Abstract
Background
Hypoalbuminemia is a strong predictor of hospitalization and mortality among adult dialysis patients. However, data are scant on the association between serum albumin and hospitalization among children new to dialysis.
Methods
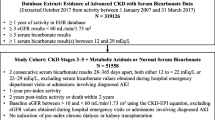
In a retrospective cohort study of children 1–17 years old with end-stage renal disease receiving dialysis therapy in a large US dialysis organization 2007–2011, we examined the association of serum albumin with hospitalization frequency and total hospitalization days using a negative binomial regression model.
Results
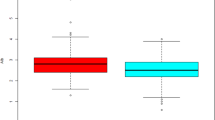
Among 416 eligible patients, median (interquartile range) age was 14 (10–16) years and mean ± SD baseline serum albumin level was 3.7 ± 0.8 g/dL. Two hundred sixty-six patients (64%) were hospitalized during follow-up with an incidence rate of 2.2 (95%CI, 1.9–2.4) admissions per patient-year. There was a U-shaped association between serum albumin and hospitalization frequency; hospitalization rates (95%CI) were 2.7 (2.2–3.2), 1.9 (1.5–2.4), 1.6 (1.3–1.9), and 2.7 (1.7–3.6) per patient-year among patients with serum albumin levels < 3.5, 3.5– < 4.0, 4.0– < 4.5, and ≥ 4.5 g/dL, respectively. Case mix-adjusted hospitalization incidence rate ratios (IRRs) (95%CI) were 1.63 (1.24–2.13), 1.32 (1.10–1.58), and 1.25 (1.06–1.49) at serum albumin levels 3.0, 3.5, and 4.5 g/dL, respectively (reference: 4.0 g/dL). Similar trends were observed in hospitalization days. These associations remained robust against further adjustment for laboratory variables associated with malnutrition and inflammation.
Conclusions
Both high and low serum albumin were associated with higher hospitalization in children starting dialysis. Because the observed association is novel and not fully explainable especially for high serum albumin levels, interpreting the results requires caution and further studies are needed to confirm and elucidate this association before clinical recommendations are made.






Similar content being viewed by others
References
Kalantar-Zadeh K, Cano NJ, Budde K, Chazot C, Kovesdy CP, Mak RH, Mehrotra R, Raj DS, Sehgal AR, Stenvinkel P, Ikizler TA (2011) Diets and enteral supplements for improving outcomes in chronic kidney disease. Nat Rev Nephrol 7:369–384. https://doi.org/10.1038/nrneph.2011.60
Fouque D, Kalantar-Zadeh K, Kopple J, Cano N, Chauveau P, Cuppari L, Franch H, Guarnieri G, Ikizler TA, Kaysen G, Lindholm B, Massy Z, Mitch W, Pineda E, Stenvinkel P, Trevino-Becerra A, Wanner C (2008) A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int 73:391–398. https://doi.org/10.1038/sj.ki.5002585
Ikizler TA, Cano NJ, Franch H, Fouque D, Himmelfarb J, Kalantar-Zadeh K, Kuhlmann MK, Stenvinkel P, TerWee P, Teta D, Wang AY, Wanner C, International Society of Renal Nutrition and Metabolism (2013) Prevention and treatment of protein energy wasting in chronic kidney disease patients: a consensus statement by the International Society of Renal Nutrition and Metabolism. Kidney Int 84:1096–1107. https://doi.org/10.1038/ki.2013.147
Rees L, Mak RH (2011) Nutrition and growth in children with chronic kidney disease. Nat Rev Nephrol 7:615–623. https://doi.org/10.1038/nrneph.2011.137
Silverstein DM (2009) Inflammation in chronic kidney disease: role in the progression of renal and cardiovascular disease. Pediatr Nephrol 24:1445–1452. https://doi.org/10.1007/s00467-008-1046-0
Tu J, Cheung WW, Mak RH (2016) Inflammation and nutrition in children with chronic kidney disease. World J Nephrol 5:274–282. https://doi.org/10.5527/wjn.v5.i3.274
Palmer SC, Maggo JK, Campbell KL, Craig JC, Johnson DW, Sutanto B, Ruospo M, Tong A, Strippoli GF (2017) Dietary interventions for adults with chronic kidney disease. Cochrane Database Syst Rev (4):CD011998. https://doi.org/10.1002/14651858.CD011998.pub2
Canada-USA (CANUSA) Peritoneal Dialysis Study Group (1996) Adequacy of dialysis and nutrition in continuous peritoneal dialysis: association with clinical outcomes. J Am Soc Nephrol 7:198–207
Combe C, Chauveau P, Laville M, Fouque D, Azar R, Cano N, Canaud B, Roth H, Leverve X, Aparicio M (2001) Influence of nutritional factors and hemodialysis adequacy on the survival of 1,610 French patients. Am J Kidney Dis 37:81–88. https://doi.org/10.1053/ajkd.2001.20756
Rees L (2015) 3.21 nutritional management in children with chronic kidney disease. World Rev Nutr Diet 113:254–258. https://doi.org/10.1159/000360347
Ku E, Fine RN, Hsu CY, McCulloch C, Glidden DV, Grimes B, Johansen KL (2016) Height at first RRT and mortality in children. Clin J Am Soc Nephrol 11:832–839. https://doi.org/10.2215/CJN.08250815
Furth SL, Stablein D, Fine RN, Powe NR, Fivush BA (2002) Adverse clinical outcomes associated with short stature at dialysis initiation: a report of the north American pediatric Renal transplant cooperative study. Pediatrics 109:909–913
Furth SL, Hwang W, Yang C, Neu AM, Fivush BA, Powe NR (2002) Growth failure, risk of hospitalization and death for children with end-stage renal disease. Pediatr Nephrol 17:450–455. https://doi.org/10.1007/s00467-002-0838-x
Ku E, Glidden DV, Hsu CY, Portale AA, Grimes B, Johansen KL (2016) Association of body mass index with patient-centered outcomes in children with ESRD. J Am Soc Nephrol 27:551–558. https://doi.org/10.1681/ASN.2015010008
Iseki K, Uehara H, Nishime K, Tokuyama K, Yoshihara K, Kinjo K, Shiohira Y, Fukiyama K (1996) Impact of the initial levels of laboratory variables on survival in chronic dialysis patients. Am J Kidney Dis 28:541–548
Kalantar-Zadeh K, Supasyndh O, Lehn RS, McAllister CJ, Kopple JD (2003) Normalized protein nitrogen appearance is correlated with hospitalization and mortality in hemodialysis patients with Kt/V greater than 1.20. J Ren Nutr 13:15–25. https://doi.org/10.1053/jren.2003.50005
Wong CS, Hingorani S, Gillen DL, Sherrard DJ, Watkins SL, Brandt JR, Ball A, Stehman-Breen CO (2002) Hypoalbuminemia and risk of death in pediatric patients with end-stage renal disease. Kidney Int 61:630–637. https://doi.org/10.1046/j.1523-1755.2002.00169.x
Amaral S, Hwang W, Fivush B, Neu A, Frankenfield D, Furth S (2008) Serum albumin level and risk for mortality and hospitalization in adolescents on hemodialysis. Clin J Am Soc Nephrol 3:759–767. https://doi.org/10.2215/CJN.02720707
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, de Ferranti SD, Dionne JM, Falkner B, Flinn SK, Gidding SS, Goodwin C, Leu MG, Powers ME, Rea C, Samuels J, Simasek M, Thaker VV, Urbina EM (2017) Subcommittee on screening and management of high blood pressure in children clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140:e20171904. https://doi.org/10.1542/peds.2017-1904
Greenland S (1995) Dose-response and trend analysis in epidemiology: alternatives to categorical analysis. Epidemiology 6:356–365
Barstow C, Rerucha C (2015) Evaluation of short and tall stature in children. Am Fam Physician 92:43–50
Lacson E Jr, Wang W, Hakim RM, Teng M, Lazarus JM (2009) Associates of mortality and hospitalization in hemodialysis: potentially actionable laboratory variables and vascular access. Am J Kidney Dis 53:79–90. https://doi.org/10.1053/j.ajkd.2008.07.031
Dalrymple LS, Mu Y, Romano PS, Nguyen DV, Chertow GM, Delgado C, Grimes B, Kaysen GA, Johansen KL (2015) Outcomes of infection-related hospitalization in Medicare beneficiaries receiving in-center hemodialysis. Am J Kidney Dis 65:754–762. https://doi.org/10.1053/j.ajkd.2014.11.030
Bennette C, Vickers A (2012) Against quantiles: categorization of continuous variables in epidemiologic research, and its discontents. BMC Med Res Methodol 12:21. https://doi.org/10.1186/1471-2288-12-21
US Renal Data System (2016) Annual Data Report: Epidemiology of Kidney Disease in the United States (2017). Am J Kidney Dis 69:A4. https://doi.org/10.1053/j.ajkd.2017.01.036
Abraham AG, Mak RH, Mitsnefes M, White C, Moxey-Mims M, Warady B, Furth SL (2014) Protein energy wasting in children with chronic kidney disease. Pediatr Nephrol 29:1231–1238. https://doi.org/10.1007/s00467-014-2768-9
Wong CS, Gipson DS, Gillen DL, Emerson S, Koepsell T, Sherrard DJ, Watkins SL, Stehman-Breen C (2000) Anthropometric measures and risk of death in children with end-stage renal disease. Am J Kidney Dis 36:811–819. https://doi.org/10.1053/ajkd.2000.17674
Friedman AN, Fadem SZ (2010) Reassessment of albumin as a nutritional marker in kidney disease. J Am Soc Nephrol 21:223–230. https://doi.org/10.1681/ASN.2009020213
Sabatino A, Regolisti G, Karupaiah T, Sahathevan S, Sadu Singh BK, Khor BH, Salhab N, Karavetian M, Cupisti A, Fiaccadori E (2017) Protein-energy wasting and nutritional supplementation in patients with end-stage renal disease on hemodialysis. Clin Nutr 36:663–671. https://doi.org/10.1016/j.clnu.2016.06.007
Kalantar-Zadeh K, Ikizler TA, Block G, Avram MM, Kopple JD (2003) Malnutrition-inflammation complex syndrome in dialysis patients: causes and consequences. Am J Kidney Dis 42:864–881
Fischbach M, Edefonti A, Schroder C, Watson A, European Pediatric Dialysis Working Group (2005) Hemodialysis in children: general practical guidelines. Pediatr Nephrol 20:1054–1066. https://doi.org/10.1007/s00467-005-1876-y
Rees L, Jones H (2013) Nutritional management and growth in children with chronic kidney disease. Pediatr Nephrol 28:527–536. https://doi.org/10.1007/s00467-012-2258-x
Acknowledgements
We thank Da Vita Clinical Research for providing statistically de-identified clinical data for this research.
Funding
The authors are supported by the research grants from the NIH/NIDDK including T32-DK104687 (M.L.), K23-DK102903 (C.M.R), R03-DK114642 (C.M.R), K24-DK091419 (K.K.-Z), U01-DK102163 (K.K.-Z), and philanthropist grants from H. Simmons, L. Chang and J. Lee.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the Institutional Review Boards of the Los Angeles Biomedical Research Institute at Harbor-University of California Los Angeles, University of California Irvine Medical Center, and the University of Washington as exempt from informed consent.
Conflict of interest
K.K.-Z. has received honoraria and/or support from Abbott, Abbvie, Alexion, Amgen, American Society of Nephrology, Astra-Zeneca, AVEO Oncology, Chugai, DaVita, Fresenius, Genentech, Haymarket Media, Hofstra Medical School, International Federation of Kidney Foundations, International Society of Hemodialysis, International Society of Renal Nutrition and Metabolism, Japanese Society of Dialysis Therapy, Hospira, Kabi, Keryx, Novartis, National Institutes of Health, National Kidney Foundation, OPKO, Pfizer, Relypsa, Resverlogix, Sandoz, Sanofi, Shire, Vifor, UpToDate, and ZSPharma.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 272 kb)
Rights and permissions
About this article
Cite this article
Okuda, Y., Obi, Y., Streja, E. et al. Serum albumin and hospitalization among pediatric patients with end-stage renal disease who started dialysis therapy. Pediatr Nephrol 34, 1799–1809 (2019). https://doi.org/10.1007/s00467-019-04270-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-019-04270-2