Abstract
Background
Intestinal malrotation results from errors in fetal intestinal rotation and fixation. While most patients are diagnosed in childhood, some present as adults. Laparoscopic Ladd’s procedure is an accepted alternative to laparotomy in children but has not been well-studied in adults. This study was designed to investigate outcomes for adults undergoing laparoscopic Ladd’s repair for malrotation.
Methods
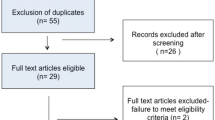
We performed a single-institution retrospective chart review over 11 years. Data collected included patient age, details of pre-operative work-up and diagnosis, surgical management, complications, rates of re-operation, and symptom resolution. Patients were evaluated on an intent-to-treat basis based on their planned operative approach. Categorical data were analyzed using Fisher’s exact test. Continuous data were analyzed using Student’s t test.
Results
Twenty-two patients were identified (age range 18–63). Fifteen were diagnosed pre-operatively; of the remaining seven patients, four received an intra-operative malrotation diagnosis during elective surgery for another problem. Most had some type of pre-operative imaging, with computed tomography being the most common (77.3 %). Comparing patients on an intent-to-treat basis, the two groups were similar with respect to age, operative time, and estimated blood loss. Six patients underwent successful laparoscopic repair; three began laparoscopically but were converted to laparotomy. There was a statistically significant difference in hospital length of stay (LOS) (5.0 ± 2.5 days vs 11.6 ± 8.1 days, p = 0.0148) favoring the laparoscopic approach. Three patients required re-operation: two underwent side-to-side duodeno-duodenostomy and one underwent a re-do Ladd’s procedure. Ultimately, three (two laparoscopic, one open) had persistent symptoms of bloating (n = 2), constipation (n = 2), and/or pain (n = 1).
Conclusion
Laparoscopic repair appears to be safe and effective in adults. While a small sample size limits the power of this study, we found a statistically significant decrease in LOS and a trend toward decreased postoperative nasogastric decompression. There were no significant differences in complication rates, re-operation, or persistence of symptoms between groups.

Similar content being viewed by others
References
Sato TT and Oldham KT (2011) Pediatric abdomen. In: Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Simeone DM, Upchurch GR Jr (eds) Editors Greenfield’s surgery scientific principles and practice, Wolters Kluwer Health/Lippincott Williams & Wilkins, Philadelphia
Ladd WE (1936) Surgical diseases of the alimentary tract in infants. N Engl J Med 215:705–708
Bass KD, Rothenberg SS, Change JHT (1998) Laparoscopic Ladd’s procedure in infants with malrotation. J Pediatr Surg 33:279–281
Mazziotti MV, Strasberg SM, Langer JC (1997) intestinal rotation abnormalities without volvulus: the role of laparoscopy. J Am Coll Surg 185:172–176
Nehra D, Goldstein AM (2011) Intestinal malrotation: varied clinical presentation from infancy through adulthood. Surgery 149:386–393
Durkin ET, Lund DP, Shaaban AF, Schurr MJ, Weber SM (2008) Age-related differences in diagnosis and morbidity of intestinal malrotation. J Am Coll Surg 206:658–663
Parker J, Reid G, Wong F (1999) Microlaparoscopic left upper quadrant entry in patients at high risk of periumbilical adhesions. Aust N Z J Obstet Gynaecol 39:88–92
Tittel A, Treutner KH, Titkova S, Ottinger A, Schumpelick V (2001) Comparison of adhesion reformation after laparoscoic and conventional adhesiolysis in an animal model. Lengenbeck’s Arch Surg 386:141–145
Garrard CL, Clements RH, Nanney L, Davidson JM, Richards WO (1999) Adhesion formation is reduced after laparoscopic surgery. Surg Endosc 13:10–13
Krahenbuhl L, Schafer M, Kuzinkovas V, Renzulli P, Baer HU, Buchler MW (1998) Experimental study of adhesion formation in open and laparoscopic fundoplication. Br J Surg 85:826–830
Polymeneas G, Theodosopoulos T, Stamatiadis A, Kourias E (2001) A comparative study of postoperative adhesion formation after laparoscopic vs open cholecystectomy. Surg Endosc 15:41–43
Hull TL, Joyce MR, Geisler DP, Coffey JC (2012) Adhesions after laparoscopic and open ileal pouch-anal anastomosis surgery for ulcerative colitis. Br J Surg 99:270–275
Liang JT, Huang KC, Lai HS, Lee PH, Jeng YM (2007) Oncologic results of laparoscopic versus conventional open surgery for stage II or III left-sided colon cancers: a randomized controlled trial. Ann Surg Oncol 14:109–117
Klarenbeek BR, Bergamaschi R, Veenhof AAFA, van der Peet DL, van den Broek WT, de Lange ESM, Bemelman WA, Heres P, Lacy AM, Cuesta MA (2011) Laparoscopic versus open sigmoid resection for diverticular disease: follow-up assessment of the randomized control Sigma trial. Surg Endosc 25:1121–1126
Polle SW, Dunker MS, Slors JF, Sprangers MA, Cuesta MA, Gouma DJ, Bemelman WA (2007) Body image, cosmesis, quality of life, and functional outcome of hand-assisted laparoscopic versus open restorative proctocolectomy: long-term results of randomized trial. Surg Endosc 21:1301–1307
Chan KL, Hui WC, Tam PK (2005) Prospective randomized single-center, single-blind comparison of laparoscopic vs open repair of pediatric inguinal hernia. Surg Endosc 19:927–932
Vignali A, De Nardi P, Ghirardelli L, De Palo S, Staudacher C (2013) Short and long-term outcomes of laparoscopic colectomy in obese patients. World J Gastroenterol 19:7405–7411
Matzke GM, Dozois EJ, Larson DW, Moir CR (2005) Surgical management of intestinal malrotation in adults: comparative results for open and laparoscopic Ladd procedures. Surg Endosc 19:1416–1419
Ferzli G, Shapiro K, Chaudry G, Patel S (2004) Laparoscopic extraperitoneal approach to acutely incarcerated inguinal hernia. Surg Endosc 18:228–231
Hoffman A, Leshem E, Zmora O, Nachtomi O, Shabtai M, Ayalon A, Rosin D (2010) The combined laparoscopic approach for the treatment of incarcerated inguinal hernia. Surg Endosc 24:1815–1818
Yang GPC, Chan CTY, Lai ECH, Chan OCY, Tang CN, Li MKW (2012) Laparoscopic versus open repair for strangulated groin hernias: 188 cases over 4 years. Asian J Endosc Surg 5:131–137
Levard H, Boudet M-J, Msika S, Molkhou J-M, Hay J-M, Laborde Y, Gillet M, Fingerhut A (2001) Laparoscopic treatment of acute small bowel obstruction: a multicentre retrospective study. Aust N Z J Obstet Gynaecol 71:641–646
O’Connor DB, Winter DC (2012) The role of laparoscopy in the management of acute small-bowel obstruction: a review of over 2,000 cases. Surg Endosc 26:12–17
Suter M, Zermatten P, Halkic N, Martinet O, Bettschart B (2000) Laparoscopic management of mechanical small bowel obstruction. Are there predictors of success or failure? Surg Endosc 14:478–1183
Turley RS, Barbas AS, Lidsky ME, Mantyh CR, Migaly J, Scarborough JE (2013) Laparoscopic versus open Hartmann procedure for the emergency treatment of diverticulitis: a propensity-matched analysis. Dis Colon Rectum 56:72–82
Acknowledgments
Author Lane Frasier is currently funded under F32 Grant HS022403 through the Agency for Healthcare Research and Quality and the AAS Research Fellowship Award and previously received funding via T32 Grant CA90217 through the NIH National Cancer Institute. Ankush Gosain is funded by the American Pediatric Surgery Association Foundation Award (2013) and NIDDK K08DK098271. This work was supported by grants from NIH, National Cancer Institute; T32 CA90217, F32 HS022403, AAS Research Fellowship Award and K08 (NIDDK K08DK098271).
Disclosures
Dr. Greenberg is a paid consultant for Bard-Davol and Covidien; neither of these relationships are relevant to the content of this manuscript. Authors Frasier, Leverson, and Gosain have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Frasier, L.L., Leverson, G., Gosain, A. et al. Laparoscopic versus open Ladd’s procedure for intestinal malrotation in adults. Surg Endosc 29, 1598–1604 (2015). https://doi.org/10.1007/s00464-014-3849-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3849-3