbout AM (2014) Patients’ preferences for surgical and adjuvant systemic treatment in early breast cancer: a systematic review. Cancer Treat Rev 40(8):1005–1018. https://doi.org/10.1016/j.ctrv.2014.06.007
Williams R, Farquharson L, Palmer L, Bassett P, Clarke J, Clark DM, Crawford MJ (2016) Patient preference in psychological treatment and associations with self-reported outcome: national cross-sectional survey in England and Wales. BMC Psychiatry 16(1):4. https://doi.org/10.1186/s12888-015-0702-8
Scherr KA, Fagerlin A, Hofer T, Scherer LD, Holmes-Rovner M, Williamson LD, Kahn VC, Montgomery JS, Greene KL, Zhang B, Ubel PA (2017) Physician recommendations trump patient preferences in prostate cancer treatment decisions. Med Decis Mak 37(1):56–69. https://doi.org/10.1177/0272989X16662841
Carlson LE, Tamagawa R, Stephen J, Doll R, Faris P, Dirkse D, Speca M (2014) Tailoring mind-body therapies to individual needs: patients’ program preference and psychological traits as moderators of the effects of mindfulness-based cancer recovery and supportive-expressive therapy in distressed breast cancer survivors. J Natl Cancer Inst Monogr 2014(50):308–314. https://doi.org/10.1093/jncimonographs/lgu034
Shingler SL, Bennett BM, Cramer JA, Towse A, Twelves C, Lloyd AJ (2014) Treatment preference, adherence and outcomes in patients with cancer: literature review and development of a theoretical model. Curr Med Res Opin 30(11):2329–2341. https://doi.org/10.1185/03007995.2014.952715
Acknowledgements
Research reported in this article was funded through a Patient-Centered Outcomes Research Institute (PCORI) Award (CER-1403-14292). This manuscript is also supported in part by a grant from the National Institutes of Health/National Cancer Institute Cancer Center (P30 CA008748). The statements presented in this article are solely the responsibility of the author(s) and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology Committee. Sincere thanks go to the CHOICE Study Patient Advisory Board members (Bill Barbour, Winifred Chain, Linda Geiger, Donna-Lee Lista, Jodi MacLeod, Alice McAllister, Hilma Maitland, and Edward Wolff), the participants, and clinical staff for their support of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This research was supported by the sources acknowledged above. The funders had no part in the collection, analysis, or interpretation of the data. The corresponding author has full control of all primary data and we agree to allow the journal to review this data if requested.
Rights and permissions
About this article
Cite this article
Garland, S.N., Eriksen, W., Song, S. et al. Factors that shape preference for acupuncture or cognitive behavioral therapy for the treatment of insomnia in cancer patients. Support Care Cancer 26, 2407–2415 (2018). https://doi.org/10.1007/s00520-018-4086-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4086-4